Painful periods are sometimes considered normal. Statistics say that 10-15% regularly experience severe pain during menstruation, and up to 70% of women of childbearing age periodically experience it. In fact, this is not the norm, but a violation of menstrual function, by correcting which you can get rid of pain.
The pain is not always localized in the lower abdomen. It can radiate to the lower back or pelvis
Symptoms
The main symptom of illness is cramping, aching, stabbing or other type of pain in the lower abdomen. It can radiate to the lower back, pelvis, perineum, and inner thighs. Most often, the peak of pain occurs in the first days of the cycle, then the intensity of the pain decreases.
Associated symptoms:
- general malaise, loss of interest in the outside world, decreased performance;
- nausea, diarrhea, other digestive problems;
- sudden mood changes, irritability, sleep disturbances, headaches;
- sweating, rapid heartbeat.
Painful periods often cause headaches
Galidor
This remedy not only relieves cramps during menstruation, but also has a slight sedative effect. The active substance of Galidor is bencyclane. This drug is prescribed not only for abdominal pain, but also for spastic headaches, renal colic and bladder spasms. "Halidor" is not the safest drug, therefore it is sold by prescription and prescribed exclusively by a doctor.
Galidor
Egis, Hungary
Vascular diseases: - peripheral vascular diseases - Raynaud's disease, other diseases with acrocyanosis and vasospasm, as well as chronic occlusive arterial diseases;
— cerebral vascular diseases: in complex therapy of acute and chronic cerebral ischemia. Elimination of spasm of internal organs: - gastrointestinal diseases - gastroenteritis of various etiologies (especially infectious), infectious and inflammatory colitis, functional diseases of the large intestine, tenesmus, postoperative flatulence, cholecystitis, cholelithiasis, condition after cholecystectomy, motility disorders with dyskinesia of the sphincter of Oddi, peptic ulcer of the stomach and duodenum (as part of combination therapy); - urological syndromes: spasms and tenesmus of the bladder, concomitant therapy for urolithiasis (in combination with analgesics for renal colic). Preparation for instrumental research methods in urology. from 370
527
- Like
- Write a review
Causes of painful menstruation
Depending on the reasons that cause painful periods (scientifically called algomenorrhea), doctors divide them into 2 types - primary and secondary algomenorrhea.
Primary algomenorrhea is spoken of when a reliable organic cause of painful menstruation is not identified during the examination. Its main causes are instability in the level of sex hormones and hormone-like substances and disturbances in the functioning of the nervous system. At this time, the contractility of the uterine muscle increases, as a result of which the uterine vessels are compressed, and the tissues do not receive sufficient nutrition. As a result, pain occurs. At the same time, due to malfunctions of the nervous system, sensitivity to pain increases, forcing patients to take painkillers. Primary algomenorrhea is most often observed in young girls who have just begun to establish their menstrual cycle. In many cases, a year or two after the first menstruation, when hormonal levels stabilize, the question of what to do with painful periods for a teenager disappears on its own.
Girls are more likely to suffer from pain caused by nerves and hormones
Prostaglandins are hormone-like substances, the imbalance of which is most often the cause of painful periods. In women suffering from primary algomenorrhea, the production of these substances increases significantly by the beginning of the menstrual cycle. Increased contractility of the uterine muscle, which causes pain, is caused precisely by an increased amount of prostaglandins.
- Secondary algomenorrhea occurs due to some disease. Most often, this is inflammation caused by fibroids, endometriosis, trauma, gynecological surgery (cauterization of erosion, cesarean section, excision of fibroids, etc.). The likelihood of developing secondary algomenorrhea increases when using an intrauterine device, abortion, after infectious diseases, or surgical interventions. The stomach begins to hurt 2-3 days before the start of menstruation and stops 2-3 days after their start. Since the main cause of pain does not disappear with the end of menstruation, it recurs periodically throughout the entire cycle. Women over 30 years of age most often suffer from secondary algomenorrhea.
- Another possible cause of painful periods is difficulty clearing the uterine cavity of secretions due to congenital or acquired anatomical features. The most common of them are too narrow cervical canal (congenital), fibroids (acquired). Pain during menstruation can also occur due to the fact that a small amount of blood is thrown into the abdominal cavity through the lumen of the fallopian tubes.
Painful menstruation may be caused by a cervical canal that is too narrow.
Menstrual pain should not be ignored. If the cause that causes them is not eliminated, in addition to unpleasant sensations and the consequences of a possible gynecological disease, you can experience a decrease in sexual desire and even infertility.
Ketoprofen
An excellent safe NSAID with minimal side effects, just like ibuprofen. The main thing is to observe the correct dosage and adhere to recommendations on contraindications. And although Ketoprofen is usually prescribed for diseases of the musculoskeletal system, it is also perfect for abdominal pain during menstruation.
Ketoprofen MV
Biocom, Russia
Articular syndrome (rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, gout);
symptomatic treatment of inflammatory and degenerative diseases of the musculoskeletal system (periarthritis, arthrosynovitis, tendonitis, tenosynovitis, bursitis, lumbago), pain in the spine, neuralgia, myalgia. Uncomplicated injuries, in particular sports injuries, sprains, sprains or ruptures of ligaments and tendons, bruises, post-traumatic pain. As part of combination therapy for inflammatory diseases of the veins, lymphatic vessels, lymph nodes (phlebitis, periphlebitis, lymphangitis, superficial lymphadenitis). from 169
179
- Like
- Write a review
What to do for pain during menstruation?
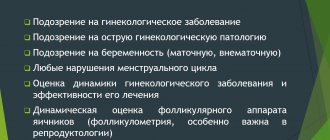
Your gynecologist should advise you on what to do if you experience severe pain during menstruation. Contact your doctor without waiting for the start of a new cycle to have time to take the necessary tests, smears, and undergo an ultrasound. The faster the cause of the phenomenon is determined, the faster you can make your life easier.
To reliably find out why painful periods are observed on the first day or throughout menstruation, after a standard examination, the doctor may prescribe:
- laboratory tests (smears);
- hysteroscopy - examination of the uterus with a special optical device that is inserted through the cervix;
- Ultrasound of the pelvic organs;
- diagnostic laparoscopy - examination of the uterus and fallopian tubes, during which an optical device is inserted through small incisions in the abdominal wall;
- hormonal profile study;
- tests for sexually transmitted diseases;
- blood test (checks for anemia).
To find out the cause of painful periods, your doctor may prescribe a hysteroscopy.
In some cases, to make a diagnosis. In addition to the gynecologist, you will have to consult with an endocrinologist and a neurologist. It is possible that you will have to change your method of contraception.
If the cause of painful periods is a gynecological disease, after recovery the pain should go away on its own.
Not only pills help to cope with primary algomenorrhea. Non-drug treatment methods are effective:
- general strengthening of the body: a good night's sleep, balance of physical and emotional stress, proper nutrition, quitting smoking, alcohol, strong tea, coffee;
- hardening, regular exercise (not for athletic performance, but for tone);
- physiotherapy: magnetic therapy, electrophoresis, diadynamics, ultrasound, massage, exercise therapy;
- acupuncture;
- taking courses of vitamins;
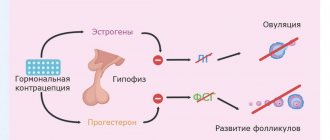
- hormone therapy. Combined oral contraceptives are used in low dosages, the intake of which adjusts the body to produce the correct amount of hormones. The minimum course is 3 months.
As an “ambulance”, the doctor may prescribe antispasmodics, analgesics, and sedatives. If the treatment package does not help, you will have to reconsider your contraceptive strategy and use non-steroidal anti-inflammatory drugs and progestins.
Result
When visiting the clinic, a woman receives effective treatment using high-precision equipment. There are also ongoing promotions, thanks to which the patient will save money. In addition, the clinic will not only effectively treat the disease, but also take the necessary tests. You can consult with various specialized doctors. The goal of the clinic is qualified medical care to achieve good health and improve the quality of life. If a woman is indicated to stay in a hospital setting, comfort will be ensured by modern equipment and new furniture. Thanks to this, the specialist is able to provide emergency assistance. The doctor gives recommendations. Namely: promptly and completely cure infectious and inflammatory disease of the pelvic organs. A woman needs to stop smoking and drinking alcohol. Maintain a healthy lifestyle, which includes proper nutrition (excludes fatty, smoked, fried, salty foods), and exercise. Carefully observe the rules of personal hygiene. Visit the gynecological office regularly (at least twice every 12 months).
Rules for taking painkillers
To avoid possible complications when taking painkillers during menstruation, you must follow several basic rules:
- Before you start taking it, you should consult your doctor and exclude contraindications:
- start taking the medicine with a minimum dose, gradually increasing it;
- do not exceed the recommended dose, no matter how severe the pain;
- do not take painkillers with alcohol, do not drink alcohol during the entire treatment course;
Memo for the patient
Every woman should know:
- You should not self-medicate, but seek help from a doctor if you have severe and regular headaches, as well as if there is a change in its nature and duration. Discomfort during the menstrual cycle and disruption of its flow are an important reason to consult a doctor, regardless of age.
- A healthy lifestyle and proper nutrition are the right decision. You can prevent the development of migraines by following a daily routine, regular walks before bed, maintaining physical activity, and getting enough sleep. In the diet, it is necessary to limit the consumption of “fast” carbohydrates, alcohol and foods that contribute to fluid retention in the body. Maintaining fluid balance is very important for women prone to headaches.
- For effective consultation with a neurologist (and other doctors), it is advisable to keep a diary of health observations, in which you should indicate not only the presence or absence of headaches, but also their intensity. Information about blood pressure, heart rate, and other indicators of well-being will not be superfluous.
- Follow all doctor's recommendations. These can be drugs of various effects, a therapeutic diet, maintenance therapy in the form of vitamin and mineral complexes. You should go for a therapeutic massage of the back and cervical-head region only on the recommendation of your attending physician.
At the Clinical Brain Institute, you can undergo a full examination to identify the causes of headaches during menstruation and prevent the occurrence of migraine attacks. We have highly qualified specialists and the most modern equipment. Our doctors will conduct an examination and prescribe effective treatment.
Prevention
Sometimes it is enough just to change your habits a little to forget about this unpleasant condition forever.
Don't get too cold
This golden rule for preventing diseases of the genitourinary system works great in this case. Dress according to the weather, insulate the pelvic area in winter, no short skirts in cool weather. Strong local and general immunity will help you forget about bladder inflammation.
Maintain hygiene
Choose skincare products that do not cause irritation and regularly cleanse the genital area in a front-to-back motion. This reduces the risk of microflora from the anus and vagina entering the urethra.
Choose the right underwear
Synthetics and thongs can provoke inflammatory processes in the urogenital area. Natural cotton underwear, on the contrary, helps maintain a healthy microclimate in the intimate area.
Go to the toilet on time
Ignoring the body’s signals “in a small way” is fraught with excessive concentration of urine, loss of sediment and the onset of an inflammatory process against the background of reduced immunity and accumulation of blood in the uterine cavity.
Avoid physical inactivity
A sedentary lifestyle provokes a whole cascade of disorders in the body. This includes the occurrence of inflammation in the genitourinary system before or during the onset of the monthly female cycle. Regular physical activity, exercise and 10,000 steps a day will help you forget about this problem.
Be attentive to yourself and your health!
- Tyuzikov I.A. Hormonal mechanisms of the pathogenesis of chronic recurrent cystitis in women as a promising pharmacotherapeutic option for disease management 2021. — (date of access: 06/26/2021).
- Guide to urology / ed. ON THE. Lopatkina. 1998
- Zaitsev A.V., Kasyan G.R., Spivak L.G. Cystitis, 2021 - (date of access: 06/26/2021).
- Khalilova U.A. Skvortsov V.V. Ismailov I.Ya. Lugovkina A.A. Proleyskaya N.A. Cystitis, 2021 — (date of access: 06/26/2021).
- Ivanov V.V. Herbal medicine for acute cystitis / V.V. Ivanov, V.E. Khitrikheev // Bulletin. East Siberian Scientific Center of the Siberian Branch of the Russian Academy of Medical Sciences. - 2010. - No. 3. - P. 72–75.
- Instructions for use of the drug PHYTOLYSIN® Paste for the preparation of suspension for oral administration
Treatment of menstrual pain by type of disease
The main goals of treatment are to eliminate pain, normalize the menstrual cycle, normalize the state of the autonomic system and eliminate organic causes of dysmenorrhea. The approach to therapy is developed for each woman individually, based on the primary disease.
- in case of endometriosis, surgical intervention is performed to eliminate foci of endometrial growth;
- in case of hormonal imbalance, it is necessary to take hormonal medications to correct the corresponding disorder;
- infectious and inflammatory processes are usually treated with antibiotics;
- when the pelvic veins are dilated, vasoconstrictor medications are prescribed;
- neoplasms in the pelvis require surgical removal with a biopsy to determine their benignity;
- adhesions in the pelvic organs are also removed through surgery.
Whatever the cause of the disturbing symptom, the doctor will try to solve the problem using conservative methods, and only if absolutely necessary will resort to surgery.