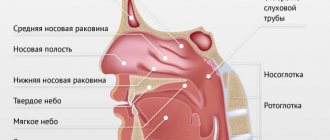
Adenoids are glands consisting of lymphoid tissue, similar to tonsils. Unlike the tonsils, they cannot be seen when you open your mouth because they are located above the roof of your mouth. Adenoids grow during childhood and begin to shrink around age 8. In adults they are very small or absent. When the adenoids become too large (adenoid hypertrophy), they can cause an obstruction in the passage of air through the nose.
Adenoids, like tonsils, perform the function of producing lymphocytes and antibodies, helping the body protect itself from microorganisms that penetrate the nasal and oral cavity. Along with the palatine tonsils, they provide immune protection, which is especially important in childhood.
In some cases, the functions of the adenoids are disrupted: after repeated bacterial or viral attacks, this tissue increases excessively in volume (hypertrophy occurs), which is the cause of the appearance of characteristic symptoms. In children, inflammation of the adenoids is a common pathology leading to breathing problems and other complications that should not be overlooked.
Types of disease
Adenoid hypertrophy is classified depending on the degree of nasopharyngeal obstruction:
- I degree (obstruction less than 25%). Adenoid vegetation has spread to 1/3 of the nasopharynx and vomer. Difficulty breathing and discomfort are possible only at night when the child is sleeping.
- II degree (damage from 25% to 50% of lymphoid tissue). Accompanied by severe difficulty in nasal breathing during the daytime. The child does not sleep well at night due to snoring.
- III degree (between 50% and 75%). Adenoid vegetations are observed in most of the nasopharynx, completely covering the vomer. In rare cases, adenoids protrude into the lumen of the pharynx. The child breathes exclusively through the mouth, as nasal breathing becomes impossible.
Children with adenoid hypertrophy or recurrent adenoiditis usually have, in addition to symptoms of respiratory distress, signs of recurrent otitis media, chronic sinusitis, and persistent rhinitis.
Age-related features of adenoids (age of adenoid hypertrophy)
It is noteworthy that adenoid lymphoid formations reach their maximum development in preschool age from 1.5-2 to 5-6 years, when the child begins to actively contact the outside world, attend preschool institutions, clubs, sections, and visit places large crowds of people: shops, public transport, cinema, theater, circus, etc. In this case, an exchange of microflora inevitably occurs with surrounding people, including pathogenic ones; in response to this, the adenoids react with inflammation, and as a result, their enlargement. Thus, there is a tireless “training” of the immune response to the action of the infectious agent. That is why in preschool age the adenoids in their physiological norm will be of the 2nd degree of hypertrophy (they occupy ½ of the lumen of the nasopharynx). As a rule, up to 1.5-2 years of age, adenoids are less than grade 1, they are still underdeveloped and do not cause any problems. But at this age a child has much less contacts, and they are limited to family members. If the family does not have many children, then before the child starts attending kindergarten, he either does not get sick at all, or no more than 1-2 times a year. After 8-10 years, adenoids undergo involution (reduction in size); by 12-14 years, most children will not have adenoids when examined. But the lymphoid cells will move to the back wall of the pharynx and will retain their protective role all their lives. This is why it is so important to preserve the immune organ and avoid removal during the “adenoid” (preschool) age.
Symptoms of enlarged adenoids
Because the adenoids trap germs that enter the body, sometimes the tissue becomes temporarily inflamed (as if it were swelling) in an attempt to fight off the infection. Often inflammation of the adenoids, called adenoiditis, is accompanied by tonsillitis and pharyngitis.
Clinical signs of adenoiditis in children are associated with three factors: a mechanical obstruction that occurs when the nasopharyngeal tonsils are enlarged, the development of an infectious process and a violation of reflex connections.
Inflamed or infected adenoids make breathing difficult and lead to the following problems:
- stuffy nose, which causes breathing through the mouth;
- snoring and problems with night sleep, which leads to daytime lethargy, weakened memory, fatigue and decreased performance at school;
- inflammation of the lymph nodes in the neck;
- hearing problems;
- quiet, monotonous and nasal voice (“nasal”).
The pressure of lymphoid tissue on the vascular structures of the mucous membrane leads to the appearance of edema and the development of a persistent runny nose. This makes nasal breathing even more difficult.
In infancy, hypertrophy of the adenoids is fraught with difficulty sucking, which is accompanied by systematic underfeeding and malnutrition. In this case, there is a decrease in blood oxygenation, which leads to the development of hypoxia.
If these signs appear, it is recommended to show the child to a specialist in the field of otolaryngology. The sooner measures are taken, the greater the chances of a complete recovery and the absence of complications.
This is new material, but Tiger Cub once wrote on this topic - “Adenoids”.
(Please note that the information contained in an earlier article may not be entirely current.) Now we invite you to familiarize yourself with the modern view of this problem.The article was prepared by otorhinolaryngologist of the Tiger Cub Children's Clinic Ramazanova Gunay Alniyazovna
ENT doctors are sounding the alarm: every 2nd child has problems with adenoids. If you look closely at children in older kindergarten groups and first-graders, you can easily notice those suffering from adenoids - such children breathe through their mouths. It would seem that there is nothing wrong. But, if you do not intervene and let everything take its course, then adenoids can cause not only constant colds, but also such serious complications as purulent otitis media and hearing loss. Until recently, the only method to solve the problem was surgery. Today, doctors have found a way to do without surgery.
What are adenoids and why do they become a problem?
Adenoids are located behind the nose, in the nasopharynx. In childhood, adenoid and lymphoid tissue protects us from infections. Normally, by the age of 14, the adenoids, having fulfilled their function, disappear by themselves. This occurs under the influence of sex hormones. It is extremely rare that adenoids persist in adults.
Adenoiditis most often “blooms” in children aged 5 to 7 years. It is during this “transitional age,” when a child becomes a schoolchild, that the number of lymphocytes in the blood decreases, which leads to a decrease in the body’s resistance to infections and viruses. This period is physiological. To protect the body, the adenoids increase in size. Unfortunately, in many children this causes the adenoids to block the nasopharynx and make breathing difficult.
Lymphoid tissue can also become a focus of infection. Viruses and bacteria enter the nasopharynx through the nose and onto the adenoid tissue. The adenoids begin to fight the infection. If the fight is unequal, then the adenoids become inflamed. And in this case, the adenoids themselves become a source of infection. Due to the fact that the auditory tubes are located next to the adenoids, festering adenoids can provoke otitis media. This scenario is one of the most dangerous. Purulent otitis, exudative otitis can lead to hearing loss for life.
Frequent colds and infectious diseases are just the tip of the iceberg. Constant, so-called “habitual” mouth breathing leads to a number of disorders of the internal organs. Habitual mouth breathing is characterized by non-closure of the lips, changes in the position of the tongue, which affects the position of the dentition and bite. Which in turn can lead to the development of serious problems of the entire musculoskeletal system (hence problems with posture) and will have a negative impact on all organs and systems of the body.
How to break this vicious circle?
Nasal breathing is very important for a child. A growing body needs oxygen more than adults. If you teach your child to breathe through his nose again, then all of the above problems can be avoided. But how to do that? After all, the child begins to breathe through his mouth forcibly.
Due to the fact that the adenoids cover the invisible part of the nostrils at the back, the so-called “choanae,” the child cannot breathe through his nose. Even if he inhales through his nose, the adenoids block the exit to the nasopharynx, blocking the air. Therefore, children begin to breathe through their mouths. In frequently ill children, the nasal mucosa and the adenoids themselves swell, which makes breathing even more difficult. A common picture: a child goes to kindergarten or school and encounters infections there. What happens in the body? The adenoids enlarge compensatoryly, blocking the choanae, and the child begins to breathe through the mouth. It turns out to be a vicious circle - mouth breathing leads to frequent infections, and in response to infections the adenoids enlarge. The problem is that until the child learns to breathe through his nose, the adenoids will not shrink. Such children need to be weaned from mouth breathing. It's not easy, but it's possible. Newborn babies can only breathe through their nose - this is vital during the sucking process.
Mouth breathing is a bad habit! A healthy person should breathe only through the nose. When breathing through the mouth, the amount of oxygen entering the human body is only 78% of the normal volume, and with chronic mouth breathing, hyperventilation of the lungs develops. A mouth-breathing child inhales every 3 seconds. For this reason, 10 times more pathogens enter the body through the nasal passages.
If the child breathes through the mouth, treatment is necessary. But first you need to determine the cause of mouth breathing.
When is surgery needed?
If endoscopy of the nasopharynx has not been performed, tympanometry and the doctor during a routine examination says: an adenotomy is needed - this is the wrong approach. In the 21st century, you need to do a full examination. If the child is restless and it is impossible to perform an endoscopy, then at least a CT scan or x-ray of the nasopharynx should be done. Without an endoscopy or x-ray, a doctor cannot adequately assess what exactly is causing the problem. Brain hernia? Tumor? Or is it still adenoids? Endoscopy of the nasopharynx eliminates such questions.
Alarming symptoms: ✓ The child does not breathe through his nose. The mouth is almost always slightly open. ✓ Frequent diseases: acute respiratory infections, flu, colds, bronchitis, tonsillitis, laryngitis, sore throat. ✓ Exudative otitis media - frequent otitis, especially purulent ones, can be a consequence of problems with the adenoids. ✓ Apnea syndrome (snoring with pauses in breathing during sleep), when the child seems to “freeze” for several moments.
Apnea syndrome in children is very dangerous. If there are frequent purulent otitis media and there is “freezing” in sleep, you still need to remove the adenoids surgically. If there are no pauses in breathing during sleep, then the child can and should be treated conservatively.
✓ Malocclusion and crowded dentition. ✓ Problems with diction.
If there is at least one of the signs, then you should contact a specialist. And best of all - to several. An interdisciplinary approach, when doctors from different specialties work together to solve one problem, is optimal in this case. A child with mouth breathing should definitely be examined not only by an ENT specialist, but also by an orthodontist. Very often the help of a speech therapist is required.
Treatment of adenoids without surgery: how does it work?
You need to pay attention to the shape of the jaws. The upper jaw and hard palate are the anatomical floor of the nose. If the jaws narrow, the volume of the nose decreases and the person cannot breathe fully. After the examination, the doctor selects special removable devices made of medical silicone for the child - myofunctional orthodontic trainers. On the upper and lower jaw. During the entire treatment period (up to six months), the child must sleep with the trainers and wear them during the day for 1 hour, every day. In addition, breathing exercises and exercises for the perioral muscles and tongue are prescribed. The trainer gradually, very gently, acts on the jaws and forces them to take a physiologically correct position, stimulating their growth and development. The air flow through the nasal passages improves - air circulates freely during inhalation and exhalation. In the process of such treatment, the upper respiratory tract is formed correctly, the lumen of the upper respiratory tract in the area of the pharyngeal tonsil increases. Children stop snoring and begin to breathe normally through their nose.
Wearing trainers in combination with breathing and muscle exercises teaches the child to close his lips at rest, since the tone of the orbicularis facial muscle and the lip-closure reflex are stimulated. The child gets used to the trainer within 10-14 days. The exercises take 5-10 minutes and are easy to remember and perform. The first results become visible after 3-6 months. This is expressed, first of all, in a decrease in the incidence of acute respiratory infections, influenza, and otitis media.
86% of exudative otitis media are cured only by wearing trainers and exercises. This has been proven. No medications, physical therapy, procedures or rinses are required.
It should be noted that not all orthodontists provide treatment using trainers and exercises. There are several reasons for this. Firstly, you need to motivate the child, which is not easy. Secondly, orthodontists have other methods of treating malocclusion, such as braces. Therefore, I recommend contacting multidisciplinary centers where specialists work together, not pulling the “blanket” over themselves, but acting in the interests of the patient.
Sometimes parents bring their children to us with a referral for surgery. But after examination, we choose conservative treatment. In a very large percentage of cases, surgery is not necessary. If the adenoids do not completely block the access of air and the child can still breathe through the nose, the situation can be corrected without surgical intervention.
If you can’t do without surgery, then you don’t need to be afraid either. Today, adenotomy is performed under general anesthesia using an endoscope and laser. Laser radiation coagulates the vessels, so the operation is not as “bloody” as it was before. The entire operation lasts 30 minutes and the child goes home the same evening. The notorious “individual approach” is needed. Several home diagnostic methods.
During sleep. Wait until your child is deeply asleep. And watch. I ask the parents of my little patients to make a 30-second video and then evaluate the frequency of breathing during sleep, is there snoring and breathing pauses? Video shooting should be done in such a way that the lips are visible - are they slightly open or closed? If the mouth is slightly open by 1-2 millimeters, this is already mouth breathing. Already need to sound the alarm! Without such observations, you will not be able to understand whether a child has apnea. With such a video recording, your attending physician will understand the clinical picture more clearly. Show him the video.
While awake. Pay attention to the child when he is very interested in the game: he assembles construction sets, draws. Watch how he breathes. Are his lips parted? When a child is deeply busy, for example, watching cartoons, and opens his mouth slightly, this is also a signal that there is weakness of the perioral muscles. And that means these muscles need to be trained. Otherwise, this situation can also lead to enlarged adenoids, changes in bite and other serious problems. The mouth must always be covered unless we are eating, drinking or talking!
How does your child hear? Until the age of 10, a child, as a rule, does not complain of hearing. Even if he doesn't hear well. Notice how loud he watches cartoons? Does he ask you to turn it up loud? Does he ask again? Does it happen that you cannot reach your child - it’s as if he doesn’t hear you? Hearing loss is a serious symptom that must be addressed as early as possible.
Possible complications of the disease
If treatment of the inflammatory process in the adenoid area is not started in time, there is a risk of developing serious health consequences.
The most common complications of inflammation of the adenoids in children:
- weight loss/stunted growth;
- sleep apnea (the child stops breathing for a while);
- sinusitis (inflammation of the maxillary sinus);
- headaches, neuroses;
- partial and temporary deafness due to obstruction of the eustachian tube;
- otitis media and a feeling of stuffiness in the ears;
- impaired swallowing and sense of smell.
In children, adenoid hypertrophy can cause the tongue to move forward, the upper teeth to protrude, and the face to elongate. The adenoid type of face is characterized by a poorly developed jaw, short upper lip, raised nostrils and a curved palate.
A high incidence of middle ear infections is associated with Eustachian tube obstruction. The proximity of the adenoids to this structure explains the relationship between these diseases. Inflammation of the adenoids can lead to Eustachian tube obstruction, which results in the accumulation of infected fluid in the middle ear. This is fraught with the development of recurrent otitis media and other respiratory infections.
Modern diagnostic methods (endoscopic examination of the ear, nose and throat by an ENT doctor)
The gold standard for diagnosis (and the only correct one) is an endoscopic examination of the nasopharynx by an ENT doctor with good skills and experience working with children from birth. An endoscopic examination is an examination using a video camera, with additional powerful lighting and magnification and display on a television screen, on which both the doctor and the child’s parents will clearly see not only all the structures of the nose, but also the nasopharynx with the mouths of the auditory tubes and adenoid vegetations. In this case, the doctor will evaluate the degree of their increase, inflammation of the mucous membrane, the nature of the discharge, the presence and size of the respiratory lumen. The examination is carried out with a special children's nozzle - a tube less than 3 millimeters in diameter, the examination is non-contact, absolutely painless, does not require special preparation (the ENT doctor only drips vasoconstrictor drops in an age-appropriate dosage before the examination) and has no contraindications and is used in children from birth.
Of course, with such a diagnosis, digital examination is not required.
It is very important that during an endoscopic examination of the ears, such a significant complication as exudative otitis (accumulation of fluid behind a healthy, non-inflamed eardrum) will not be missed. Thanks to good lighting and magnification, the eardrum is transparent during endoscopic examination, so the liquid and air bubbles behind it are clearly visible. Whereas when examined in the usual way, the eardrum, if it is not inflamed, reflects the light of a flashlight and looks gray and opaque, the liquid behind it cannot be seen.
Comparative characteristics of traditional examination of ENT organs and endoscopic examination of ENT organs
| Criteria | Traditional ENT examination | Endoscopic examination of ENT organs |
| Price | Low inspection costs due to the use of tools and a reflector | High cost due to the use of expensive equipment |
| Painless | The contact method can be unpleasant due to the instrumental expansion of the entrance to the nose for examination; the use of an ear mirror is also contact. Digital examination is traumatic and can be painful | The method is non-contact, painless, as nozzles of less than 3 mm are used. in diameter |
| Diagnostic reliability | The examination is superficial, the structures of the nose are examined only in the anterior sections, the nasopharynx is inaccessible for inspection, the adenoids and the mouths of the auditory tubes are not visible, it is impossible to assess the condition of the middle ear behind a healthy eardrum | The reliability of diagnosis of adenoiditis, adenoid hypertrophy, and complications in ENT organs is 100%. All structures of the nose, nasopharynx, ear and throat are examined on a screen with additional magnification and lighting. A diagnostic error has been ruled out. |
| Accuracy of the diagnosis | The diagnosis is presumptive | Reliable diagnosis with assessment of possible risks and complications |
| Purpose of treatment | Overdiagnosis, high probability of prescribing antibacterial therapy “just in case” | Prescribing adequate therapy |
| Assessment of dynamics during treatment | Assessment of only external signs and symptoms (presence of runny nose, cough, etc.) | Assessment of both the dynamics of symptoms and mucus and size of the adenoids, development or relief of complications. |
| Recommendations for adenoid removal | It is possible to prescribe removal of adenoids if they can be preserved and monitored. | Appointment of adenoid removal only if there are indications for removal and an objective assessment of the lack of effect of treatment. |
| Who can carry out diagnostics | Pediatrician, ENT doctor with any experience and qualifications | ENT doctor with practical skills and experience in endoscopic examination of ENT organs in children from birth. |
Laboratory diagnostic methods (the goal is to clarify the cause of chronic adenoiditis and/or adenoid hypertrophy)
To establish the cause of enlarged adenoids, as a rule, a detailed blood test is prescribed, a nasal smear for cytology (cellular composition of nasal discharge), blood for total immunoglobulin E (to exclude an allergic nature or allergic background), feces for worm eggs and scraping for enterobiasis ( adenoids often enlarge due to helminthic lesions), a PCR test for the Epstein bar virus is possible (if mononucleosis is suspected)
Diagnosis of inflammation of the adenoids
If primary symptoms of inflammation of the adenoids appear, it is recommended to consult an ENT doctor. The specialist will conduct an initial consultation and prescribe a comprehensive examination:
- Endoscopy. A small flexible tube with a camera and a light at the end is inserted into the nose or throat. The condition of the nasal passages and adenoids is visualized on a video screen in real time.
- X-ray of the nasopharynx. It is prescribed only if there is a serious justification, when the consequences of the disease cause great harm to health. For adenoids, an X-ray with contrast is performed.
- Computed tomography (CT). Provides detailed images of the sinuses and adenoids.
- Magnetic resonance imaging (MRI). Features highly detailed images of the nasal passages, sinuses and adenoids.
- Laboratory diagnostics. Often includes an immunoglobulin E test, a general blood and urine test. Also, according to indications, bacterial culture from the nasopharynx is performed to test sensitivity to antibiotics, PCR and ELISA diagnostics to determine infections.
If necessary, the patient is referred to an otolaryngologist who performs a digital examination, epipharyngoscopy and posterior rhinoscopy to determine the consistency, size and degree of adenoid vegetation.
Consultation with a pediatric allergist-immunologist and neurologist (in the presence of epileptiform seizures) is required.
Traditional diagnostic methods (examination by an ENT doctor or pediatrician)
In a regular clinic, to diagnose chronic adenoiditis and adenoid hypertrophy, an examination of the nose, throat and ears is used using metal instruments for examining ENT organs: nasal and ear mirrors and a spatula illuminated with reflected light, using a conventional head reflector (head mirror) or a head lamp in the form flashlight. In this case, the ENT doctor (or pediatrician) only sees the area of the nasal vestibule and the surrounding parts of the nose. The nasopharynx, the anatomical location of the adenoids, is not visible. The examination is contact (when examining the nose, the wings of the nose in the vestibule area are expanded with a nasal speculum; when examining the ear, an ear speculum is inserted into the ear canal)
In addition, it will be possible to perform a digital examination of the nasopharynx for a subjective assessment of the size of the adenoids (the doctor feels the nasopharynx and the surface of the adenoids through the mouth, trying to determine their size). This method is not reliable, is unpleasant for a small patient and is traumatic for adenoid vegetations.
Treatment of inflammation of the adenoids in children
Hypertrophied adenoids begin to disappear only from the age of seven. Many children experience complications between the ages of 2 and 3 years. This means another four years of recurring infections and respiratory distress, which is accompanied by poor sleep and changes in facial anatomy.
The only treatment for large adenoids is a surgery called an adenoidectomy. Since adenoids spontaneously shrink over time, indications for surgery should be considered by a medical council. Experts weigh surgical risks against complications caused by airway obstruction.
Adenoidectomy surgery is usually indicated for children with severe airway obstruction aged 3-4 years who have the following symptoms:
- sleep disturbance caused by difficulty in nasal breathing;
- repeated episodes of otitis media with hearing loss;
- chronic sinusitis.
Milder cases are treated with antibiotics and corticoids during crises (adenoiditis). The use of antibacterial drugs is aimed at killing bacteria that cause ear or sinus infections.
Doctors recommend removing adenoids when drug therapy does not give the desired result or complications arise. Surgical intervention involves an adenoidectomy. Sometimes the tonsils and adenoids are removed at the same time. This means that the child undergoes a tonsillectomy and adenoidectomy.
The operation is performed under general anesthesia and does not require long hospitalization after the procedure. Rehabilitation is usually carried out at home under clinical supervision. Most children can return to normal life in less than a week.
What factors contribute to the appearance of adenoids?
Heredity - at least if the parents suffered from adenoids, the child, to one degree or another, will also encounter this problem.
Inflammatory diseases of the nose, throat, pharynx - and respiratory viral infections, and measles, and whooping cough, and scarlet fever, and tonsillitis, etc.
Eating disorders - especially overfeeding and excess sweets.
Tendency to allergic reactions, congenital and acquired immunity deficiency.
Violations of the optimal properties of the air that the child breathes - very warm, very dry, a lot of dust, an admixture of harmful substances (ecological conditions, excess household chemicals).
Thus, the actions of parents aimed at preventing adenoids come down to correction, and even better, to the initial organization of a lifestyle that promotes the normal functioning of the immune system - feeding according to appetite, physical activity, hardening, limiting contact with dust and household chemicals, optimizing physical activity. properties of the inhaled air.
But if there are adenoids, it is necessary to treat them - the consequences are too dangerous and unpredictable if you do not intervene. At the same time, the main thing is lifestyle correction and only then therapeutic measures.
Prevention of adenoiditis
Measures to prevent adenoid hypertrophy include:
- carrying out preventive vaccination;
- daily hardening procedures;
- early diagnosis and rational treatment of infectious diseases of the upper respiratory tract.
Doctors recommend that parents take measures to improve the immunological properties of the body. It is important to follow a daily routine, organize a healthy diet and carry out wet cleaning in the children's room.
Advantages of treating adenoiditis at the RebenOK clinic
Treatment of adenoids in children is carried out in our medical center at affordable prices in Moscow. The clinic is equipped with expert-class diagnostic equipment. We employ competent specialists who have extensive practical experience in the medical and surgical treatment of adenoiditis.
We offer you to use the service of calling a doctor at home. If you have symptoms of adenoid hypertrophy, it is recommended to request a visit to a pediatrician or ENT specialist. A specialist will come to the address specified in the application, conduct an examination and prescribe medications for the treatment of adenoids in children without surgery. If necessary, the patient will be invited to the clinic for a full diagnosis and radical therapy.