Today, inflammatory diseases occupy a leading position in the frequency of diagnosis among all other gynecological pathologies. It is the symptoms caused by them that are the reason for visiting the gynecologist in 60-65% of cases, but more often, unfortunately, women self-medicate or do not at all attach importance to changes in the condition of the genital organs. But many of them can lead to serious complications, inflammation of other organs, infertility and a number of other undesirable consequences. Therefore, gynecologists around the world urge women to be more attentive to their health and not only not to neglect annual preventive examinations, but also to immediately consult a doctor if the nature of the discharge changes, itching in the genital area and other changes occur.
What are inflammatory diseases of the genital organs and their types
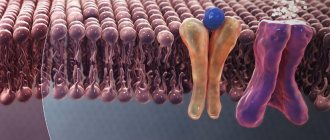
Inflammation is a process that is a natural reaction of the body to an irritant, mechanical damage or penetration of pathogenic microorganisms into tissues. It is aimed at destroying the irritating factor, eliminating the consequences of its negative impact on tissues and restoring their integrity. This is accompanied by redness of the tissues, swelling of varying degrees, pain, dysfunction and sometimes increased temperature.
Infectious processes today are of leading importance in the development of inflammatory processes of the external and internal genital organs.
In the latter case, when the inflammatory disease is a consequence of an infection, they are divided into:
- nonspecific - provoked by opportunistic microflora, which include streptococci, staphylococci, enterococci, Klebsiella, Escherichia coli, fungi of the genus Candida, etc.;
- specific - caused by infection with absolute pathogens, in particular gonococci, trichomonas, chlamydia, mycoplasma.
Thus, if the main route of infection with absolute pathogens is unprotected sexual intercourse, then nonspecific inflammatory diseases can also occur against the background of their absence due to decreased immunity, non-compliance with personal hygiene rules, disturbance of vaginal pH as a result of douching and other procedures, etc. Mixed infections are detected.
Expert Opinion of a Doctor
Inflammatory diseases of the uterine appendages are a complex and practically important problem associated with serious medical, social and economic losses. This pathology can lead to disruption, first of all, of the functions of both the reproductive and other organs and systems of the female body. In the structure of gynecological diseases, inflammatory processes of the female genital organs occupy a leading place, accounting for 65% of all pathologies of the reproductive system in women.
Women's inflammatory diseases
Experience:
Ask a Question
In this case, the female reproductive system is formed by the external genitalia and internal:
- vulva - the outer part of the genital organs, formed by the labia majora and minora and the vestibule of the vagina;
- vagina - a tubular organ lined with mucous membrane into which the cervix opens;
- cervix - one end opens into the vagina, and the other into the uterine cavity, the cervical canal passes inside it;
- the uterus is a hollow muscular organ that ensures pregnancy;
- ovaries - paired endocrine organs connected to the uterus through the fallopian tubes, where already at the time of the birth of a girl the entire supply of follicles with eggs is present;
- Fallopian (uterine) tubes are hollow tubular formations that ensure the passage of a mature egg at the time of ovulation from the ovary into the uterine cavity.
In the area of the labia, directly next to the vagina, there are paired glands called Bartholin's glands. They provide the production of secretions to moisturize the vaginal opening.
Each of these organs, when favorable conditions are created, can become a victim of inflammation. On the basis of which all gynecological inflammatory diseases are divided into those affecting the lower and upper parts of the genital organs. The first include:
- vulvitis;
- bartholinitis;
- colpitis;
- endocervicitis;
- cervicitis.
Among the inflammatory pathologies of the upper genital organs there are:
- endomyometritis;
- salpingo-oophoritis;
- pelvioperitonitis;
- parametritis.
All of them can occur in an acute form, when symptoms arise suddenly, quickly intensify and are generally pronounced, or in a chronic form, when signs of the disease of varying severity are observed again and again with a certain frequency. Also, gynecological inflammatory diseases can occur in a subacute form, which is characterized by a blurred clinical picture of the pathology.
Symptoms of tertiary syphilis
This type of disease is diagnosed extremely rarely. It develops 4-5 years after infection and is characterized by damage to the skin, mucous membranes, bones and internal organs. Over time it leads to death.
The symptoms are as follows:
- the appearance of brown or red-brown plaques on the skin. They have an uneven outline, rise above the skin, and are covered with ulcers and crusts. Localization – arms, back, face;
- formation in the subcutaneous tissue of an isolated gumma - a hard node the size of a walnut and an ulcer in the center. It usually occurs on the scalp, chest, face, and sometimes on the mucous membranes of the mouth, larynx and nose. In the latter case, tissue destruction and deformation of the palate occurs. Against this background, a number of complications develop:
- the nasal septum is destroyed and the nose is deformed;
- hoarseness and hoarseness appear;
- tongue mobility is impaired.
- damage to the nervous, vascular and skeletal systems, which manifests itself in the form of syphilitic meningitis, hydrocephalus, progressive paralysis;
- deformation and dysfunction of internal organs (liver, kidneys, lungs, heart).
Reasons for the development of inflammatory processes in the female genital organs
Normally, the vaginal microflora is very diverse, which provides natural protection against infection. It contains lacto- and bifidobacteria, which are also called Dederlein's bacilli. They account for 90-95% of all normal vaginal microflora in women of reproductive age.
These microorganisms break down glycogen, which is present on the surface of the epithelial cells of the vaginal mucosa, resulting in the formation of lactic acid. It ensures the maintenance of an optimal acidic environment for the vagina with a pH in the range of 3.8-4.5, in which many microorganisms die, and therefore cannot cause infection and the development of the inflammatory process. Therefore, any manipulations, including the use of antibacterial or antimicrobial agents, that change the level of acidity in the vagina, can create the preconditions for the development of inflammatory diseases.
Normally, the pH in the vagina is higher in girls before puberty and in postmenopausal women, since the number of lactobacilli directly depends on the level of estrogen.
The remaining 5-10% are staphylococcus epidermidis, enterococci, hemolytic and non-hemolytic streptococcus. Normally, the vaginal microflora may also contain E. coli, yeast-like fungi, ureaplasma and mycoplasma, but due to the fact that the number of lacto- and bifidobacteria significantly exceeds their number, opportunistic microorganisms are not able to multiply and provoke the development of inflammatory diseases. Thus, the vaginal flora is a dynamic and completely self-regulating system, any interference in which can lead to the development of nonspecific inflammatory processes.
Expert Opinion of a Doctor
Undoubtedly, the most important cause of inflammatory diseases of the genitals are various microorganisms that penetrate the genital tract of women. Also, general diseases contribute to the occurrence of inflammatory diseases of the uterine appendages; great physical activity and mental stress; stressful situations; allergic reactions. Extreme concern is caused by the steady increase in sexually transmitted diseases, especially the so-called latent infections caused by chlamydia, ureoplasma, and mycoplasma.
Women's inflammatory diseases
Experience:
Ask a Question
In addition to the irrational use of antibacterial and antiseptic agents, violations of the rules of hygiene procedures, the following can provoke inflammation:
- transmission of other infectious diseases, including acute respiratory viral infections and others, leading to a decrease in immunity;
- hormonal disorders;
- incorrect selection of hormonal contraceptives, including intrauterine devices;
- taking a number of medications (cytostatics, antibiotics).
Even if microorganisms managed to provoke inflammation in the lower parts of the genital organs, the cervical canal, which normally has virtually no lumen, is designed to protect the upper parts from involvement in the pathological process. In addition to its natural narrowness, the cervix contains a large amount of mucus, saturated with nonspecific protective factors. Thanks to it, the vast majority of pathogens cannot penetrate the uterus further and provoke inflammation.
However, infections and inflammatory diseases of the uterus, ovaries and fallopian tubes are also common. Their occurrence is facilitated by:
- intrauterine manipulation, including diagnostic curettage, abortion, removal of tumors, etc.;
- sexual intercourse during menstruation, when the cervical canal expands for natural reasons and loses some mucus;
- childbirth;
- surgical interventions on the pelvic and abdominal organs;
- chronic infections;
- stress;
- hypothermia.
All this can lead to changes in the natural mechanisms of protection of the internal genital organs and create favorable conditions for their infection by opportunistic or pathogenic microorganisms with the subsequent development of an inflammatory disease.
Treatment
Conservative therapy
The list of therapeutic measures is determined by the etiology of pain in the vagina:
- Vaginitis.
Antibacterial, antiviral and antifungal agents of general and systemic action are recommended. Antiseptic ointments and vaginal suppositories, disinfectant solutions, sitz baths with herbal decoctions, potassium permanganate solution, and furatsilin are used. - Endometriosis.
The leading role is played by hormone therapy using agonists of gonadotropic releasing hormones, gestagens, antigonadotropic and combined estrogen-progestogen drugs. It is possible to prescribe medications with anti-inflammatory effects, analgesics, antispasmodics, and immunostimulants. - Dyspareunia.
In the presence of causative organic pathologies, local anesthetics, hormone replacement therapy, sedative and anti-inflammatory drugs, physiotherapy, and gynecological massage are used. For psychogenic dyspareunia, psychocorrection is carried out using various techniques. - Prolapse of the uterus and vagina.
A special diet, Kegel exercises, gymnastics according to Atarbekov, and estrogen-containing drugs are indicated. Individually selected gynecological pessaries are used to support the organs. - Malignant neoplasms.
Photodynamic therapy, chemotherapy or radiation therapy using interstitial, intracavitary or external irradiation are required.
Surgery
Taking into account the nature of the disease, the following surgical interventions can be performed:
- Traumatic injuries:
suturing of vaginal ruptures, opening of submucosal hematomas, removal of foreign bodies, laparotomy and revision of the abdominal cavity with combined damage to several organs. - Endometriosis:
laparoscopic endocoagulation, excision of retrocervical endometriosis, organ removal interventions for common pathology in patients of the older age group. - Organ prolapse:
colporrhaphy, vaginopexy with MESH prosthesis, sling operations, colpocleisis, various options for vaginoplasty. - Hematocolpos:
emptying and sanitation of hematocolpos, hymenotomy, excision of the vaginal septum, vaginoplasty, excision of the wall of the “blind” vagina. - Fistulas:
excision of rectovaginal, urethro-vaginal and vesicovaginal fistulas, levatoroplasty, sphincteroplasty. - Volumetric formations:
removal of a benign tumor, excision of a cyst, electroexcision, vaginectomy and hysterectomy for malignant neoplasia.
Inflammatory diseases of the external genitalia
Such diseases are not common and do not pose a serious threat to a woman’s health. These include vulvitis and bartholinitis. However, they also require timely diagnosis and treatment. Otherwise, the inflammatory process can become chronic, which will be much more difficult to cope with in the future.
Vulvitis
Vulvitis is an inflammation of a woman's external genitalia. It extremely rarely occurs in isolation and in the vast majority of cases develops against the background of existing inflammation of the vaginal mucosa, cervical canal, and uterine appendages.
Primary vulvitis is usually characteristic of women with diabetes mellitus, as well as those suffering from obesity, which leads to poor hygiene of the external genitalia and the formation of diaper rash and mechanical injury.
Typical symptoms of the disease are:
- itching and burning in the vulva area;
- swelling and redness of the external genitalia;
- purulent discharge;
- enlarged inguinal lymph nodes.
Sometimes this is accompanied by a slight change in general condition. In any case, to treat vulvitis, it is necessary to initially eliminate the primary inflammatory disease (vaginitis, endometritis, adnexitis). For isolated inflammation of the vulva, external use of antibacterial ointments and antiseptics is indicated. Antihistamines may be prescribed to reduce itching.
Bartholinitis
Bartholinitis is an inflammation of the Bartholin glands, which leads to blockage of their ducts. The process can be one- or two-way. This is accompanied by swelling, redness and severe pain of the gland, which takes on the appearance of a tumor. If left untreated in the early stages, an abscess forms, so when pressure is applied to the glands, pus may be released. This is accompanied by a deterioration in the general condition, in particular weakness, chills, and fever.
Treatment of bartholinitis is carried out by prescribing antibiotics and painkillers. Anti-inflammatory ointments should be applied directly to the inflamed gland. If an abscess has already formed, opening it is indicated, which quickly leads to an improvement in well-being and the disappearance of throbbing pain.
Symptoms of secondary syphilis
The development of the secondary stage begins 2 months after the formation of compacted papules. The following symptoms may be observed:
- general malaise: headache, tinnitus, dizziness, poor appetite, high body temperature (up to 380C), pain in bones and joints, insomnia, nausea, vomiting, confusion. Speech disturbances and epileptic seizures may occur;
- dysfunction of internal organs (in 25% of cases): damage to the myocardium, liver, stomach, kidneys, membranes and blood vessels of the brain;
- loss of hair, eyelashes and eyebrows. Hair growth resumes after 1-2 months;
- the appearance of condylomas on the genitals and in the anal area;
- the occurrence of rashes on the skin, including the palms and soles of the feet, and mucous membranes.
The following types of rash are distinguished:
- syphilitic roseola - pink or pale pink flat spots from 0.5 to 1 cm in diameter. Localization – trunk and limbs;
- lenticular syphilide - copper-red round formations with a dense structure, rising above the skin;
- meliary syphilide - small dense formations with a diameter of up to 2-2.5 mm. They are brown in color and localized on the skin of the body. As a rule, such papules accumulate and form rings, arcs or plaques;
- coin-shaped syphilide - large red or brown formations with a diameter of up to 2.5 cm, slightly raised above the skin;
- weeping syphilide - eroded formations. They are moist, round in shape, and cause moderate itching. Localization – groin area and axillary folds;
- Condylomas lata are soft, pale pink formations that rise above the skin and are similar in appearance to papillomas. Localization – perineum and area around the mouth;
- pustular syphilide - small purulent formations with a yellowish crust at the end. Localization - on the skin of the trunk, limbs and face.
Usually after 3-5 weeks the rashes suddenly disappear, leaving no trace, even if no treatment was carried out. This period is called secondary latent syphilis. This stage lasts up to 5 years. During this time, relapses of the disease are observed, the rash appears again, but later also disappears on its own.
The course of the first wave of rashes is pronounced: multiple skin lesions, formations of a bright shade. Subsequently, darker elements are observed, often accumulating in groups.
Inflammatory diseases of the vagina and cervical canal
Inflammation of the vagina is much more common than that of the external genitalia. Moreover, they can be provoked by a variety of microorganisms, which determines the differences in their course and treatment features.
Bacterial vaginosis
Bacterial vaginosis, or, as it is also called, vaginal dysbiosis, cannot be called a full-fledged disease, but its presence creates clear preconditions for the development of more severe infectious processes. With it, there is a decrease in the number of lactobacilli and an increase in the number of opportunistic microorganisms. This leads to an increase in pH to 7.0-7.5, which destroys the natural defense mechanism against infections.
Bacterial vaginosis is found in 21-33% of women.
With bacterial vaginosis the following is observed:
- an increase in the volume of discharge, which has a uniform consistency, but can acquire the smell of rotten fish and stick to the walls of the vagina;
- itching and burning in the vagina;
- discomfort during sexual intercourse.
A characteristic sign of the disease is the detection of key cells in smear microscopy, a decrease in the number or complete absence of Dederlein rods and the detection of leukocytes.
Treatment of bacterial vaginosis consists of using antimicrobial agents, vitamins, and then restoring normal vaginal microflora with the help of special probiotics in the form of suppositories. There is no need to abstain from sexual intercourse during treatment, but you should use a condom when contacting a new partner to avoid contracting other infections.
Nonspecific vaginitis or colpitis
Nonspecific vaginitis is called inflammation of the vaginal mucosa, provoked by invasion of microorganisms or the action of chemical, mechanical or thermal factors. Most often it is caused by representatives of opportunistic microflora and may be a consequence of an increase in their virulence, i.e., the ability to cause pathological processes, against the background of decreased immunity.
Colpitis is characterized by the appearance of:
- itching and burning in the vagina;
- purulent or serous-purulent discharge;
- discomfort during sexual intercourse;
- swelling and redness of the vaginal mucosa;
- formation of pinpoint hemorrhages on the mucous membrane in places where it is touched (in severe cases, the formation of erosions and ulcers is possible).
Colpitis is often combined with vulvitis, urethritis, and endocervicitis.
Nonspecific vaginitis can become chronic. In such situations, patients also experience itching and burning in the vagina, but the intensity of the sensations is much lower than with acute colpitis. As a rule, the reason for a visit to the gynecologist in such cases is copious serous-purulent discharge.
Treatment of colpitis is always comprehensive and at the same time aimed at destroying the causative agents of the disease, eliminating concomitant diseases, and strengthening the immune system. Therefore, patients are advised to use antibacterial and antimicrobial drugs in the form of suppositories, sometimes hormonal agents, as well as probiotics to restore normal flora and acidity.
Vaginal candidiasis
Vaginal candidiasis is one of the most common infectious diseases of the genital organs. Its causative agent is yeast-like fungi of the genus Candida, which are single-celled aerobic microorganisms. Popularly, this disease is often called thrush.
Vaginal candidiasis is not considered a sexually transmitted disease (STD), since different strains of Candida can live in the vagina constantly, but become active only when favorable conditions are created for them (a slightly acidic environment, decreased immunity). But the development of candidiasis is very often a marker of the development of STDs. Therefore, if it is detected, it is recommended to get tested for STDs.
Signs of thrush are:
- severe itching and burning in the vagina, which tends to intensify after water procedures, sexual intercourse and at night;
- cheesy discharge from the genital tract;
- swelling and redness of the mucous membranes of the vagina;
- the presence of a characteristic white, thick coating on the walls of the vagina.
In acute vaginal candidiasis, involvement of the vulvar mucosa in the inflammatory process is observed. This may be accompanied by the formation of vesicles, which rupture with the formation of erosions in their place.
Very often, due to self-medication, candidiasis becomes chronic. In such situations, the disease regularly recurs and is difficult to treat. Therapy for thrush consists of prescribing antifungal drugs, as well as eliminating factors contributing to its development. Therefore, women are advised to stop taking COCs, corticosteroids, cytostatics, and antibiotics, if possible. To eliminate acute vaginal candidiasis, it is enough to use local remedies, but for a chronic inflammatory process, systemic medications will be required. In any case, the choice of specific antifungal agents should be based on the results of bacterial culture with determination of the sensitivity of the detected fungi to various active substances with antifungal activity.
Trichomonas vaginitis
Trichomonas vaginitis is also a common problem of our time. It is already classified as an STD, since the causative agent of the disease, Trichomonas vaginalis, is an aggressive pathogenic microorganism and is normally absent from the vaginal microflora. They affect sperm motility, therefore, in the presence of Trichomonas vaginitis, the possibility of pregnancy is extremely low.
60-70% of women have encountered trichomonas vaginitis at least once in their lives.
Very often, trichomonas vaginitis is combined with other STDs, including gonorrhea, viral diseases, chlamydia, etc. In most cases, the infection does not extend beyond the vagina, although it can affect the cervical canal, the uterus, and the organs of the urinary system.
Trichomonas can serve as a container for other pathogenic microorganisms, for example, gonococci, ureaplasma, chlamydia, etc. Therefore, after their destruction, the development of gonorrhea, chlamydia, and ureplasmosis, respectively, is possible.
Typical symptoms of the disease are:
- itching and burning in the vagina;
- a large amount of foamy discharge;
- increased urge to urinate and pain (if Trichomonas affects the urethra).
The incubation period can range from 3 to 30 days.
Treatment of trichomonas infection is prescribed to all sexual partners. Be sure to avoid sexual intercourse during the procedure. The essence of therapy is the prescription of specialized antimicrobial drugs, as well as the treatment of all other detected infections.
Endocervicitis
Endocervicitis is an inflammatory process in the cervical canal that develops against the background of injury to its mucous membrane during manipulations on the uterus or during childbirth. It often accompanies other inflammatory processes of a gynecological nature, in particular colpitis, adnexitis, endometritis, and the cervical canal mucosa itself is very sensitive to gonococci and chlamydia. Also, endocervicitis often occurs against the background of the development of non-inflammatory diseases, including ectropion of the cervix, ectopia and others.
It is characterized by the appearance of mucopurulent discharge, which is sometimes accompanied by nagging pain in the lower abdomen. During the examination, the gynecologist may detect swelling and redness of the mucous membrane of the vaginal part of the cervix, erosion. If a woman delays seeing a doctor and starting treatment, inflammation of the cervical canal can lead to the development of cervicitis, which will also involve the muscular layer of the cervix, which will provoke the formation of so-called nabothian cysts.
If the cause of inflammation is gonococci, they speak of the presence of gonorrhea, but if it is provoked by chlamydia, it is urogenital chlamydia. From the cervical canal, microorganisms can penetrate the uterus and fallopian tubes, causing their inflammation. Gonorrhea is characterized by purulent discharge, the consistency of which resembles cream. Chlamydia is accompanied by serous-purulent discharge.
Treatment of endocervicitis consists of prescribing antibiotics taken orally. The use of local remedies in such situations is not indicated due to the high risk of infection spreading to the upper genital organs.
Prevention of female diseases
There is no magic pill. No one will ever give you a guarantee that you will be able to avoid this or that disease, but you can still reduce the risks of their development.
- Stop smoking. Smoking is a serious provocateur of the development of various diseases.
- Lead an active lifestyle. Stable activity helps avoid the development of congestion in the pelvis, significantly reduces the risk of obesity and helps improve overall tone.
- Maintain healthy sexual activity. Avoid contact without barrier contraception with untested partners.
- Don't forget about a healthy diet and drinking regime. Fruits, vegetables, dairy products, fish and seafood support not only reproductive health, but also overall health.
- Get preventive examinations every six months. This does not require much time and effort, but in this way you can reduce the risks of developing severe pathologies.
- Sign up for a preventive examination with a gynecologist at a medical clinic in Moscow. With us you can take all the necessary tests and get maximum information about your health. You can read reviews about gynecologists at our medical centers on our website.
Take care of yourself!
Inflammatory diseases of the pelvic organs
Inflammation in the uterus and appendages is a serious situation that requires immediate treatment, since with chronic infections there is a risk of not only spreading to other abdominal organs, but also the formation of adhesions. In the future, they will become a significant obstacle to pregnancy and its normal course.
Expert Opinion of a Doctor
It is very important for a woman to regularly visit an obstetrician-gynecologist, at least 2 times a year. If you have the slightest complaint about pathological discharge from the genital tract, discomfort in the area of the external genital organs, pain in the lower abdomen, you must immediately consult a doctor in order to identify the cause in time, carry out correct treatment and, thereby, prevent the development of complications from the reproductive system, which cause inflammatory diseases of the uterine appendages.
Women's inflammatory diseases
Experience:
Ask a Question
Endometritis
Endometritis is a gynecological disease in which the uterine mucosa becomes inflamed during intrauterine procedures, after childbirth, or as a result of ascending infection. As a rule, it is characterized by an acute onset, which is accompanied by:
- fever;
- chills;
- purulent discharge from the genital tract.
With adequate treatment, the inflammatory process subsides after 8-10 days. In its absence, severe complications may develop, including peritonitis, thrombophlebitis, abscess formation, or chronic inflammatory process.
Chronic endometritis can also develop against the background of frequent curettage of the uterine mucosa or prolonged use of intrauterine contraceptives. It may not cause such pronounced symptoms of inflammation, but provoke menstrual irregularities and nagging pain in the lower abdomen.
Uterine fibroids
Uterine fibroids are one of the most common benign tumors in women. It often occurs precisely at the most active flowering age - after 30-35 years. The proliferation of cells that form a myomatous node occurs for various reasons. This may be a hereditary predisposition, hormonal imbalance. Myoma can occur in response to a negative impact, for example, after a serious inflammatory process.
The tumor forms “quietly”, without any special symptoms. Only a doctor can detect it during a gynecological examination. To clarify the diagnosis, it is necessary to perform an ultrasound; sometimes CT and MRI are used. After the examination, the doctor determines the further treatment strategy. Most often it is non-operative and combined.
An indication for surgery may be the “term” of fibroids: a tumor over 12 weeks must be removed. Tumors that grow too quickly, cause excessive bleeding, and therefore can cause anemia, are also surgically removed.
It is important to remember that the presence of fibroids can affect the ability to bear a child: it is more difficult for a fertilized egg to attach to the wall of the uterus.