YES.
Kuzhel, G.V. Matyushin, T.D. Fedorova E.A., Savchenko, T.M. Zadoenko KGUZ "Krasnoyarsk Regional Hospital No. 2" GOUVPO "Krasnoyarsk State Medical Academy"
An electrocardiogram in 12 standard leads is the method of choice in the diagnosis of acute myocardial infarction (AMI). Quick and accurate diagnosis of AMI is vital, as it makes it possible to immediately begin reperfusion therapy, which reduces the area of necrosis and improves the patient's prognosis. One of the generally accepted criteria for myocardial infarction is ST segment elevation in two or more anatomically adjacent leads [10]. The importance of timely identification of ST segment elevation associated with AMI is emphasized by the fact that neither ST segment depression nor increased biochemical markers of cardiac necrosis (MCN) in the blood serum are indications for thrombolytic therapy [4, 9].
In the early stages of AMI, diagnosis can be significantly difficult, since the ECG is often normal or has minimal abnormalities. Moreover, only half of patients with AMI have obvious diagnostic changes on the first ECG. At the same time, approximately 10% of patients with proven AMI (based on clinical data and positive MCI) will not develop typical changes on the ECG, such as ST segment elevation or depression [4]. However, in most cases, serial ECGs in individuals with AMI show a characteristic evolution that usually corresponds to the typical changes observed in myocardial infarction. In the domestic school of cardiology, it is customary to distinguish four stages of the course of AMI [1].
I.
The most acute stage
. In this stage, which lasts from several hours to several days, changes in the ECG affect only the ST segment and the T wave. The earliest signs of acute myocardial infarction are difficult to distinguish and usually include an increase in the amplitude of the T wave in the affected area, which becomes symmetrical and directional ( hyperacute). Typically, hyperacute T waves are most evident in the anterior precordial leads and are most noticeable when an older ECG is available for comparison. Changes in T wave amplitude can be observed within a few minutes of the onset of infarction and are accompanied by corresponding changes in the ST segment. The optimal time for delivery of a patient to a medical facility is considered to be an interval of up to four hours from the onset of AMI. Unfortunately, ECG changes in the acute stage of myocardial infarction are often not properly assessed, which significantly increases the time it takes for the patient to be delivered to a specialized facility and prolongs the start of reperfusion therapy.
II. Acute stage.
In the acute stage, which usually lasts up to one week, ST segment elevation is recorded and Q waves begin to form. In practice, ST segment elevation is often the earliest sign of AMI and usually becomes noticeable within a few hours from the onset of symptoms. At the initial stages, the angle between the T wave and the ST segment, characteristic of a normal ECG, is lost. The T wave becomes wide and the ST segment rises, losing its normal concavity. During further ascent, the ST segment becomes convex upward. The degree of ST segment elevation varies between small changes of less than 1 mm to pronounced elevation of more than 10 mm. Sometimes the QRS complex, ST segment and T wave merge, forming the so-called monophasic curve.
III. Subacute stage.
The subacute stage of myocardial infarction lasts up to several weeks. During this stage, the ST segment begins to approach the isoline, and negative T waves are formed. In the case of transmural myocardial infarction, the necrosis process is accompanied by changes in the QRS complex, which include a decrease in the amplitude of the R waves and the development of pathological Q waves. Such changes develop as a result of the loss of viable myocardium under recording electrode, therefore Q waves are the only ECG criterion that verifies myocardial necrosis. Q waves can develop within 1 to 2 hours of the onset of AMI symptoms, although this often takes 12 to 24 hours. The presence of pathological Q waves, however, does not necessarily indicate a completed infarction. If ST segment elevation and Q waves are detected on the ECG and the chest pain is of recent onset, the patient may still benefit from thrombolysis or interventional therapy.
IV. Scar stage.
Consolidation of scar tissue ends on average 8 weeks after myocardial infarction. At this stage, the ST segment reverts to the isoline and the amplitude of negative T waves decreases. In the case of extensive myocardial infarction, pathological Q waves are a stable marker of cardiac necrosis. In small infarcts, scar tissue may include viable myocardium, which may reduce the size of the electrically inert region and even cause the eventual disappearance of Q waves.
One of the curious features of the ECG in AMI is the so-called pseudonormalization phenomenon. Wilson's theory of the formation of Q waves implies the formation of a so-called electrical window in case of necrosis, through which the recording electrode records the electrical potentials of the opposite wall. However, despite necrosis, some of the myocardial fibers in the infarction zone remain viable, which explains the characteristic flattening of Q waves during myocardial infarction. However, the potentials of these fibers remain hidden behind the powerful electric vector of the opposite wall. With a repeated infarction, which involves the opposite wall, this vector is significantly reduced, which, in turn, makes it possible to record the potentials of myocardial fibers in the area of the old scar. As a result, in the area of the old scar with pathological Q waves (for example, in the anterior wall), in the event of a re-infarction of the opposite wall (for example, the posterior wall), R waves begin to be recorded. Thus, the registration of R waves in the area where pathological Q waves were previously observed, strongly suggests the formation of an infarction in the opposite wall.
Dynamics of changes in the ST segment and T wave in AMI
The ECG picture during myocardial infarction has its own characteristic development. Firstly, ST segment elevation, as a rule, leads to the formation of Q waves. Secondly, the formation of negative T waves occurs against the background of a characteristic arcuate ST segment elevation.
ST segment elevation associated with myocardial infarction in the anterior wall can persist for a long time if dyskinesia or left ventricular (LV) aneurysm develops. Negative T waves can also persist for a long period and sometimes remain a permanent sign of myocardial infarction. It should be noted that the absence of formation or “restoration” of pre-inverted T waves in the acute stage of myocardial infarction strongly suggests the development of post-infarction pericarditis [11].
Stages of development of a heart attack with ST segment elevation
The most acute stage of STEMI
First, a high coronary T appears on the cardiogram. The high coronary T before ST elevation is present for a very short time, so it is not always possible to register it. Then there is an increase in the ST segment, which merges with a high T.
Scheme 2. ECG fragments in the most acute stage of STEMI
Acute stage STEMI
Lasts up to 2-3 days (sometimes up to 2 weeks). The beginning of the acute phase is considered to be the appearance of the Q wave, which reflects the formation of a zone of myocardial necrosis. As the acute phase develops, the Q wave deepens, and the ST segment begins to decline towards the isoline. The T wave becomes negative.
Scheme 3. ECG fragment in the acute stage of STEMI
Subacute stage of STEMI.
Lasts for several weeks. The ECG records a decrease in the ST segment to the level of the isoline. At the same time, a deep negative T wave is formed.
Scheme 4. ECG fragment in the subacute stage
Scar stage STEMI
Dead myocardial cells are replaced by connective tissue, which leads to the formation of a scar. The areas of the myocardium surrounding the scar undergo compensatory hypertrophy. The number of leads on the ECG in which changes associated with a heart attack are recorded is reduced. The Q wave may become less deep, and the T wave returns to the baseline. The formed picture of post-infarction cardiosclerosis on the ECG persists throughout the patient’s life.
Sometimes the ST segment does not reach the isoline and remains elevated almost throughout life. As a rule, the QRS complex takes on the QS form, which may indicate the formation of a cardiac aneurysm.
Scheme 5. ECG fragments with post-infarction changes
Diagram 5 on the left shows a fragment of a cardiogram indicating a myocardial infarction. On the right is a fragment of a cardiogram in which the ST segment has not reached isolia and a QS complex has formed, turning into increased ST. This picture is called a “frozen ECG” and indicates a post-infarction cardiac aneurysm.
Reciprocal ST segment depression
ST segment depression in leads opposite the affected area, otherwise known as reciprocal depression, is a highly sensitive indicator of AMI. The pathogenesis of reciprocal changes remains unknown. Reciprocal changes have high sensitivity and a positive predictive value of up to 90% and are observed in approximately 70% of lower and up to 30% of infarcts involving the anterior wall of the LV, although, of course, their absence does not exclude the diagnosis of AMI [4, 5]. As a rule, ST segment depression is horizontal or oblique. The presence of reciprocal changes is especially important when there is doubt about the clinical significance of the recorded ST segment elevation. We especially note that reciprocal changes may be the only sign of AMI against the background of still unobvious ST segment elevation. Similar situations often occur in cases of myocardial infarction with damage to the lower wall. The presence of severe ST segment depression in the precordial leads against a background of normal heart rate or bradycardia in a patient with an ischemic painful attack strongly requires the exclusion of AMI.
Clinical case
A patient was admitted to the hospital with severe chest pain that lasted for three days. Taking analgesics and Nitroglycerin did not bring relief. Previously, a diagnosis of angina pectoris FC II was made. A week before the attack, I experienced severe stress, and my condition worsened. The cardiogram revealed a large-focal infarction localized in the anterior wall, acute stage. In the blood - increased myoglobin and troponin.
After a month of hospitalization, the patient was discharged for treatment on an outpatient basis. An ECG showed scarring in the affected area, and blood counts returned to normal.
Myocardial infarction of the anterior wall
Anteroseptal ST-segment elevation infarction in leads V1-V3 is a highly accurate indicator of left anterior descending coronary artery (LADCA) involvement. ST segment elevation in these three leads and in lead aVL, combined with ST segment depression of more than one mm in lead aVF, indicates occlusion of the proximal segment of the LCA. ST-segment elevation in leads V1, V2, and V3 without significant ST-segment depression in the inferior leads suggests occlusion of the LCA after origin of the first diagonal branch.
In some cases, the LPNCA wraps around the apex of the LV and supplies blood to the apical parts of the inferior wall in the distal part of the posterior interventricular groove. Rarely, the LCA extends along the entire length of the posterior sulcus, replacing the posterior descending artery. In the case of ST segment elevation in leads V1, V2 and V3 with ST elevation in the inferior leads, occlusion of the LCA of the distal origin of the first diagonal branch, in the area that irrigates the inferoapical parts of the LV, can be assumed [7].
Localization of infarction with ST elevation
Changes in cardiograms during a heart attack with ST segment elevation vary depending on which part of the heart the heart attack develops in. The location of the infarction can be determined by the ECG leads in which ST elevation is recorded and in which leads reciprocal ST depression appears. In this regard, remember which leads correspond to different parts of the myocardium. Look at diagram 6.
Scheme 6. Correspondence of cardiogram leads to different areas of the myocardium.
Schema source.
Diagram 7 below shows the location of large coronary arteries, the occlusion of which can lead to transmural infarction with appropriate localization.
Scheme 7. Large coronary arteries
| Localization of infarction | ST elevation leads | Leads with reciprocal ST depression |
| Interventricular septum | V1-V2 | |
| Front wall | V3-V4 | |
| Lateral wall of the left ventricle | I, aVL, V5-V6 | III, aVF |
| Bottom wall | II, III, aVF | I, aVL |
| Back wall | V7-V9 | V1-V3 (and high R in V1-V3) |
| Right ventricle | V1, III, II (STIII > STII), V3R - V5R | V2 |
The table above shows which leads show ST elevation or depression depending on the location of STEMI. In practice, ST elevation infarction usually affects more than one area. For example, an infarction of the interventricular septum is usually combined with an infarction of the anterior wall of the left ventricle. In this case, ST elevation will be not only in leads V1-V2, but also in V3-V4.
Let's consider STEMI options with different localizations.
Lower IM
AMI with isolated ST-segment elevation in leads II, III, and aVF is usually associated with damage to the right coronary artery (RCA) or the distal circumflex artery (CA). A rather unpleasant feature of AMI with damage to the inferior wall is that the ST segment elevation associated with the infarction can develop over a long period, up to two weeks, to become evident on the ECG [4]. The inferior wall can be supplied with blood from the right coronary artery (in 80% of cases) or from the OA, which is a branch of the left coronary artery.
ST segment elevation in lead III is greater than in lead II, and ST segment depression of more than one mm in leads I and aVL suggests damage to the RCA, which supplies the inferior wall. In the case of blood supply to the lower wall from the OA, the rise of the ST segment in lead III does not exceed the rise in lead II. In this case, either an elevation of the ST segment in aVL is observed, or it is located on the isoline [6, 7].
Left ventricular lateral wall infarction
Left ventricular lateral wall infarction with ST elevation, as discussed above, is usually associated with anterior wall infarction. In addition, it can be combined with infarction of the lower or posterior wall. It develops as a result of occlusion of the left anterior descending artery (LAD) and/or the circumflex coronary artery (LCX).
Isolated lateral wall infarction is less common and is associated with occlusion of the small branches of the LAD or the marginal branch of the LCX.
Scheme 10. Infarction of the lateral wall of the left ventricle
On the cardiogram with a lateral wall infarction, ST elevation is recorded in leads I, aVL, V5-V6. If ST elevation is only in leads I, aVL, but not in leads V5-V6, they speak of a high lateral infarction. A reciprocal decrease occurs in leads III, aVF.
Examples of lateral wall infarction combined with anterior wall infarction were shown above (see ECG 3-5).
ECG 6. High lateral left ventricular infarction
ECG source.
ECG 6 shows ST elevation in leads I and aVL, as well as reciprocal depression in leads III, aVF. There is no ST elevation in leads V5-V6. These are signs of high lateral left ventricular infarction.
Right ventricular myocardial infarction
Right ventricular MI is usually associated with occlusion at the level of the proximal RCA. The most sensitive ECG sign of right ventricular MI is ST segment elevation of more than one mm in lead V4R with a positive T wave in this lead [5]. This sign is rarely observed more than 12 hours after AMI, so right leads should be recorded as soon as possible in all patients with inferior wall infarction. On a standard 12-lead ECG, signs of AMI involving the right ventricle are ST segment elevation in lead V1 combined with ST segment elevation in leads II, III, and aVF (STIII greater than STII).
Right ventricular infarction is often missed because the standard 12-lead ECG does not have high sensitivity for right ventricular infarction. At the same time, the diagnosis of right ventricular infarction is important, as it may be associated with a state of hypotension caused by treatment with nitrates or diuretics. At the same time, in contrast to cardiogenic shock, which requires differential diagnosis, the patient responds well to fluid administration.
In approximately 40% of cases, inferior wall AMI is complicated by right ventricular infarction [2, 6]. Less commonly, right ventricular infarction is associated with occlusion of the circumflex artery and, if this branch is dominant, may be associated with inferolateral infarction. Right ventricular infarction can complicate anterior wall AMI and can rarely occur as an isolated phenomenon [15].
Expert advice
When the first signs of a heart attack appear, measures should be taken immediately.
I advise you to immediately call an ambulance, and while the doctor is on the way, provide the patient with complete rest, sit him down or put him in a position that will alleviate the condition as much as possible. Give Corvalol, Nitroglycerin, Aspirin, ventilate the room. The most dangerous period is the most acute period, which is usually manifested by very severe pain, shortness of breath, and rhythm disturbances. The patient’s life depends on the speed and correctness of the actions of the person nearby. When calling a doctor, it is best to describe the symptoms so that a specialized team can arrive to take an ECG, give oxygen, and administer medications to limit the area of necrosis.
Myocardial infarction of the posterior wall
The posterior descending coronary artery (PDCA), which supplies blood to the posterobasal sections, can be a branch of the RCA (in 85-90% of cases) or a branch of the OA (12), which determines the right or left type of coronary circulation. The diagnosis of AMI with posterior-basal lesions is often difficult when using a standard 12-lead ECG, while early detection of coronary thrombosis is very important from the point of view of prescribing thrombolytic therapy.
Changes in the ECG during AMI of the posterior basal sections are indirectly manifested in the anterior precordial leads. Leads V1-V3 record the potentials of not only the anterior, but also the opposite (posterior) wall, and changes in blood supply in this area are reflected in these leads. Typically, there is an increase in R waves that become wider and more dominant, as well as ST segment depression and high amplitude T waves pointing toward the posterior wall [3]. The use of leads V7-V9, recording posterobasal potentials, will show ST segment elevation in patients with AMI.
These additional leads provide valuable information and help in identifying patients who may benefit from urgent invasive therapy. In any case, registration of ST segment depression in leads V1-V2 should serve as a reason to exclude AMI of the posterobasal parts of the LV. In the cicatricial stage, a previous myocardial infarction in the posterior-basal sections will be indicated by the ratios R/S > 1 in lead V2 and RV2 > RV6, recorded against the background of the horizontal position of the electrical axis of the heart [2].
Lateral wall infarction.
Lesions in the proximal circumflex artery are often associated with lateral infarction and changes in leads I, aVL, V5-V6. Often, AMI can manifest itself as changes that occur isolated in lead aVL. In such cases, it is customary to diagnose AMI with damage to the high lateral parts of the LV [3].
Cost of consultation for myocardial infarction?
| Name of service | Price, rub.) |
| Initial appointment with a cardiologist | 2000 rub. |
| Repeated appointment with a cardiologist | 1500 rub. |
| Primary appointment with a general practitioner | 2000 rub. |
| Repeated appointment with a general practitioner | 1500 rub. |
| Prescription of treatment (drawing up an individual treatment regimen) | 1500 - 3000 rub. |
All our services and prices
ECG predictors of reperfusion
Pathogenetic therapy for AMI has the goal of restoring blood flow in the affected artery. Lack of restoration of blood flow (reperfusion) is the most powerful predictor of the development of LV systolic dysfunction and the risk of death after AMI. In the absence of reperfusion, 30-day mortality can reach 15% [14]. In turn, the resolution of ST segment elevation is an indicator of improved short-term (30-day) and long-term (one-year) prognosis [5]. Assessing ST segment resolution is also useful for deciding on further management of the patient.
Failure to resolve the ST segment within the first 90-120 minutes after thrombolytic administration should be a reason to consider angioplasty. A specific marker of reperfusion that has occurred is considered to be a reduction in ST segment elevation by more than 50-70% in the lead with maximum elevation, which is associated with the most favorable further prognosis. At the same time, a number of authors propose a criterion of 50% reduction in ST segment elevation after 60 minutes of reperfusion therapy as a predictor of a good prognosis in individuals with AMI [13]. Considering that the maximum effect from subsequent angioplasty after thrombolysis is achieved no later than 6-8 hours from the onset of AMI [14], reducing the time for assessing reperfusion has good reason.
Other ECG markers of reperfusion include T wave inversion within four hours of AMI onset. T wave inversion, which occurs within the first hours of reperfusion therapy, is a highly specific sign of restoration of blood flow. T wave inversion, which develops after more than four hours, is associated with natural ECG dynamics during AMI and does not indicate restoration of blood flow. Accelerated idioventricular rhythm 60-120 beats/min, late, paired, ventricular extrasystoles are also a highly specific marker of reperfusion. These rhythms are considered not dangerous and, as a rule, do not require antiarrhythmic therapy. Polymorphic ventricular tachycardia and ventricular fibrillation can also be associated with reperfusion, but are rare and more often a consequence of persistent coronary occlusion.
Myocardial infarction (heart attack) - symptoms and treatment
A patient with an acute heart attack must be promptly transported to the hospital to prevent complications and increase the chances of survival. The system of care for patients with myocardial infarction includes the following stages:
- Pre-hospital stage. Ambulance teams provide assistance and transport the patient to the hospital.
- Hospital stage. Help is provided in specialized vascular departments.
- Rehabilitation stage. Rehabilitation is carried out in special departments of hospitals or specialized cardiological sanatoriums.
- Dispensary observation and outpatient treatment. Clinical examination in the post-infarction period is carried out in regional or city cardiology centers or in cardiology offices of clinics [6].
At the prehospital stage, the following tasks are solved:
- an accurate diagnosis is established. If this fails, it is permissible to establish a tentative syndromic diagnosis as soon as possible;
- The patient is given a nitroglycerin tablet under the tongue (or use a nitro-containing spray) and 0.25-0.35 g of aspirin;
- pain is relieved by administering painkillers;
- acute circulatory failure and heart rhythm disturbances are eliminated;
- the patient is brought out of the state of cardiogenic shock;
- in case of clinical death, resuscitation measures are performed;
- transport the patient to the hospital as soon as possible.
Further therapy is determined by the stage (period) of myocardial infarction. In the acute and very acute period, the goal of treatment is to prevent an increase in the focus of myocardial necrosis, eliminate pain and other symptoms. It is important to restore blood flow through the heart arteries and relieve pain. The intensity of pain during this period is so great that the patient may die due to cardiac arrest. It is necessary to prevent severe complications. When the disease passes into the subacute stage and in the post-infarction period, the goal of therapy is to reduce the risk of attack recurrence and possible complications.
For the treatment of acute myocardial infarction, drugs from various pharmacological groups are used:
Painkillers. Analgesics from the group of narcotic painkillers (morphine, promedol, omnopon) in combination with analgin, antihistamines (diphenhydramine). Neuroleptanalgesia is most effective when a combination of the analgesic fentanyl with the strong antipsychotic droperidol is used. The effectiveness of these drugs is noticeable within a few minutes. Not only pain disappears, but also fear of death, unmotivated anxiety and psychomotor agitation. Tranquilizers (diazepam) can be used to relieve psychomotor agitation. To reduce hypoxia (decreased oxygen in tissues), oxygen inhalation is used using a nasal catheter.
Thrombolytic therapy. It is important to restore blood flow and dissolve blood clots so that the death of the heart muscle does not spread further. The smaller the area of necrosis, the higher the patient’s chances of successful rehabilitation and the lower the risk of life-threatening complications. Immediate use of drugs (preferably within the first hour after an attack) allows you to achieve maximum effectiveness of treatment. A time limit of three hours is allowed. To dissolve a blood clot, thrombolytic drugs are administered intravenously, for example, streptokinase, urokinase, alteplase. The dose depends on the patient's weight.
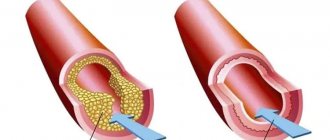
Restoration of coronary blood flow is also possible with the help of surgical treatment - stenting or coronary artery bypass grafting. A balloon catheter is inserted into a narrow section of the artery under fluoroscopic guidance. In this case, the atherosclerotic plaque is “crushed”, and the lumen of the heart artery increases. Then a stent (metal frame) can be installed into the lumen of the vessel.
Antiplatelet agents. Drugs from this group affect blood cells (platelets and red blood cells). The action of antiplatelet agents prevents platelet aggregation, improving blood flow. The main drug used is aspirin (acetylsalicylic acid). Contraindications to the use of aspirin: bleeding from the gastrointestinal tract, exacerbation of gastric or duodenal ulcers.
P2Y12 platelet receptor inhibitors are also used , which block platelet activation. The main blockers are ticagrelor, prasugrel and clopidogrel.
Intravenous/subcutaneous anticoagulants. , unfractionated heparin intravenously, is used to prevent deep vein thrombosis (DVT) and pulmonary embolism (PE) . Enoxaparin , which is also used to prevent venous thromboembolism, is administered subcutaneously.
To limit the area of myocardial ischemia and necrosis, it is necessary, in addition to restoring blood flow in the arteries of the heart, to reduce the hemodynamic load on the heart. Nitrates and beta blockers are used for this purpose.
Nitrates. They have an analgesic effect, reduce myocardial oxygen demand, increase coronary and collateral (bypass) blood flow, reduce the load on the heart muscle, and limit the size of the myocardial lesion. Their combination with beta blockers is especially effective, leading to rapid positive ECG dynamics and reducing the risk of sudden death [10].
Beta-blockers have an antiarrhythmic effect. The purpose of using beta-blockers (propranolol, metoprolol, atenolol) is to reduce the frequency and force of heart contractions, which will help reduce the load on the heart and the myocardial oxygen demand. Beta blockers continue to be used indefinitely in the absence of side effects and contraindications [1].