“Asystole” literally means “absence of systole” or cardiac arrest. Simply put, this is a state of clinical death. There are 2 possible variants of sudden fatal rhythm disturbances - ventricular fibrillation and asystole. It is impossible to distinguish them in the clinic, and there is no time, since there are only a few minutes for survival.
At this time, a person’s life is in the hands of the people around him and depends entirely on the desire and ability to provide first aid. According to research by resuscitators, 2/3 of cases of sudden death that occur in different places on the street occur from ventricular asystole.
Why does the heart stop?
The most common cause of cardiac arrest is chronic or acute diseases with a severe stage of decompensation and organic changes in the myocardium. Depending on the cardiac pathology, all causes are divided into primary and secondary. Primary cardiac diseases include:
- acute widespread myocardial infarction and its complications (cardiogenic shock, pulmonary embolism, aneurysm rupture);
- sudden disturbances in the rhythm of ventricular contraction (paroxysm of atrial fibrillation, ventricular tachycardia, some types of ventricular extrasystoles);
- rupture of aortic aneurysm;
- heart defects in the stage of decompensation;
- acute cardiovascular failure.
Risk factors contributing to asystole include:
- elderly age;
- excess weight;
- concomitant diabetes mellitus;
- drinking alcohol and smoking;
- increased blood cholesterol levels;
- When comparing gender, men are the most disadvantaged.
Secondary causes can occur suddenly in young people, without myocardial damage. They are caused by diseases such as:
- sudden stroke with extensive damage to the cerebral cortex;
- respiratory failure caused by long-term unresolved severe asthmatic condition;
- damage to internal organs in the coma stage with renal and liver failure, diabetes mellitus, leukemia, anemia;
- malignant tumors in the terminal phase.
In addition to diseases, secondary causes can be caused by accidents or injuries:
- suffocation due to foreign body entering the larynx or bronchi;
- poisoning by chemicals and poisons;
- drowning;
- extensive injuries in emergency situations, during man-made and other disasters, in everyday life, accompanied by traumatic shock;
- massive burns;
- large blood loss;
- electrical injury due to high voltage current.
Extracardiac causes
Represented by a large group of phenomena leading to secondary asystole:
- Pneumothorax. Penetration of air into the chest. Normally, it is sealed, which ensures the existence of organs in ideal conditions. Atmospheric gases provoke compression of the heart and lungs. They reduce the efficiency of hemodynamics, and in the long term even lead to the impossibility of normal functioning of cardiac structures. This is not an axiom; there is no 100% probability of such an outcome. Depends on the case and the volume of air penetrated.
- Hypoxia. Disruption of normal gas exchange in tissues. It leads to cardiac asystole relatively rarely, only if the process reaches a certain critical point. This requires a severe disease of the respiratory system or heart. Emergency care requires restoration of normal organ function. But in the case of severe somatic illness, the prospects are pessimistic.
- Electrical injury. Normally, cardiac structures work autonomously: they themselves generate an impulse, conduct it, and contract. As a result of exposure to a significant current, a disruption of the normal rhythm is observed. This ends with the sinus node first generating a signal chaotically, and then stopping producing it altogether. Spontaneous contractions of the ventricles continue for several seconds, then asystole occurs - cardiac arrest.
- Increased blood acid level. Biochemical abnormality. Occurs as a result of metabolic disorders. Relatively rarely leads to such a terrible phenomenon.
- Poisoning with salts of heavy metals, antihypertensive drugs, sleeping pills, tranquilizers, cardiac glycosides, psychotropic medications, insect poisons and others. Intoxication leads to blockage of cellular respiration, acute ischemia of cardiac structures and primary asystole occurs. The organ cannot cope with such loads, activity drops to zero. Recovery is possible, but the likelihood is minimal.
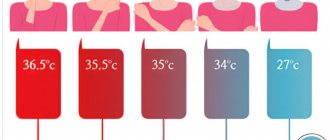
- Decrease in body temperature to critical levels. Thermometer readings below 35 degrees Celsius are deadly. Urgent measures can be effective.
- Excessive amount of potassium in the blood. Not associated with alimentary (food) factor. Normally, excess elements are evacuated from the body naturally. There is also a serious metabolic disorder here. Which one is a question for an endocrinologist.
- Changes in glucose levels. Both a decrease (hypoglycemia) and an increase in the indicator against the background of uncompensated diabetes are dangerous. Cardiac arrest is a relatively common consequence. A drop in sugar carries an even greater danger, since there is much less time for resuscitation.
- Advanced liver failure. As a result of cirrhosis or an oncological process. Ends with multiple organ dysfunction.
- Deviations in kidney function in the terminal phase.
- Cancer in the last stages with many metastases. The reason is intoxication and organ destruction.
What is asystole in medicine? We are talking about cardiac arrest. The prospects for restoration of activity depend on the underlying process. Organic ones have the worst prognosis.
Asystole in the form of attacks
A special pathology of the heart disrupts the conduction of impulses from the sinus node to the ventricles. It is called atrioventricular or atrioventricular block. Similar changes are formed in diphtheria, rheumatic carditis and other inflammatory diseases of the heart muscle, post-infarction scars. In addition, the excessive inhibitory influence of the vagus nerve should be taken into account.
The complete rupture of communication between the atria and ventricles depends on the degree of organic (scar) changes in the tissues. Impulses from the ventricles are not regulated by the sinus node and are characterized by a rare rhythm (bradycardia up to 25–30 beats per minute). The ECG reveals pauses in myocardial contraction.
Arrows indicate missing ventricular contractions
Symptoms of temporary asystole:
- when the heart stops in 3 seconds. the person feels dizzy;
- at 9 sec - fainting appears;
- 15 sec. - epileptiform seizure, clinical death is possible.
Cardiac causes of asystole
This group of factors causes primary asystole, that is, associated with electrical instability of the myocardium itself, often against the background of ischemia (oxygen starvation of tissues).
Heart attack
General acute malnutrition of muscle structures. It occurs as a result of long-term coronary insufficiency, atherosclerosis, thromboembolism and other phenomena of this kind.
The development of cardiac asystole is a consequence of extensive damage, if the area reaches more than 25% or about a similar value. Possible delayed development. Thus, some patients suffer from cardiac arrest within a few days.
The most dangerous period is the first 72 hours. Further, the risks decrease, but remain throughout life, since a heart attack does not go away without a trace.
Cardiosclerosis, persistent heart failure, these are the reasons for the possible development of asystole. Lifelong maintenance treatment and constant monitoring of the condition are indicated.
Decrease in the amount of blood circulating in the body
It has a dual nature. On the one hand, there is a possibility of classic bleeding, when liquid connective tissue leaves the closed system. Then the physical variety takes place.
On the other hand, everything can be more complicated. Against the background of pathologies of the mitral valve and aorta, incomplete ejection and movement in a large circle are possible. Hence the decrease in the amount of circulating blood against the background of a preserved nominal volume.
This is no less dangerous, rather the opposite: transfusion in such a situation is pointless, the problem is of an organic nature.
Cardiac tamponade
Accumulation of blood around. Liquids are also possible. The result of an injury, long-term swelling, and inflammatory process. Recovery is carried out surgically as a matter of urgency.
Pulmonary embolism
Refers to cardiac causes conditionally. The essence of the phenomenon is the blockage of a large vessel with a blood clot.
It can be either a result of the chest injury itself or a consequence of distant damage to anatomical structures (in a large circle the blood clot moves throughout the body and penetrates the pulmonary artery).
It is also possible that spontaneous rupture of small vessels may occur due to the use of anti-inflammatory drugs, corticosteroids, hematological conditions, or excessive thickening of fluid connective tissue.
Such problems are resolved before urgent processes arise. The chances of survival from thromboembolism are almost zero.
Features of asystole in children
All of the above reasons apply to children, but an important difference from adults is a special type of asystole, which is included in the general concept of “sudden infant death syndrome.” In this case, cardiac arrest is recorded in a child more often under the age of 5 months against the background of sleep and the absence of any diseases during this period.
It is believed that ventricular asystole in a baby is caused by underdevelopment of myocardial cells, impulse transmission pathways. Perhaps it is associated with the pathological course of pregnancy and labor in the mother:
- hypoxia (lack of oxygen) in the fetus due to anemia, diseases of the maternal body;
- asphyxia during childbirth;
- vacuum extraction of the fetus;
- multiple pregnancy;
- the birth of a premature baby;
- smoking and alcohol consumption by the expectant mother.
Contributing factors are:
- placing the baby on a soft mattress;
- unventilated hot room;
- many blankets covering the child and causing him to overheat;
- tight swaddling.
Sleeping in the prone position is one of the risk factors for asystole
Many causes of death in a newborn due to asystole are associated with the lack of proper care for the child by adults.
Prognosis and possible complications
The outcome depends on the quality of first aid, the timing of transporting the patient to the hospital and the resuscitation scheme.
Against the background of severe organic pathologies, thromboembolism, cardiogenic shock, intoxication with dangerous poisons, the probability of death is almost 100%. In other cases, the risks are slightly lower. It is possible to return the patient in 30-50% of situations.
Consequences:
- Death is the most common outcome.
- Neurological deficit, its nature depends on the focus. The type of manifestations resembles the period after a severe stroke.
- Brain death. Equal to biological cessation of existence. Cardiac activity is present, natural processes are also carried out, but these are vegetative moments.
Clinical manifestations
Symptoms of cardiac arrest are characterized by a sudden death clinic and are accompanied by respiratory arrest. Let's consider possible options for the conditions for detecting a patient.
- Option 1 - an outwardly ordinary person at work or on the street, in transport suddenly falls, hoarse, rare breathing escapes from the throat, lips and face turn blue, there is no consciousness, attempts to make contact are unsuccessful.
- Option 2 - fatal cardiac arrest occurs during sleep, and the patient lies down and looks like a normal sleeping person. Those around him do not immediately notice his lack of any reactions.
In both cases, the patient does not have time to call for help or complain about deteriorating health.
- Option 3 - the patient is being treated in a specialized department for heart disease in a general ward, he is allowed to walk, or he forces the regime on his own. He can fall in the corridor, in the ward, on the stairs. Symptoms correspond to clinical death.
- Option 4 - the patient is in the acute stage of a heart attack or with severe somatic lesions, trauma, is in the intensive care unit, the condition is monitored by a monitor, the ECG picture is constantly monitored, any deviation in the rhythm activity is indicated by a sound signal.
The last option is the most favorable in terms of providing the necessary assistance.
Doctors in a specialized department do not need to waste time searching for a pulse; all equipment for resuscitation is usually at hand
Not every passerby can find the pulse on the carotid artery (at the angle of the lower jaw) or verify the absence of a heartbeat. Usually the first place is given to:
- loss of consciousness;
- pallor and cyanosis of the face;
- lack of breathing movements.
Characteristic symptoms
Subjectively, the phenomenon makes itself known only in the initial period. Harbingers of organ stoppage:
- Sharp chest pain. It happens that the symptom is absent, depending on the root cause. Breathing disorders. As they say, it takes your breath away. The patient cannot take in air.
- Panic arises, a feeling of fear of death. Motor activity persists for several tens of seconds or a couple of minutes.
- Tachycardia, other forms of rhythm disturbances.
- Weakness, drowsiness.
- Headache, vertigo.
- Nausea and vomiting.
- Loss of consciousness as a result.
In many cases (approximately 50%) there may be no previous symptoms. Then everything happens quickly, the patient does not even have time to react.
Objective signs after fainting can only be tracked by those around you.
- Breathing disappears completely.
- Cardiac activity may be recorded, but it is false activity.
- The blood circulation has already stopped. Possible forms are tachycardia, atrial fibrillation. After a few minutes they disappear too.
- There is also no vascular pulsation.
If this happens in a hospital, the heart rate is assessed. With asystole, the ECG shows minimal physical activity (in the first minutes), then the graph degenerates into a straight line.
The symptoms are specific, but without preparation a person is capable of little. There is too little time to react.
Desirable algorithm for the action of a random passerby
Since a person’s life depends on the speed of first aid, any passerby must be able to navigate the indications and the severity of the victim’s condition.
Recommended:
- Stimulate the victim, shake him, slap him on the cheeks, speak loudly. If a person regains consciousness, this indicates a short-term disturbance of cerebral circulation. Accordingly, you need to try to ensure free breathing, a position with a low head end.
- If there is no reaction to the intervention, then you should try to feel the pulsation of the carotid artery, if it is impossible to listen to the heartbeat, by placing your ear to the chest.
- You need to call for help. Someone must call an ambulance and help carry out emergency measures.
When you see a fallen person, you should not pass by; your family and friends may find themselves in the same situation.
What emergency assistance is needed to restore rhythm?
Emergency care should:
- ensure heart contractions;
- maintain breathing;
- prevent hypoxia of the brain and other organs.
For brain cells, the decisive period is the first 8 minutes, after which the restoration of functions is doubtful.
The person should be laid on a hard surface (on the floor, a board made of boards, the ground) since subsequent compression of the chest on a soft surface is ineffective.
Tilt the victim's head back and check the patency of the airway with your finger; it is necessary to free the oral cavity from food debris, dentures, and other foreign bodies.
Air is blown into the patient's mouth or nose while one of the holes is clamped. With effective passive inspiration, chest rise is visible.
At the same time, for each “inhalation,” 4–5 intense pushes are made with two palms on the chest.
The force must be balanced against the potential for fracture of the ribs and sternum
Indirect massage is carried out until the ambulance arrives or until a pulse appears.
Medical assistance
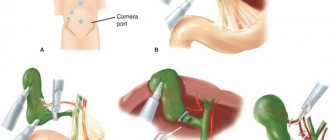
Treatment of asystole with medical methods begins in the ambulance and continues in the intensive care unit. Depending on the equipment, the ambulance doctor continues indirect massage with simultaneous ventilation of the lungs with an Ambu bag, injects adrenaline intracardially and tries to act with a defibrillator discharge.
Intensive activities should be carried out within 30 minutes. In a specialized department, the patient is transferred to mechanical breathing. Other medications are injected into the subclavian vein to support brain functions (alkaline solution, Dopamine, Reopoliglucin, Sodium oxybutyrate).
A cardiac monitor connected to the patient allows you to monitor the results of the staff’s actions. If ineffective, biological death is declared.
Resuscitation measures are not carried out for patients with asystole caused by severe chronic heart disease or malignant tumors.
Prevention measures
It is impossible to prevent an emergency condition with a 100% guarantee. Even healthy people are at risk, although to a lesser extent.
Possible actions:
- Quit smoking, alcohol, and especially drugs. Heroin and cocaine, ethyl alcohol, nicotine, tar, all these substances have a depressing effect on the myocardium. The result may be delayed, against the background of imaginary well-being.
- Adequate physical activity. Hiking, amateur cycling, swimming, exercise therapy. You can't overwork yourself. Lack of training in itself turns out to be an increased risk factor.
- Complete nutrition. Fortification of the diet. From the point of view of diet, the abuse of fatty, fried, in a word, “junk” food is not as dangerous as a lack of vegetables, fruits, and protein in the menu. It makes sense to discuss the diet with your doctor, depending on the underlying disease. Specialist - nutritionist.
- Sleep 8 hours per night. Lack of normal rest leads to overstrain of all the body's forces. Especially in the long term. The body can work like this for a year or two, but at some point it will fail.
It is important to systematically treat the underlying pathology, which can cause ventricular or atrial asystole. Regular (1-2 times a year) visits to a cardiologist are also an important measure.