VERO-AMIODARONE
special instructions
Except in urgent cases, intravenous administration of amiodarone should be carried out only in the intensive care unit with constant monitoring of the ECG (due to the possibility of developing bradycardia and proarrhythmogenic effects) and lowering blood pressure.
The injectable form of amiodarone should be administered only as an infusion (except in cases of cardiac resuscitation due to cardiac arrest caused by ventricular fibrillation resistant to cardioversion (see "Dosage and Administration"), since even a very slow intravenous bolus may cause an excessive decrease in blood pressure, heart failure or severe respiratory failure.
In order to avoid reactions at the injection site (see “Side Effects”), the injectable form of amiodarone is recommended to be administered through a central venous catheter. Only in the case of cardiac resuscitation for cardiac arrest caused by ventricular fibrillation refractory to cardioversion, in the absence of central venous access (no central venous catheter in place), the injectable form of amiodarone can be administered into a large peripheral vein with maximum blood flow.
If treatment with amiodarone must be continued after cardiac resuscitation, the drug should be administered intravenously through a central venous catheter under constant monitoring of blood pressure and ECG.
Amiodarone should not be mixed in the same syringe or dropper with other medications.
Due to the possibility of the development of interstitial pneumonitis when severe shortness of breath or a dry cough appears after the administration of amiodarone, both accompanied and not accompanied by a deterioration in the general condition (increased fatigue, fever), it is necessary to perform a chest x-ray and, if necessary, discontinue the drug, since interstitial pneumonitis can lead to the development of pulmonary fibrosis. However, these phenomena are generally reversible with early discontinuation of amiodarone with or without the administration of glucocorticosteroids. Clinical manifestations usually disappear within 3-4 weeks. Recovery of the X-ray picture and lung function occurs more slowly (several months).
Following mechanical ventilation (eg, surgery) in patients receiving amiodarone, rare cases of acute respiratory distress syndrome, sometimes fatal, have been reported (possible interaction with high doses of oxygen). Therefore, it is recommended to strictly monitor the condition of such patients.
In patients receiving long-term treatment with amiodarone for cardiac arrhythmias, an increase in the incidence of ventricular fibrillation and/or an increase in the sensitivity threshold of the pacemaker or implanted artificial pacemaker has been reported, which may reduce their effectiveness. Therefore, before starting and during treatment with amiodarone, their correct functioning should be regularly monitored.
Due to the prolongation of the period of repolarization of the ventricles of the heart, the pharmacological effect of amiodarone causes certain changes in the ECG: prolongation of the QT interval, QTc (corrected), and the possible appearance of U waves. Allowable QT prolongation is no more than 450 ms or no more than 25% of the original value. These changes are not a manifestation of the toxic effect of the drug, but require monitoring to adjust the dose and assess the possible proarrhythmogenic effect. If II-III degree AV block, sinoatrial block or double-bundle intraventricular block develops, treatment with amodarone should be discontinued. If 1st degree AV block occurs, it is necessary to intensify monitoring of the patient.
If visual impairment occurs (blurred visual perception, decreased visual acuity), it is necessary to conduct a full ophthalmological examination, including fundus examination. If optic neuropathy or optic neuritis develops, treatment with amiodarone is discontinued due to the risk of blindness.
During the first 24 hours after starting use of the injectable form of amiodarone, severe acute liver damage may develop with the development of liver failure, sometimes with death. Regular monitoring of liver function is recommended before starting amiodarone use and regularly during amiodarone treatment. If the activity of “liver” transaminases increases, 3 times higher than the upper limit of normal, the dose of amiodarone should be reduced or discontinued.
General anesthesia. Before surgery, the anesthesiologist should be informed that the patient is receiving amiodarone. Treatment with amiodarone may increase the hemodynamic risk inherent in local or general anesthesia. This particularly applies to its bradycardic and hypotensive effects, decreased cardiac output and conduction disturbances.
Combinations with β-blockers other than sotalol (a contraindicated combination) and esmolol (a combination requiring special caution when used), verapamil and diltiazem can only be considered in the context of the prevention of life-threatening ventricular arrhythmias and in the case of restoration of cardiac activity in cardiac arrest caused by ventricular fibrillation resistant to cardioversion.
Electrolyte imbalances, especially hypokalemia: It is important to consider situations that may be accompanied by hypokalemia as predisposing to proarrhythmic effects. Hypokalemia should be corrected before starting amiodarone.
Side effects of the drug (see "Side Effects") are usually dose dependent; Therefore, care should be taken when determining the minimum effective maintenance dose to avoid or minimize the occurrence of adverse effects.
Amiodarone may cause thyroid dysfunction, especially in patients with a personal or family history of thyroid dysfunction. Therefore, in case of switching to oral amiodarone during treatment and several months after the end of treatment, careful clinical and laboratory monitoring should be carried out. If thyroid dysfunction is suspected, the concentrations of T3, T4 and TSH in the blood serum should be determined.
Clinical manifestations are usually mild, so symptoms such as weight loss, the occurrence of rhythm disturbances, angina attacks, and the development of CHF should alert the doctor. The diagnosis is confirmed by identifying a decrease in the concentration of thyroid-stimulating hormone (TSH) in the blood serum, determined using an ultrasensitive TSH test. In this case, amiodarone should be discontinued. Recovery usually occurs within a few months after treatment is stopped. First, clinical manifestations disappear, then normalization of thyroid function indicators occurs. Severe cases of thyrotoxicosis, which can sometimes be fatal (both due to the thyrotoxicosis itself and due to a dangerous imbalance between myocardial oxygen demand and oxygen supply), require emergency treatment. Treatment should be selected individually in each specific case: antithyroid drugs (which may not always be effective), glucocorticosteroids, beta-blockers.
Possible suppression of bone marrow function, manifested by the development of normocytic normochromic anemia, thrombocytopenia or neutropenia, possible formation of granulomas, in addition, in post-registration studies or observations, cases of the development of agranulocytosis, hemolytic anemia, pancytopenia were identified. Symptoms may regress after discontinuation of the drug and the prescription of glucocorticosteroids; if the drug is re-prescribed, they may recur.
While taking amiodarone, the development of undesirable mental phenomena is possible, including changes in consciousness, hallucinations and delirium. The developed condition may be resistant to the use of benzodiazepine drugs; discontinuation of amiodarone is necessary.
The use of amiodarone can cause the development of unpleasant skin phenomena, the most commonly reported development of increased photosensitivity and changes in skin tone (more often in patients under 60 years of age), less often - reversible alopecia.
Severe adverse events may develop, including toxic epidermal necrolysis, exfoliative dermatitis, bullous dermatosis, cutaneous vasculitis, linear IgA-dependent dermatosis, psoriasis, skin cancer, pruritus.
Patients should be instructed about the possibility of photosensitivity reactions, the need to avoid exposure to sunlight and use sunscreen if necessary. Increased sensitivity to sunlight may persist for several months after stopping amiodarone. In most cases, manifestations are limited to sensations of redness, burning or "twitching" of the skin exposed to intense sunlight, but severe phototoxic reactions can develop. Hypersensitivity reactions associated with the use of the drug include the cutaneous reactions listed above, as well as anaphylactic and anaphylactoid reactions, including shock, angioedema, lupus erythematosus, drug reaction with eosinophilia and systemic symptoms. It is possible to develop cross-allergic reactions to amiodarone in patients with hypersensitivity to iodine-containing contrast agents.
The safety and effectiveness of amiodarone have not been studied in children. Vero-amiodarone injection contains benzyl alcohol. Cases of severe choking with fatal outcome have been reported in newborns after intravenous administration of solutions containing benzyl alcohol.
Amiodarone amp 50mg/ml 3ml N10 (Borisov)
Medicines that can cause torsades de pointes are primarily class Ia and class III antiarrhythmic drugs and some antipsychotics. Hypokalemia is a predisposing factor, as well as bradycardia or congenital or acquired prolongation of the QT interval. Combinations with - Drugs that can cause torsade de pointes (TdP) are contraindicated. - Class Ia antiarrhythmic drugs (quinidine, hydroquinidine, isopyramide). - Class Ia antiarrhythmic drugs. III (dofetilide, ibutilide, sotalol). - Other drugs, such as bepridil, cisapride, difemanil, IV ritromycin, mizolastine, IV vincamine, moxifloxacin, IV spiramycin. - Sultopride. Increases the risk of ventricular rhythm disturbances (tachycardia type "pirouette"). These contraindications do not apply to the use of amiodarone for cardiopulmonary resuscitation in the event of cardiac arrest resistant to electrical defibrillation. Not recommended combinations with Cyclosporine Possible increase in the level of cyclosporine in plasma associated with a decrease in the metabolism of the drug in the liver, with possible nephrotoxic manifestations .Determining the level of cyclosporine in the blood, checking renal function and reviewing the dosage during treatment with amiodarone and after discontinuation of the drug. Diltiazem for injection Risk of bradycardia and atrioventricular block. If the combination is unavoidable, strict clinical and continuous ECG monitoring must be established. Verapamil for injection Risk of bradycardia and atrioventricular block. If a combination is unavoidable, it is necessary to establish strict clinical and constant ECG monitoring. Antiparasitic drugs that can cause torsades de pointes (halofantrine, pentamidine, lumefantrine) If the combination is unavoidable, preliminary control of the QT interval and ECG monitoring is necessary. Neuroleptics that can cause ventricular tachycardia of the “pirouette” type: Some phenothiazine neuroleptics (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine), benzamides (amisulpride, sulpiride, tiapride, veralipride), butyrophenones (droperidol, haloperidol), other neuroleptics (pimozide). The risk of ventricular rhythm disturbances increases. (tachycardia of the “pirouette” type).MethadoneThe risk of ventricular rhythm disturbances (tachycardia of the “pirouette” type increases). Recommended: ECG and clinical observation. Combinations requiring precautions when using Amiodarone with: Oral anticoagulants: Increased anticoagulant effect and risk of bleeding, due to increased plasma concentrations of anticoagulants. The need for more frequent monitoring of the level of prothrombin in the blood and MHO (INR), as well as adaptation of doses of anticoagulants during treatment with amiodarone and after discontinuation of the drug. Beta blockers, with the exception of sotalol (a contraindicated combination) and esmolol (a combination that requires caution in use) Violations contractility, automaticity and conductivity (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring. Beta blockers prescribed for heart failure (bisoprolol, carvedilol, metoprolol) Contractility and conduction disorders (synergistic effect) with the risk of developing severe bradycardia. Increased risk of ventricular arrhythmias, especially tachycardia of the “pirouette” type. Regular clinical and electrocardiographic monitoring is required. Cardiac glycosides Impairments of automaticity (excessive bradycardia) and atrioventricular conduction (synergism of action). When using digoxin, an increase in its concentration in plasma (due to decreased clearance of the alkaloid). It is necessary to carry out clinical and ECG monitoring, as well as determine the level of digoxin in plasma); It may be necessary to change the dose of digoxin. Oral diltiazem Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG monitoring. Oral verapamil Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG monitoring. Esmolol Disorders of contractility, automaticity and conduction (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring. Hypokalemic drugs: potassium-sparing diuretics (in monotherapy or combination), stimulant laxatives, amphotericin B (iv), glucocorticoids (systemic), tetracosactide. Increases the risk of ventricular rhythm disturbances, especially tachycardia of the “pirouette” type "(hypokalemia is a predisposing factor). Clinical and ECG monitoring, laboratory tests. Lidocaine Risk of increased plasma concentrations of lidocaine, with the possibility of neurological and cardiac side effects, due to amiodarone's reduction in the metabolism of lidocaine in the liver. Clinical and ECG monitoring, if necessary, dose adjustment of lidocaine during treatment with amiodarone and after its discontinuation. Orlistat Risk of decreased plasma concentrations of amiodarone and its active metabolite. Clinical and, if necessary, ECG monitoring, Phenytoin (and, by extrapolation, fosphenytoin) Increased plasma levels of phenytoin with symptoms of overdose, especially of a neurological nature (decreased metabolism of phenytoin in the liver). Clinical monitoring and determination of plasma phenytoin levels; if possible, reduce the dose of phenytoin. Simvastatin Increased risk of side effects (depending on dose) such as rhabdomyolysis (decreased metabolism of simvastatin in the liver). The dose of simvastatin should not exceed 20 mg per day. If a therapeutic effect cannot be achieved at this dose, you should switch to another statin that does not interact with this type of interaction. Tacrolimus An increase in the level of tacrolimus in the blood due to inhibition of its metabolism by amiodarone. Blood levels of tacrolimus should be measured, renal function monitored, and tacrolimus levels leveled off. Drugs that cause bradycardia: Many drugs can cause bradycardia. This is especially true for class Ia antiarrhythmic drugs, beta blockers, some class III antiarrhythmic drugs, some calcium channel blockers, digitalis, pilocarpine and anticholinesterase agents. Risk of excessive bradycardia (cumulative effect). Combinations to consider Drugs that cause bradycardia: calcium channel blockers with bradycardic effect (verapamil), beta blockers (except sotalol), clonidine, guanfacine, digitalis alkaloids, mefloquine, cholinesterase inhibitors (donezepil, galantamine, rivastigmine, tacrine, ambemonium, pyridostigmine, neostigmine), pilocarpine. Risk of excessive bradycardia (cumulative effects). Incompatibilities When using PVC material or medical equipment plasticized with 2-diethylhexyl phthalate (DEHP) in the presence of amiodarone injection solution, DEHP may be released. To minimize exposure to DEHP, it is recommended that the solution be final diluted before infusion in DEHP-free equipment.
Amiodarone (Cordarone, Sanofi-Aventis), introduced into medical practice in 1962 as a treatment for coronary heart disease (CHD), has now acquired the status of the most widely used antiarrhythmic drug in the world. Interest in amiodarone especially increased in the 1990s, when it was demonstrated to have a beneficial effect on the survival of patients who had suffered myocardial infarction (MI), and, on the contrary, a negative effect on the life prognosis of class I antiarrhythmic drugs (AAP). In recent decades, amiodarone has been included in European and North American guidelines for the treatment of various cardiac pathologies, which has led to a further increase in its use. In 1998, the share of amiodarone in the structure of prescribed AAPs was 34.5% in Europe, 32.8% in North America, and 73.8% in Latin America [1].
Pharmacodynamics of amiodarone
In the most widely used classification, Vaughan Williams, amiodarone is classified as a class III AAP, which slows repolarization and increases the duration of the action potential and myocardial refractoriness. However, the classification of amiodarone into class III AAP is relatively arbitrary, since the mechanism of action of the drug is much broader. In fact, it is determined by all four main mechanisms of action of AAP:
- amiodarone blocks potassium and, to a lesser extent, sodium and calcium channels;
- has antiadrenergic properties (see figure).
The antiadrenergic mechanism of action of amiodarone differs from that of beta-blockers: it inhibits the formation of adenylate cyclase and helps reduce the amount
beta-adrenergic receptors [2]. In this regard, the drug does not enter into a competitive relationship with beta-blockers and, when administered together, enhances the effect of the latter. Apparently, an important role in the antiarrhythmic effect of amiodarone is played by its ability to inhibit the synthesis of thyroxine in the thyroid gland, as well as the conversion of thyroxine (T4) to triiodothyronine [3]. The latter is due to the structural similarity of amiodarone to T4 and the significant iodine content in the drug molecule (75 mg iodine/200 mg amiodarone - 37.5%). It is believed that the antiarrhythmic effect of amiodarone is the result of hypothyroidism at the tissue level [4].
Amiodarone inhibits the automatism of the sinus node and causes a decrease in heart rate (HR). In addition, it increases the refractoriness of the atrioventricular (AV) node, atria and ventricles, and slows down the conduction of impulses in all parts of the conduction system of the heart, including additional conduction pathways. The maximum effect of oral amiodarone on the sinus and AV nodes is observed after approximately 2 weeks, refractoriness in the ventricles develops more slowly, reaching a maximum by the 10th week of therapy [5].
Unlike other AAPs, amiodarone does not have a pronounced negative inotropic effect. In addition, the decrease in the force of contraction of the left ventricle (LV) is also counteracted by a moderate decrease in systemic vascular resistance caused by the drug [6]. This allows the use of amiodarone in patients with heart failure (HF), including those with severe LV dysfunction. Another important advantage of amiodarone over other classes of AAP is its low arrhythmogenic potential.
Along with the antiarrhythmic effect, amiodarone also has a pronounced antianginal effect, due to both the expansion of the coronary arteries and a decrease in the myocardial oxygen demand. Moreover, it slightly reduces peripheral vascular resistance, having little effect on blood pressure [4].
Pharmacokinetics of amiodarone
Amiodarone is slowly absorbed from the gastrointestinal tract. Its bioavailability when taken orally is 35–65%. A significant part of the drug binds to proteins and lipids [8]. This determines the large volume of distribution of amiodarone (50 l) and its accumulation at the beginning of treatment in almost all tissues, especially in fatty inclusions. To saturate all binding sites in the body, about 15 g of the drug is required, so its therapeutic effect develops slowly: the onset of the effect is after 2-3 days, maximum after 8-12 weeks. Stable concentrations of amiodarone in the blood, depending on the individual characteristics of the patient, are created after one or several months. Even with intravenous administration, the antiarrhythmic effect of amiodarone reaches its maximum only after several hours.
Deiodination plays a certain role in the clearance of amiodarone, but the drug is predominantly metabolized in the liver to form an active metabolite, desethylamiodarone, which is not inferior in antiarrhythmic activity to amiodarone. Removal of amiodarone from the body begins a few days after the start of therapy. The drug is excreted mainly in bile and feces. The half-life is subject to significant interindividual fluctuations (from 6 to 180 days), averaging 52 days [8]. After stopping amiodarone, its removal from the body continues for several months, and its pharmacological effect lasts for several weeks.
The level of drug concentrations in the blood varies from patient to patient, so dose selection should be individualized. For long-term treatment of supraventricular and ventricular arrhythmias, amiodarone is usually used in doses of 200 to 400 mg/day, but in some patients it is effective at a daily dose of 100 mg [9]. Taking into account the pharmacokinetics of amiodarone, in the first weeks of treatment it is prescribed in higher doses for the purpose of saturation (“amiodaroneization”). For supraventricular arrhythmias, the saturating dose is usually 600–800 mg/day (if rapid saturation is necessary, it can be increased to 1000–1200 mg/day). When an antiarrhythmic effect is achieved, the dose is gradually reduced to a maintenance dose (first by 200 mg, then 100 mg every 2 weeks) [4]. For the treatment of ventricular tachyarrhythmias, foreign authors recommend a saturating dose of 1200–1800 mg/day for 1–2 weeks, then 800 mg/day for 2–4 weeks, 600 mg/day for a month and then 200–400 mg [ 10]. However, when using such treatment regimens, it should be remembered that amiodarone plasma concentrations >2.5 mg/l are associated with an increased risk of toxicity [11]. The drug is administered intravenously at an initial dose of 5 mg/kg as a rapid infusion over 15–30 minutes, then 10–20 mg/kg/day (on average from 600–800 mg/day to 1200 mg/day) in 250 ml glucose solution for several days.
The effectiveness of amiodarone and indications for its use
The variety of mechanisms of action of amiodarone determines its high effectiveness in a variety of heart rhythm disorders: extrasystoles of any origin, parasystoles, all types of supraventricular tachycardias, paroxysmal atrial fibrillation and flutter, paroxysmal tachycardias in patients with ventricular pre-excitation syndromes (Wolf-Parkinson-White syndrome, Clerk syndrome). Levi-Cristesco, etc.), coronarogenic and most non-coronarogenic ventricular tachycardias [4].
Deciding on the prescription of amiodarone requires being guided by the general principles of the use of AAP. In particular, it is necessary to evaluate the type of arrhythmia and its impact on life prognosis. For example, in asymptomatic supraventricular extrasystoles and mild ventricular arrhythmias, the potential risk of using AAPs outweighs the benefits, and therefore their use in these patients is usually not recommended.
In atrial fibrillation (AF), due to the risk of thromboembolism, attempts to restore sinus rhythm are made within the first 2 days or after 3 weeks of anticoagulant therapy. In the paroxysmal form of MA, amiodarone is used both for the relief and prevention of attacks. The effectiveness and reasonable safety of amiodarone as a means of restoring sinus rhythm in a wide range of patients with AF were demonstrated in two meta-analyses [12, 13]. When administered orally to restore and maintain sinus rhythm in patients with atrial fibrillation and flutter, its effectiveness in clinical studies ranged from 53 to 87% [14]. A regimen using a saturating intravenous dose followed by switching to oral administration of the drug allowed restoration of sinus rhythm in 47–93% of patients [15]. According to generalized data from seven randomized studies, when administered intravenously, amiodarone can stop on average 66.5% of paroxysms of atrial fibrillation and flutter, not inferior in this indicator to propafenone, procainamide, disopyramide and other AAPs [16].
When stopping attacks of MA, amiodarone has similar effectiveness to flecainide, but has an important advantage over the latter: it leads to a slowdown in heart rate even when it is not possible to restore sinus rhythm [17]. On the contrary, flecainide accelerates ventricular contractions. A meta-analysis of clinical trials showed that, although the effect of amiodarone develops more slowly than class IC AAPs, their effectiveness 24 hours after the start of therapy in patients with new-onset AF does not differ [13].
Amiodarone is superior to propafenone and sotalol in preventing MA relapses. The advantages of amiodarone over sotalol and propafenone, which is structurally similar to flecainide, in the chronic treatment of paroxysmal or persistent atrial fibrillation have been proven in three large randomized trials [18–20]. Their results suggest that amiodarone is approximately 2-fold superior to comparator drugs in maintaining sinus rhythm one year after initiation of therapy. The CTAF (Canadian Trial of Atrial Fibrillation) study demonstrated not only the higher effectiveness of amiodarone compared to propafenone and sotalol in maintaining sinus rhythm, but also a reduction in the cost of treating AF when used [21]. According to the results of the HOT CAFE Polish Study, amiodarone is the most effective drug for restoring and maintaining sinus rhythm in patients with persistent AF resistant to electrical cardioversion and standard pharmacological prophylaxis [22]. It is the drug of choice for maintaining sinus rhythm during paroxysmal AF and after cardioversion in patients with HF [23].
Amiodarone is included in the European Society of Cardiology guidelines for the treatment of atrial fibrillation [24].
Amiodarone is also widely used as a first-line drug for the treatment of ventricular tachyarrhythmias. In clinical studies, the effectiveness of intravenous administration of the drug for ventricular tachycardia and ventricular fibrillation ranged from 51 to 100% [14]. In a comparative study with bretylium in patients with severe unstable ventricular tachyarrhythmias, intravenous amiodarone was noninferior to comparator drug and was associated with lower rates of hypotension and study dropout (20% of patients receiving amiodarone 1000 mg/day vs. 32% of patients receiving bretylium at a dose of 2500 mg/day) [25].
The effectiveness of amiodarone in cardiac arrest survivors was demonstrated in studies conducted during a period when implantable cardioverter defibrillators (ICDs) were not available. These studies demonstrated the survival benefits of amiodarone over traditional drugs such as quinidine and procainamide (procainamide).
From 1985 to 1995, a large number of studies of amiodarone were conducted in patients without a history of persistent ventricular arrhythmias but at high risk of sudden death. A meta-analysis of eight randomized controlled trials, including a total of 5101 patients with recent MI, and five randomized controlled trials, including 1452 patients with chronic HF, showed that prophylactic amiodarone in high-risk patients reduced the likelihood of death from arrhythmias/sudden heart failure. death by an average of 29%, and overall mortality by 13% [26]. According to the meta-analysis, the effect of amiodarone on overall and sudden mortality did not depend on the age and gender of patients, the functional class of HF, the value of LV ejection fraction (EF), the frequency of ventricular extrasystole and the presence of non-sustained ventricular tachycardia according to 24-hour ECG monitoring.
In the CASCADE (Cardiac Arrest Study in Seattle: Conventional Versus Amiodarone Drug Evaluation) trial, amiodarone was superior to “standard” therapy (mainly Class I antiarrhythmic drugs) in preventing arrhythmia recurrence in high-risk patients with ventricular fibrillation [27].
The benefits of amiodarone over class I AAP in preventing sudden death in high-risk patients were demonstrated in a large meta-analysis, including 61 studies (23,486 patients) of class I AAP, 56 studies (53,521 patients) of class II AAP, 14 studies (5713 patients) class III AAP and 26 studies (21,644 patients) class IV AAP [28]. A decrease in the risk of death under the influence of amiodarone and beta-blockers and, on the contrary, an increase in the risk of death with the use of class I AAP have been shown.
The advantage of amiodarone over beta-blockers is the possibility of its use in patients with organic cardiac pathology and severe heart failure, for whom beta-blockers cannot be prescribed in more than 20% of cases due to the initial negative inotropic effect [29]. In addition, two large studies, EMIAT (European Myocardial Infarction Amiodarone Trial) and CAMIAT (Canadian Amiodarone Myocardial Infarction Arrhythmia Trial), showed that amiodarone combines well with beta-blockers and increases their effectiveness in patients after MI [30].
In a number of studies, oral amiodarone improved survival in the long-term post-infarction period [31, 32]. Intravenous administration of amiodarone during the acute period of MI can alleviate ischemia and thus control arrhythmia [14]. The cost-effectiveness of the use of amiodarone in post-infarction patients with suppression of heart rate variability has been shown [33].
A review of 15 targeted randomized controlled trials of amiodarone (total of 5864 participants, 2936 receiving amiodarone) suggests that in patients at risk of sudden death, the drug leads to a 10–19% reduction in all-cause mortality [34]. The risk reduction under the influence of amiodarone was equally pronounced in patients with a history of myocardial infarction, patients with heart failure and symptomatic arrhythmia.
In recent years, a number of comparative studies in patients with malignant ventricular arrhythmias and a meta-analysis of three large studies have demonstrated the survival benefits of ICDs over amiodarone. However, when meta-analyses subdivided patients into groups depending on LVEF, it became apparent that the benefits of ICDs were mainly seen in patients with an EF < 35%, while patients with a history of symptomatic ventricular arrhythmia and normal LV function had poor treatment outcomes. when using amiodarone and ICD were the same [35]. In patients at moderate risk of arrhythmic death, amiodarone reduces the risk of cardiac arrest or sudden death by 20–30% [17].
Since in many countries, including Russia, the widespread use of ICDs is limited by their high cost, amiodarone continues to retain important clinical significance as a means of primary and secondary prevention of sudden death. In addition, amiodarone has been successfully used in patients refractory to electrical cardioversion, as well as in patients with ICDs in whom frequent discharges of the latter lead to a significant deterioration in quality of life (amiodarone reduces the frequency of discharges without affecting their threshold). In addition, patients with ICDs often require AADs to treat atrial tachyarrhythmias. In general, up to 70% of such patients require AAP [36]. An analysis of data from 429 patients with ICD suggests that concomitant use of amiodarone significantly improves treatment outcomes [37]. Amiodarone is also used to prepare for electropulse therapy.
A number of studies have demonstrated a higher effectiveness of amiodarone in patients with non-ischemic heart failure compared to patients with coronary artery disease. For example, in the GESICA study, which predominantly included patients with congestive non-ischemic HF with an EF less than 35%, long-term (2 years) therapy with amiodarone at a dose of 300 mg/day led to a decrease in total and sudden mortality [38]. The beneficial effect of amiodarone on long-term prognosis was especially pronounced in patients with dilated cardiomyopathy.
Moreover, the results of the AMIOVIRT trial (Amiodarone versus implantable cardioverter–defibrillator: randomized trial in patients with nonischemic dilated cardiomyopathy and asymptomatic nonsustained ventricular tachycardia) suggest that amiodarone is superior to ICD in patients with nonischemic dilated cardiomyopathy, an important substrate of sudden death [39]. ]. In this study, at 1 and 3 years of follow-up, patient survival was similar in the amiodarone and ICD groups, but there was a trend towards increased arrhythmia-free survival in the amiodarone group. The quality of life of patients after a year of treatment did not differ in both groups. At the same time, the cost of treatment in the amiodarone group was $8,879 versus $22,039 in the ICD group.
The results of a recent prospective study of 37 patients with decompensated HF despite optimal therapy suggest that amiodarone may be useful in patients with idiopathic dilated cardiomyopathy, even in the terminal stage, which is considered a contraindication to its use [40]. In this study, the probability of survival at 2 years in patients with cardiomyopathy receiving oral amiodarone 400 mg/day in combination with weekly dobutamine infusions (10 mcg/kg/min) was 44%. The same figure in patients with coronary artery disease who received the same therapy was 5%.
According to experimental data, long-term use of amiodarone in dilated cardiomyopathy prevents LV remodeling, restores the tone of cardiac sympathetic innervation and improves heart function [41].
Thus, the available evidence-based medicine indicates the effectiveness of amiodarone for ventricular arrhythmias and as a means of preventing sudden death. These data provided the basis for the inclusion of amiodarone in the European ICD Society guidelines for the treatment of HF [42] and the prevention of sudden death [43].
Amiodarone is a valuable prophylactic agent during cardiac surgery. According to the results of a recent meta-analysis, prophylactic use of amiodarone in these patients leads to a reduction in the incidence of AF, ventricular tachyarrhythmias and stroke, as well as a reduction in postoperative hospitalization [44].
Another meta-analysis showed that prophylactic use of amiodarone during cardiothoracic surgery is associated not only with favorable clinical outcomes, but also with a reduction in the overall cost of treatment [45]. The cost-effectiveness of amiodarone for the prevention of AF after open-heart surgery was also demonstrated in a targeted pharmacoeconomic study [46].
The American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation in patients undergoing cardiac surgery recommend amiodarone as the drug of choice for pharmacological cardioversion of postoperative atrial fibrillation and flutter in patients with LV dysfunction who do not require emergency cardiac cardioversion [47]. .
Safety and tolerability of amiodarone
The frequency and severity of side effects of amiodarone depend on the dose, duration of use and consideration of contraindications when prescribing it. Extracardiac contraindications to amiodarone include:
- thyrotoxicosis (the drug can be prescribed during preoperative preparation of patients with goiter);
- active autoimmune thyroiditis;
- fibrosing alveolitis, other severe interstitial lung diseases with immune pathogenesis;
- severe damage to the liver, cornea;
- hypersensitivity to iodine preparations (skin allergy to iodine does not exclude the use of amiodarone, since iodine is absorbed through the skin in significantly larger quantities) and to the drug itself.
Caution should be exercised when prescribing amiodarone to patients with any severe immune diseases [4]. It is contraindicated for use during lactation. During pregnancy, amiodarone is prescribed only for health reasons, since it can have an undesirable effect on the fetal thyroid gland.
Cardiac contraindications to the use of amiodarone are:
- bradycardia (heart rate < 55–50 per minute), other serious manifestations of sick sinus syndrome (repeated pauses > 2–3 s);
- pronounced prolongation of the PQ interval (> 0.22–0.24 s);
- prolongation of the QTc interval to 460–500 ms or AV block of II (especially 2:1) and III degrees;
- two- and three-bundle blockade [4].
Quite common side effects of amiodarone are nausea and vomiting. They usually occur in the early stages of treatment, more often when using saturating doses [17]. Other side effects of the drug, on the contrary, are more often observed with long-term treatment. The most common among them are constipation, anorexia, taste disturbance, benign microdeposits in the cornea and blue-gray pigmentation of the skin, which develops slowly, but in most cases is irreversible. Pigment deposits in the corneal epithelium can in rare cases lead to minor visual impairment.
Many patients have increased sensitivity to sunlight, predominantly not to ultraviolet, but to the visible spectrum, so the prophylactic use of lotions against ultraviolet rays may be ineffective [17]. With active questioning, 10–20% of patients are diagnosed with sleep disturbances accompanied by vivid dreams. In most cases, sleep returns to normal over time or when the dose of the drug is reduced.
With long-term use of amiodarone in relatively high doses, neurological disorders may occur, the most common of which are peripheral sensory and/or motor neuropathies. Physicians should be vigilant for early signs of neuropathies, as they may be irreversible [17].
Side effects of particular concern include chronic hepatitis, thyroid dysfunction, and pulmonary toxicity. The latter can occur in an acute form that responds to treatment with steroids, but more often manifests itself as chronic fibrosis. To date, there is no evidence that pulmonary complications develop more often in people with chronic lung diseases, so the presence of the latter is not an absolute contraindication to the use of amiodarone [17]. If hepatitis or toxic lung damage is suspected, the drug should be discontinued.
Hyperthyroidism is more likely to develop in areas with iodine deficiency in the diet, while hypothyroidism is more likely to develop in areas with sufficient iodine. When using amiodarone at a dose of 300 mg/day for 6 weeks, urinary iodine excretion increases 40 times. This dose, as a rule, does not suppress the function of the thyroid gland, since it stimulates a compensatory increase in the synthesis of hormones (the Wolff-Chaikoff phenomenon) and iron, promoting the body’s adaptation to excess iodine [48].
Amiodarone-induced thyrotoxicosis (AIT) can develop both against the background of an existing pathology of the thyroid gland (AIT type I) and in patients with an intact thyroid gland (AIT type II). In type II AIT, which is based on destructive thyroiditis, glucocorticoids are often effective [49].
If signs of thyrotoxicity appear, amiodarone is recommended to be discontinued, but in some cases it is permissible to continue treatment with simultaneous therapy aimed at normalizing thyroid function [17].
Cardiac side effects of amiodarone include severe sinus bradycardia, sinoatrial or AV block. According to a meta-analysis of double-blind placebo-controlled studies, the risk of developing bradycardia requiring drug discontinuation or a break in treatment is 2.4% over the course of a year compared to 0.8 in the placebo group [26]. If AV block develops, amiodarone should be discontinued. If there is an urgent need to continue treatment with amiodarone, a permanent pacemaker should be provided [17].
The presence of a blockade of one of the bundle branches is not a contraindication to the use of amiodarone. However, in such patients it is necessary to control the width of the QRS complex - it should not increase by more than 25% [4].
When amiodarone is prescribed for the prevention of postoperative AF, bradycardia and hypotension may develop. According to the results of a meta-analysis, the risk of these complications increases with intravenous administration of the drug, initiation of prophylaxis in the postoperative period, and use of doses above 1 g/day [50].
As already noted, amiodarone has the least arrhythmogenic effect among all AAPs. In seven placebo-controlled studies of the drug, no proarrhythmic events were recorded [51]. In uncontrolled studies with a total of 2878 participants, proarrhythmic events developed in 2% of patients, including 0.7% torsade de pointes [50].
Prolongation of the QT interval on the ECG is a sign of the therapeutic effect of amiodarone, since its main electrophysiological mechanism is prolongation of repolarization of the cardiac action potential. For unknown reasons, torsade de pointes arrhythmia occurs much less frequently with amiodarone than with other drugs that prolong the QT interval. In most cases, it develops against the background of a significant initial prolongation of QT, and often resolves spontaneously with drug withdrawal and/or acceleration of the heart rate [52, 53]. In general, the incidence of torsades de pointes does not exceed 0.5% [1, 26]. In a number of long-term studies of amiodarone, including two large ones (462 and 589 patients, respectively), not a single case of this arrhythmia was reported [54, 55]. This may be due to the effect of amiodarone on calcium channels. Experiments on animals have shown that all substances that reduce intracellular calcium concentration help reduce the frequency of torsades de pointes [17]. However, in patients in whom this type of arrhythmia has been observed while using other drugs that prolong the QT, amiodarone should be prescribed only if there are no alternatives [17].
In general, the frequency of arrhythmogenic effects when using low doses of amiodarone ranges, according to different authors, from less than 1 to 5%.
Only isolated cases of worsening arrhythmia during treatment with amiodarone have been described [10]. As a rule, this was observed in patients with hypokalemia or concomitantly taking AAP of other groups, most often class I A. No study in patients with arrhythmia showed an increase in mortality under the influence of amiodarone.
Amiodarone is well tolerated in patients with heart failure. In a study of 516 patients with HF, amiodarone resulted in a reduction in hospitalization for congestive HF and an improvement in HF functional class [39]. In the placebo-controlled CHF-STAT study (674 patients with HF), treatment with amiodarone was associated with a significant increase in LVEF [56]. Suppression of myocardial contractility in patients with LV dysfunction was reported in only one study using intravenous amiodarone [57].
According to a meta-analysis, the risk of quite severe side effects that can cause amiodarone withdrawal is within a year: from the lungs 1%, liver - 0.6, thyroid - 6.9 (hypothyroidism - 6, hyperthyroidism - 0 .9%; ) [26].
Peripheral neuropathies develop within a year in 0.3% of patients. It should be noted that hypothyroidism in many cases is well corrected by replacement therapy with thyroid hormones, including during ongoing treatment with amiodarone. As noted above, continued use of the drug is currently allowed with appropriate correction in some patients with hyperthyroidism. In clinical trials, the discontinuation rate of low-dose amiodarone was approximately 1.5 times higher than placebo [58].
It should be noted that the incidence of side effects of amiodarone varies depending on the source of information [59]. Thus, in the WHO database of spontaneous reports, the most common side effect was thyroid dysfunction; among spontaneous reports published in medical journals, pulmonary disorders predominated, and in a meta-analysis of clinical trials, cardiac conduction disorders predominated.
Preventing side effects of amiodarone
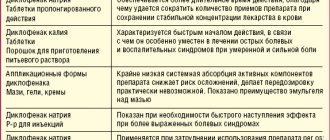
Side effects of amiodarone are largely dose-dependent and can be corrected if detected early. The benefit/risk ratio of amiodarone can be significantly improved with proper examination of patients, individual selection of doses and monitoring of treatment. Before prescribing the drug, it is necessary to determine the levels of T4, thyroid-stimulating hormone (TSH) and liver enzymes, perform an ultrasound of the thyroid gland and chest x-ray, evaluate the ECG to exclude prolongation of the QT interval, bradycardia and signs of hypokalemia, and determine the level of potassium in the blood serum. These indicators require monitoring during treatment (). Methods for diagnosing and treating side effects of amiodarone are presented in.
As mentioned above, the risk of developing undesirable effects is significantly reduced when the dose of the drug is reduced. Selection of the minimum effective dose is one of the most important elements of the correct use of amiodarone. Its use in a maintenance dose of up to 200 mg/day intermittently avoids serious side effects in most patients. A low dose of amiodarone (200 mg/day) is well tolerated, and the most common side effect, thyroid dysfunction, is reversible [62].
Other key principles for improving the safety of amiodarone treatment include prompt recognition and management of side effects and vigilance for drug interactions (). It should be remembered that with the simultaneous use of amiodarone with class I AAP, sotalol and antidepressants (mainly tricyclics), the risk of developing torsades de pointes arrhythmia increases; with verapamil, diltiazem and beta-blockers - AV blockade; with laxatives – hypokalemia and ventricular tachycardia. In addition, it should be remembered that amiodarone enhances the effect of cardiac glycosides, nitrates and anticoagulants, so the daily dose of these drugs must be reduced by 1/3 or ½ [7].
Generic amiodarone
AAPs are a pharmacological group with a narrow therapeutic index, therefore even minor changes in their pharmacokinetics, leading to changes in the concentration of the active substance in the blood, can lead to both a decrease in effectiveness and an increase in toxicity. This places special demands on the quality of drugs in this group. Even when compiling various lists (essential drugs, formulary, etc.) for AAP, as well as for some other pharmacological groups with a narrow therapeutic index (cardiac glycosides, antiepileptic drugs, anticoagulants), an exception is allowed - along with generic names, you can indicate and trade names.
In this regard, it should be emphasized that all large clinical studies were conducted using the original drug amiodarone - Cordarone. The data obtained from the study of Cordarone cannot be automatically transferred to its generics. A fairly large number of cases have been published in the literature where the transfer of a patient from Cordarone to a generic was accompanied by relapses of arrhythmia. For example, Reiffel JF and Kowey PR described 44 cases of arrhythmia recurrence, seven proarrhythmic events and three deaths when replacing Cordarone with generic amiodarone [63]. Pollak P. provides data on increased toxicity of generic amiodarone due to changes in the ratio of concentrations of the drug and its active metabolite [64]. An analysis of 284 medical histories of patients admitted to the hospital for recurrent supraventricular and ventricular tachyarrhythmias, carried out by domestic authors, also showed that in some cases the transition from treatment with Cordarone to the use of its generic analogues leads to an increase in relapses of atrial fibrillation and the development of serious, sometimes life-threatening complications [65].
Conclusion
The therapeutic value of any drug is determined by its benefit/risk ratio. The latter depends not only on the properties of a particular drug, but also on other factors:
- the severity of the disease for which it is used;
- outcome of the disease in the absence of treatment;
- availability of therapeutic alternatives, their effectiveness and safety.
The unique pharmacological properties of amiodarone ensure its high effectiveness against supraventricular and ventricular arrhythmias, a preventive effect against sudden death, low arrhythmogenic potential, and the possibility of use in patients with LV dysfunction. Despite the large number of potential side effects, including serious ones, proper use of amiodarone allows it to be used quite safely in most patients. This determines the favorable benefit/risk ratio of amiodarone as a therapeutic and prophylactic agent for a wide range of supraventricular and ventricular arrhythmias. Amiodarone is one of the most effective drugs for the treatment of almost all arrhythmias, with the exception of ventricular tachycardia such as torsades de pointes and severe arrhythmias caused by intoxication with cardiac glycosides. According to cardiologists, amiodarone (Cordarone) remains the number one drug in arrhythmology practice [4].
The role of amiodarone in the treatment of arrhythmias
Amiodarone is undoubtedly the most effective antiarrhythmic drug (AAD) available. It is even called an “arrhythmolytic drug.” Although amiodarone was synthesized in 1960, and reports of its antiarrhythmic activity first appeared in 1969, to date, none of the new AAPs can compare with it in effectiveness. Amiodarone accounts for about 25% of the total number of prescriptions for all AAPs.
Amiodarone has the properties of all four classes of AAP and, in addition, has a moderate α-blocking and antioxidant effect. However, the main antiarrhythmic property of amiodarone is the prolongation of the action potential and the effective refractory period of all parts of the heart.
However, the attitude of cardiologists towards amiodarone from the very beginning of its use for the treatment of arrhythmias was very contradictory. Due to the large list of extracardiac side effects, amiodarone, despite the fact that its high antiarrhythmic effectiveness was already known, was considered a reserve drug for quite a long time: it was recommended to use it only for life-threatening arrhythmias and only in the absence of effect from all other AAPs. The drug has gained a “reputation” as a “last resort”, used “only for the treatment of life-threatening diseases (LN Horowitz, J. Morganroth, 1978; JW Mason, 1987; JC Somberg, 1987).
After a number of studies, including CAST, it was revealed that while taking class I AAP, mortality in patients with organic heart disease can increase more than 3 times; It turned out that amiodarone is not only the most effective, but also the safest (after β-blockers) AAP. Numerous large controlled studies of the effectiveness and safety of amiodarone not only did not reveal an increase in overall mortality; on the contrary, a decrease in this indicator and the frequency of arrhythmic and sudden death was found. The incidence of arrhythmogenic effects, in particular torsade de pointes (TdP), while taking amiodarone is less than 1%, which is much lower than when taking other AAPs that prolong the QT interval. For comparison: the arrhythmogenic effect of sotalol hydrochloride in patients with ventricular arrhythmias is 4–5%, and the arrhythmogenic effect of foreign class I drugs reaches 20% or more. Thus, amiodarone has become the drug of first choice in the treatment of arrhythmias. Amiodarone is the only AAP, the use of which, according to renowned cardiologists, is considered the safest for outpatient treatment, even in patients with organic heart disease. The arrhythmogenic effect of amiodarone is rarely observed, and this does not allow us to identify a reliable connection between the occurrence of arrhythmogenic effects and the presence of organic heart damage (EM Prystovsky, 1994, 2003; LA Siddoway, 2003).
It should be emphasized that amiodarone is the only drug whose use is safe in heart failure. For any arrhythmias requiring treatment in patients with heart failure, amiodarone is primarily indicated. Moreover, in acute heart failure or decompensation of chronic heart failure with a high heart rate (sinus tachycardia or tachysystole in atrial fibrillation), when the use of β-blockers is contraindicated, and the administration of digoxin is ineffective and leads to dangerous consequences, a decrease in heart rate, improvement of hemodynamics and the patient's condition can be achieved with the help of amiodarone.
Side effects of amiodarone
As already noted, the main disadvantage of amiodarone is the likelihood of developing many extracardiac side effects, which, with long-term use of the drug, are observed in 10–52% of patients. However, the need to discontinue amiodarone occurs in 5–25% of patients (JA Johus et al., 1984; JF Best et al., 1986; WM Smith et al., 1986). The main side effects of amiodarone include: photosensitivity, skin discoloration, thyroid dysfunction (both hypothyroidism and hyperthyroidism), increased transaminase activity, peripheral neuropathies, muscle weakness, tremor, ataxia, visual impairment. Almost all of these side effects are reversible and disappear after discontinuation or reduction of the dose of amiodarone.
Thyroid dysfunction is observed in 10% of cases. In this case, subclinical hypothyroidism is much more common. Hypothyroidism can be controlled by taking levothyroxine. In case of hyperthyroidism, discontinuation of amiodarone is required (except for life-threatening arrhythmias) and treatment of hyperthyroidism (I. Klein, F. Ojamaa, 2001).
The most dangerous side effect of amiodarone is lung damage, causing interstitial pneumonitis or, less commonly, pulmonary fibrosis. According to various authors, the incidence of lung damage ranges from 1 to 17% (JJ Heger et al., 1981; B. Clarke et al., 1985, 1986). However, these data were obtained in the 1970s, when amiodarone was prescribed for a long time and in large doses. In most patients, lung damage develops only with long-term use of relatively large maintenance doses of amiodarone - more than 400 mg/day (up to 600 or even 1200 mg/day). In Russia, such doses are used extremely rarely; usually the maintenance daily dose is 200 mg (5 days a week) or even less. Currently, the incidence of “amiodarone-induced lung injury” is no more than 1% per year. In one study, the incidence of lung injury was no different between amiodarone and placebo (SJ Connolly, 1999; MD Siddoway, 2003). Clinical manifestations of “amiodarone lung damage” resemble an acute infectious lung disease: the most common complaint is shortness of breath, while a slight increase in temperature, cough, and weakness are observed. Radiologically, diffuse interstitial infiltration of the lung tissue is noted; localized changes can be observed, including the so-called “air-containing opacities” (JJ Kennedy et al., 1987). Treatment for amiodarone-induced lung injury involves discontinuation of amiodarone and administration of corticosteroids.
Basic amiodarone therapy regimens
It is necessary to dwell separately on some features of the use of amiodarone. For the antiarrhythmic effect of amiodarone to occur, a period of “saturation” is required.
Taking amiodarone orally. In Russia, the most common regimen for prescribing amiodarone is 600 mg/day (3 tablets per day) for 1 week, then 400 mg/day (2 tablets per day) for another 1 week, maintenance dose - 200 mg for a long time per day (1 tablet per day) or less. A faster effect can be achieved by prescribing the drug at a dose of 1200 mg/day for 1 week (6 tablets per day), then gradually reducing the dose to 200 mg per day or less. One of the regimens recommended in the international guidelines for cardiology Heart Disease (2001): taking amiodarone for 1–3 weeks at 800–1600 mg/day (i.e. 4–8 tablets per day), then taking 800 mg (4 tablets) for 2-4 weeks, after that - 600 mg / day (3 tablets) for 1-3 months and then switch to maintenance doses - 300 mg / day or less (titration depending on sensitivity patient to minimum effective doses).
There are reports of the effective use of high loading doses of amiodarone - 800-2000 mg 3 times a day (i.e. up to 6000 mg / day - up to 30 tablets per day) in patients with severe, life-threatening, refractory to other treatment methods ventricular arrhythmias with repeated episodes of ventricular fibrillation (ND Mostow et al., 1984; SJL Evans et al., 1992). A single dose of amiodarone at a dose of 30 mg/kg body weight is officially recommended as one of the ways to restore sinus rhythm in atrial fibrillation.
Thus, the use of large loading doses of amiodarone is relatively safe and effective. To achieve an antiarrhythmic effect, it is not necessary to achieve a stable concentration of the drug in the body. Short-term administration of large doses may be even safer than long-term administration of the drug at lower daily doses, and allows for rapid assessment of the antiarrhythmic effectiveness of the drug (LE Rosenfeld, 1987). During the “saturation” period, it can be recommended to take amiodarone at a dose of 1200 mg/day during the first week. After achieving the antiarrhythmic effect, the dose is gradually reduced to the minimum effective. It has been shown that effective maintenance doses of amiodarone can be 100 mg/day and even 50 mg/day (A. Gosselink, 1992; M. Dayer, S. Hardman, 2002).
Intravenous administration of amiodarone. The effectiveness of intravenous amiodarone has been less studied. When administered as a bolus intravenously, amiodarone is usually prescribed at a dose of 5 mg/kg body weight over 5 minutes. In recent years, slower intravenous administration of amiodarone has been recommended. With rapid administration, a decrease in the effectiveness of the drug may occur due to vasodilation, lowering blood pressure and activation of the sympathetic nervous system. One of the most popular intravenous amiodarone administration regimens is a bolus of 150 mg over 10 minutes, then an infusion at a rate of 1 mg/min for 6 hours (360 mg over 6 hours), followed by an infusion at a rate of 0.5 mg/min. However, there is evidence of safe and effective intravenous administration of amiodarone at a dose of 5 mg/kg body weight over 1 min or even 30 s (R. Hofmann, G. Wimmer, F. Leisch, 2000; DE Hilleman et al., 2002). The antiarrhythmic effect of amiodarone begins to appear within 20–30 minutes. Side effects with intravenous administration are rare and usually have no symptoms. 5% of patients have bradycardia, 16% have a decrease in blood pressure (LE Siddoway, 2003).
Interestingly, intravenous administration of amiodarone in its effect on electrophysiological parameters differs sharply from taking a loading dose of the drug orally. When conducting an electrophysiological study after intravenous administration, only a slowdown in conduction through the AV node (an increase in the AH interval) and an increase in the refractory period of the AV node are noted. Thus, with intravenous administration of amiodarone, only an antiadrenergic effect occurs (no class III effect), while after taking a loading dose of amiodarone orally, in addition to slowing conduction through the AV node, there is an increase in the duration of the QT interval and effective refractory periods in all parts of the heart (atria, AV node, His–Purkinje system, ventricles and accessory pathways). Based on these data, the effectiveness of intravenous amiodarone for atrial and ventricular arrhythmias is difficult to explain (HJJ Wellens et al., 1984; RN Fogoros, 1997).
Amiodarone is administered intravenously into the central veins through a catheter, since long-term administration into peripheral veins may cause phlebitis. When injecting the drug into peripheral veins, 20 ml of saline must be quickly injected immediately after the injection.
Published data suggest that intravenous amiodarone is more effective for ventricular tachyarrhythmias than lidocaine, bretylium tosylate, and procainamide.
Principles for selecting effective antiarrhythmic therapy
In the absence of contraindications, amiodarone is the drug of choice for almost all arrhythmias requiring antiarrhythmic therapy. The use of amiodarone is advisable for all types of supraventricular and ventricular arrhythmias. The effectiveness of AAP in the treatment of the main clinical forms of rhythm disturbances is approximately the same: in the treatment of extrasystole in most of them it is 50–75%, in therapy to prevent the recurrence of supraventricular tachyarrhythmias - from 25 to 60%, in severe ventricular tachycardias - from 10 to 40 %. Moreover, one drug is more effective in some patients, and the other in others. An exception is amiodarone - its effectiveness often reaches 70–80% even with arrhythmias refractory to other AAPs in this group of patients.
In patients with arrhythmias, but without signs of organic heart disease, the prescription of any AAP is considered acceptable. In patients with organic heart disease (post-infarction cardiosclerosis, ventricular hypertrophy and/or cardiac dilatation), the first choice drugs are amiodarone and beta-blockers. Numerous studies have found that the use of class I AAP in patients with organic heart disease is accompanied by a significant increase in mortality. Thus, amiodarone and β-blockers are not just the drugs of choice in patients with organic heart disease, but practically the only means for the treatment of arrhythmias.
Taking into account the safety of AAPs, it is advisable to begin assessing their effectiveness with β-blockers or amiodarone. If monotherapy is ineffective, the effectiveness of a combination of amiodarone and β-blockers is assessed. If there is no bradycardia or prolongation of the PR interval, any β-blocker can be combined with amiodarone.
In patients with bradycardia, pindolol (Wisken) is added to amiodarone. Coadministration of amiodarone and beta-blockers has been shown to significantly reduce mortality in patients with cardiovascular disease than either drug alone. Some experts even recommend implantation of a dual-chamber stimulator (in DDD mode) for safe amiodarone therapy in combination with beta-blockers. Only if there is no effect from β-blockers and/or amiodarone, class I AAPs are used. In this case, class I drugs are usually prescribed while taking a β-blocker or amiodarone. The CAST study showed that co-administration of β-blockers eliminated the negative effect of class I anti-inflammatory drugs on survival of patients with arrhythmias. In addition to class I drugs, it is possible to prescribe sotalol hydrochloride (a β-blocker with the properties of a class III drug).
Combinations of amiodarone and other AAPs
If there is no effect from monotherapy, combinations of amiodarone are prescribed not only with β-blockers, but also with other AAPs. Theoretically, of course, the most rational is considered to be a combination of drugs with different mechanisms of antiarrhythmic action. For example, it is advisable to combine amiodarone with class I drugs: propafenone, lappaconitine hydrobromide, etacizine. Class Ic drugs do not prolong the QT interval. The simultaneous administration of drugs that have the same effect on the electrophysiological properties of the myocardium seems dangerous. For example, amiodarone and sotalol hydrochloride prolong the QT interval, and the risk of QT prolongation and associated torsade de pointes (TdP) is considered to be increased when these drugs are taken concomitantly. However, in combination therapy with AAPs, they are prescribed in reduced doses. Therefore, we can expect both a lack of influence of combination therapy on the frequency of arrhythmogenic effects and a reduction in the frequency of undesirable effects. Of interest in this regard are the results of one study in which ibutilide (a drug that prolongs the QT interval, the incidence of torsade de pointes (TdP) reaches 8%) was administered to patients with recurrent atrial fibrillation who were chronically taking amiodarone. Restoration of sinus rhythm was achieved in 54% with atrial flutter and in 39% with atrial fibrillation. At the same time, in 70 patients, only one case of tachycardia of the “pirouette” type was noted (1.4%). It should be noted that in this study, ibutilide was not discontinued if QT prolongation or bradycardia occurred (K. Glatter et al., 2001). Thus, amiodarone may even reduce the risk of torsade de pointes (TdP) when combined with class III drugs. In this case, reports of cases of stopping tachycardia of the “pirouette” type with amiodarone, including in patients with congenital variants of QT interval prolongation, are explained. In addition, prolongation of the QT interval by 15% or more is one of the predictors of the effectiveness of amiodarone during long-term use.
An approximate sequence for selecting AAT for recurrent arrhythmias in patients with organic heart disease can be presented as follows:
- β-blocker or amiodarone;
- β-blocker + amiodarone;
- sotalol hydrochloride;
- amiodarone + AAP Ic (Ib) class;
- β-blocker + any class I drug;
- amiodarone + β-blocker + class Ic (Ib) AAP;
- sotalol hydrochloride + AAP Ic (Ib) class.
The use of amiodarone in certain clinical forms of arrhythmias
Since amiodarone is the most effective drug for almost all types of cardiac arrhythmias, and especially if it is necessary to prevent recurrent arrhythmias, the selection scheme for anti-relapse AAT is applicable for all recurrent arrhythmias, ranging from extrasystole to life-threatening ventricular tachyarrhythmias, up to “electrical storm” .
Atrial fibrillation. Currently, due to its high effectiveness, good tolerability and ease of administration, restoration of sinus rhythm in atrial fibrillation using a single oral dose of amiodarone is becoming increasingly important. The recommended dose for a single dose of the drug is 30 mg/kg body weight. The average time to restore sinus rhythm after taking this dose is about 6 hours.
GE Kochiadakis et al (1999) compared two schemes for the use of amiodarone to restore sinus rhythm during atrial fibrillation: 1) on the first day - oral administration of 2 g of amiodarone (500 mg 4 times a day), on the second day - 800 mg (200 mg each). mg 4 times a day); 2) intravenous drip administration of amiodarone: 300 mg over 1 hour, then - 20 mg/kg during the first day, second day - 50 mg/kg.
Restoration of sinus rhythm was noted in 89% of patients taking amiodarone orally (first regimen), in 88% with intravenous infusion of amiodarone (second regimen), and in 60% with placebo. With intravenous administration, several cases of decreased blood pressure and the occurrence of thrombophlebitis were observed. Taking amiodarone orally did not cause any side effects.
At the Department of Therapy of the Russian State Medical University, the effectiveness of a single oral dose of amiodarone (cordarone) at a dose of 30 mg/kg body weight for atrial fibrillation was studied. Restoration of sinus rhythm was achieved in 80% of patients. However, no significant side effects were noted (Dzhanashiya et al., 1995, 1998; Khamitsaeva et al., 2002).
Amiodarone is the most effective drug for preventing recurrence of atrial fibrillation. In a direct comparison with sotalol hydrochloride and propafenone, amiodarone was found to be 1.5 to 2 times more effective than sotalol hydrochloride and propafenone (CTAF and AFFIRM studies).
There are reports of very high effectiveness of amiodarone even when prescribed to patients with severe heart failure (NYHA classes III, IV): out of 14 patients, sinus rhythm was maintained for 3 years in 13 patients (93%), and out of 25 patients - in 21 (84%) within 1 year (AT Gosselink et al., 1992; HR Middlekauff et al., 1993).
Ventricular tachycardia. To stop ventricular tachycardia, it is recommended to use: amiodarone - 300-450 mg intravenously, lidocaine - 100 mg intravenously, sotalol hydrochloride - 100 mg intravenously, procainamide - 1 g intravenously. After restoration of sinus rhythm, if necessary, infusion of an effective AAP is performed.
The intervals between administration of each drug depend on the clinical situation. In case of severe hemodynamic disturbances, electrical cardioversion is performed at any stage. True, the authors of international recommendations for cardiopulmonary resuscitation and emergency cardiology (2000) do not recommend administering more than one drug, and if there is no effect from the first drug, they consider it advisable to immediately use electrical cardioversion.
The clinical effectiveness of amiodarone in preventing recurrence of ventricular tachyarrhythmias ranges from 39 to 78% (average 51%) (HL Greene et al., 1989; Golitsyn et al., 2001).
To characterize a particularly severe course of ventricular tachyarrhythmias, some “jargon” definitions are sometimes used, for example, “electrical storm” - recurrent unstable polymorphic ventricular tachycardia and/or ventricular fibrillation. Quantitative definitions, according to various authors, range from “more than 2 episodes in 24 hours” to “19 episodes in 24 hours or more than 3 episodes in 1 hour” (K. Nademanee et al., 2000). Patients with an “electrical storm” undergo repeated defibrillation. One of the most effective ways to overcome this severe complication is to prescribe β-blockers in combination with intravenous administration and oral administration of large doses of amiodarone (up to 2 g or more per day). There are reports of success using very large doses of amiodarone. For severe, refractory to drug therapy (ineffectiveness of lidocaine, bretylium tosylate, procainamide and other AAPs) and life-threatening recurrent ventricular tachyarrhythmias), amiodarone was successfully prescribed orally up to 4–6 g per day (50 mg/kg) for 3 days (i.e. . 20–30 tablets), then 2–3 g per day (30 mg/kg) for 2 days (10–15 tablets), followed by a dose reduction (SJL Evans et al., 1992). If patients with electrical storm respond to intravenous amiodarone and continue to receive oral amiodarone, the survival rate for these patients is 80% within the first year (RJ Fogel, 2000). When comparing the effectiveness of amiodarone and lidocaine in patients with ventricular tachycardia refractory to electrical cardioversion and defibrillation, amiodarone was significantly more effective in increasing the survival of such patients (P. Dorian et al., 2002).
The second term used to denote the severe course of tachycardia is the term incessant (“continuous”, “persistent”, “difficult to cure”, “unceasing”) - continuously recurrent monomorphic ventricular tachycardia of severe course. In this variant of the course of ventricular tachycardia, combinations of AAP are used, for example, amiodarone in combination with lidocaine, mexiletine or class Ia and Ic antiarrhythmics. There are reports of the effectiveness of blockade of the left stellate ganglion. There is also evidence of the high effectiveness of intra-aortic balloon counterpulsation. With this procedure, complete cessation of recurrent tachycardia is achieved in 50% of patients, and a noticeable improvement in tachycardia control is achieved in 86% (EC Hanson et al., 1980; H. Bolooki, 1998; JJ Germano et al., 2002).
Increased risk of sudden death. For a long period of time, the main method of treatment for patients at increased risk of sudden death was the use of AAP. The most effective way to select antiarrhythmic therapy was to assess its effectiveness using intracardiac electrophysiological studies and/or repeated 24-hour ECG monitoring before and after AAP administration.
In the CASCADE study, empirical amiodarone was also found to be much more effective in patients who had suffered sudden death than class I drugs (quinidine, procainamide, flecainide) selected using repeated electrophysiological studies and ECG monitoring (41% and 20%, respectively) .
It has been established that to prevent sudden death, it is most advisable to prescribe β-blockers and amiodarone.
In the CAMIAT study, the use of amiodarone in post-infarction patients was accompanied by a significant reduction in arrhythmic mortality by 48.5% and cardiovascular mortality by 27.4%. The EMIAT study noted a significant reduction in arrhythmic mortality by 35%. A meta-analysis of 13 studies of the effectiveness of amiodarone in post-infarction patients and patients with heart failure (ATMA) revealed a significant reduction in arrhythmic mortality by 29% and overall mortality by 13%.
The simultaneous administration of a β-blocker and amiodarone is even more effective. When taking a beta-blocker and amiodarone in patients who had myocardial infarction, there was an additional reduction in arrhythmic mortality by 2.2 times, cardiac mortality by 1.8 times and overall mortality by 1.4 times (EMIAT and CAMIAT studies). In some patient groups, amiodarone is as effective as implantable cardioverter defibrillators (ICDs) in reducing overall mortality.
ICD discharges are very painful (the pain experienced by a patient during an ICD discharge is usually compared to “a horse’s hoof hitting the chest”). Prescribing amiodarone to patients with ICD significantly reduces the frequency of defibrillator discharges by reducing the frequency of arrhythmias. The recent OPTIC study compared the effectiveness of beta-blockers, a combination of amiodarone and beta-blockers, and sotalol hydrochloride in reducing the incidence of ICD discharges. The combination of amiodarone and β-blockers was 3 times more effective than β-blockers alone and more than 2 times more effective than sotalol hydrochloride (SJ Connolly et al., 2006).
Thus, despite a number of disadvantages of the drug, amiodarone still represents the first choice AAP.
It should be noted that the use of generic forms of amiodarone is fraught with a lack of treatment effectiveness and the development of complications (JA Reiffel and PR Kowey, 2000). A study by S. G. Kanorsky and A. G. Staritsky revealed a 12-fold increase in the frequency of relapses of atrial fibrillation when replacing the original drug with generics.
In the US and Canada, approximately 20,000 hospitalizations could be avoided each year as a result of replacing amiodarone with generic versions (PT Pollak, 2001).
P. Kh. Janashia, Doctor of Medical Sciences, Professor N. M. Shevchenko, Doctor of Medical Sciences, Professor T. V. Ryzhova Russian State Medical University, Moscow
Instructions for use AMIODARONE
Medicines that can cause torsades de pointes are primarily class Ia and class III antiarrhythmic drugs and some antipsychotics. Hypokalemia is a predisposing factor, as is bradycardia or congenital or acquired prolongation of the QT interval.
Combinations with
- Drugs that can cause ventricular tachycardia of the “pirouette” type.
- Class Ia antiarrhythmic drugs (quinidine, hydroquinidine, isopyramide).
- Class III antiarrhythmic drugs (dofetilide, ibutilide, sotalol).
- Other drugs, such as bepridil, cisapride, difemanil, IV ritromycin, mizolastine, IV vincamine, moxifloxacin, IV spiramycin.
- Sultopride.
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases.
These contraindications do not apply to the use of amiodarone for cardiopulmonary resuscitation in cardiac arrest refractory to electrical defibrillation.
Not recommended combinations with
Cyclosporine
There may be an increase in the level of cyclosporine in plasma, associated with a decrease in the metabolism of the drug in the liver, with possible nephrotoxic manifestations.
Determination of the level of cyclosporine in the blood, checking renal function and reviewing the dosage during treatment with amiodarone and after discontinuation of the drug.
Diltiazem for injection
Risk of bradycardia and atrioventricular block. If a combination is unavoidable, strict clinical and continuous ECG monitoring should be established.
Verapamil for injection
Risk of bradycardia and atrioventricular block. If a combination is unavoidable, strict clinical and continuous ECG monitoring should be established.
Antiparasitic drugs that can cause torsade de pointes (halofantrine, pentamidine, lumefantrine)
If the combination is unavoidable, preliminary control of the QT interval and ECG monitoring is necessary.
Neuroleptics that can cause ventricular tachycardia of the “pirouette” type:
Some phenothiazine antipsychotics (chlorpromazine, cyamemazine, levomepromazine, thioridazine, trifluoperazine), benzamides (amisulpride, sulpiride, tiapride, veralipride), butyrophenones (droperidol, haloperidol), other antipsychotics (pimozide).
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases.
Methadone
The risk of ventricular rhythm disturbances (pirouette-type tachycardia) increases. Recommended:
- ECG and clinical observation.
Combinations requiring precautions when using Amiodarone with:
Oral anticoagulants:
Increased anticoagulation effect and risk of bleeding, due to increased concentrations of anticoagulants in plasma. The need for more frequent monitoring of the level of prothrombin in the blood and MHO (INR), as well as adaptation of doses of anticoagulants during treatment with amiodarone and after discontinuation of the drug.
Beta blockers, with the exception of sotalol (contraindicated combination) and esmolol (combination requiring caution when used)
Violations of contractility, automatism and conduction (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring.
Beta blockers prescribed for heart failure (bisoprolol, carvedilol, metoprolol)
Impaired contractility and conduction (synergistic effect) with the risk of developing severe bradycardia. Increased risk of ventricular arrhythmias, especially torsade de pointes.
Regular clinical and electrocardiographic monitoring is necessary.
Cardiac glycosides
Disorders of automaticity (excessive bradycardia) and atrioventricular conduction (synergism of action). When using digoxin, its concentration in plasma increases (due to decreased clearance of the alkaloid).
It is necessary to carry out clinical and ECG monitoring, as well as determination of plasma digoxin levels); It may be necessary to change the dose of digoxin.
Diltiazem for oral administration
Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG control.
Verapamil for oral administration
Risk of bradycardia and atrioventricular block, especially in the elderly. Clinical and ECG control.
Essex scraper
Violations of contractility, automatism and conduction (suppression of compensatory sympathetic mechanisms). Clinical and ECG monitoring.
Hypokalemic drugs: potassium-sparing diuretics (in monotherapy or combination), stimulant laxatives, amphotericin B (iv), glucocorticoids (systemic), tetracosactide.
The risk of ventricular rhythm disturbances increases, especially tachycardia of the “pirouette” type (hypokalemia is a predisposing factor). Clinical and ECG monitoring, laboratory tests.
Lidocaine
Risk of increased lidocaine plasma concentrations, with the possibility of neurological and cardiac side effects, due to amiodarone's decreased metabolism of lidocaine in the liver. Clinical and ECG monitoring, if necessary, dose adjustment of lidocaine during treatment with amiodarone and after its discontinuation.
Orlistat
Risk of decreased plasma concentrations of amiodarone and its active metabolite. Clinical and, if necessary, ECG monitoring.
Phenytoin (and, by extrapolation, fosphenytoin)
An increase in the level of phenytoin in plasma with symptoms of overdose, especially of a neurological nature (decreased metabolism of phenytoin in the liver). Clinical monitoring and determination of plasma phenytoin levels; if possible, reduce the dose of phenytoin.
Simvastatin
Increased risk of side effects (depending on dose) such as rhabdomyolysis (decreased metabolism of simvastatin in the liver). The dose of simvastatin should not exceed 20 mg/day.
If a therapeutic effect is not achieved at this dose, you should switch to another statin that does not interact with this type of interaction.
Tacrolimus
An increase in the level of tacrolimus in the blood due to inhibition of its metabolism by amiodarone. Measurement of tacrolimus blood levels, monitoring of kidney function and leveling of tacrolimus levels should be carried out.
Drugs that cause bradycardia:
Many drugs can cause bradycardia. This is especially true for class 1a antiarrhythmic drugs, beta blockers, some class III antiarrhythmic drugs, some calcium channel blockers, digitalis, pilocarpine and anticholinesterase agents.
Risk of excessive bradycardia (cumulative effect).
Combinations to Consider
Drugs that cause bradycardia:
- calcium channel blockers with bradycardic effect (verapamil), beta blockers (except sotalol), clonidine, guanfacine, digitalis alkaloids, mefloquine, cholinesterase inhibitors (donezepil, galantamine, rivastigmine, tacrine, ambemonium, pyridostigmine, neostigmine), pilocarpine.
Risk of excessive bradycardia (cumulative effects).
Incompatibilities
When PVC material or medical equipment plasticized with 2-diethylhexyl phthalate (DEHP) is used in the presence of amiodarone injection solution, DEHP may be released. To minimize exposure to DEHP, it is recommended that the solution be final diluted before infusion in DEHP-free equipment.