1.General information
Potassium is one of the key macroelements in the human body. This substance, especially in interaction with sodium, is necessary for the regulation of contractile activity of muscles (including the myocardium), water-salt, acid-base and energy balance, higher nervous activity, normal fermentation and metabolism, secretory activity of the endocrine glands, functioning liver and kidneys. Up to half of all salts in the body are potassium compounds, and most of them are contained in intracellular liquid spaces.
For all micro- and macroelements, including potassium, a certain concentration range must be observed.
Otherwise, both deficiency and excess lead to the development of severe, sometimes life-threatening conditions. Hyperkalemia, i.e. Excessive potassium levels are a typical example.
A must read! Help with treatment and hospitalization!
Renal mechanism of hyperkalemia
The excretory capacity of the kidneys directly depends on:
- the number of working nephrons - the smallest structural elements, including tubules and glomeruli;
- sufficient sodium and water in the incoming blood;
- concentrations of the adrenal hormone aldosterone.
These components determine the required glomerular filtration rate.
Potassium accumulation begins when the rate decreases to 10-15 ml per minute (normally from 80 to 120) or urine output drops per day to less than a liter
Similar conditions occur in kidney failure caused by inflammatory and other diseases.
There is also a mechanism for blocking potassium release through the connection between renin and aldosterone. The fact is that aldosterone synthesis is activated by the hormone renin. A decrease in its amount automatically leads to hypoaldosteronism (Addison's disease). Similar conditions are caused by drugs (Indomethacin, Captopril), especially in older people and patients with diabetes.
The “renin” variant of kidney pathology is also characteristic of chronic nephritis, mechanical damage, diabetes mellitus, and sickle cell anemia.
Other drugs that affect the excretion of potassium by the kidneys include:
- group of ACE inhibitors,
- Spironolactone,
- Amiloride,
- Triamterene,
- Heparin.
Defective tubular filtration in acute renal failure is associated with direct damage (necrosis) and leads to rapid hyperkalemia.
Mineralocorticoid deficiency (hypoaldosteronism) may be primary due to damage to the adrenal glands or the result of a hereditary disorder of hormone synthesis (with adrenogenital syndrome, congenital deficiency of the hydrolase enzyme).
2. Reasons
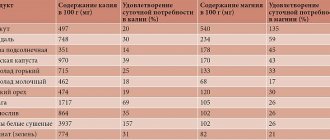
It would be logical to assume that hyperkalemia is caused by excessive consumption of potassium-rich foods, for example, dried fruits, legumes, potatoes, bananas, etc. However, in reality this is extremely rare: the body’s daily need for potassium is quite large (up to 5 g in adults), and with normal metabolism the balance is easily restored through the excretion of potassium in the urine.
Thus, one of the main factors in the development of hypercalcemia is disorders of the kidneys (chronic renal failure, diabetic nephropathy, etc.), when potassium excretion becomes difficult and it begins to be retained in the body. This can be caused, in particular, by hypocorticism (Addison's disease) - chronic functional insufficiency of the adrenal cortex, in which the kidneys simply do not receive the appropriate hormonal “commands”.
Another group of reasons is associated with long-term use of medications that contain potassium or prevent its excretion.
The massive release of potassium from cellular fluids into the bloodstream is accompanied by severe polytrauma with crushing of large volumes of muscle tissue, drug overdose, and extensive burns.
The progressive accumulation of potassium in the body can also be caused by pathologically rapid and intense hemolysis (decomposition of red blood cells) in anemia and some other diseases.
Rarely, hereditary hyperkalemia is recorded - familial hyperkalemic periodic paralysis.
Visit our Therapy page
Potassium is largely an intracellular cation, and its concentration inside and outside the cell is regulated by various mechanisms. When they are violated, hyperkalemia or hypokalemia develops. Hyperkalemia is a condition in which the concentration of potassium in the extracellular fluid is more than 5 mmol/kg. According to research, the total potassium content in the body is about 50 mmol/l, of which 98% is found inside cells. On average, the intracellular potassium concentration is 150 mmol/L, and the extracellular concentration is about 4 mmol/L. Maintaining the ratio of potassium concentrations inside and outside the cell depends on several factors: potassium intake from food and drink, its redistribution between intra- and extracellular compartments and renal excretion.
Potassium homeostasis
About 90% of enteral potassium is excreted by the kidneys and partially eliminated in the stool. However, renal excretion is slow, and in the initial stages the body requires extrarenal mechanisms to maintain potassium concentrations.
Renal potassium excretion
The rate of excretion by the kidneys depends on a number of factors: sodium concentration in the tubules, the renin-angiotensin-aldosterone system, vasopressin, the amount of potassium ingested and its plasma concentration, acid-base status and diuresis rate. Potassium secretion occurs passively in the distal nephron loop and depends on a transmembrane concentration gradient generated primarily by sodium reabsorption.
Aldosterone plays a major role in potassium homeostasis via renal mechanisms. As a result of its action on the connecting segments of the main cells of the cortical and medullary collecting ducts and collecting duct, it increases potassium secretion. If we consider the mechanism of its action at the cellular level, aldosterone opens apical sodium channels and increases Na+/K+-ATPase activity on the basolateral membrane.
The main stimulus for the release of aldosterone is angiotensin II: an increase in its plasma concentration by as little as 0.1 mmol/l causes a significant increase in the synthesis of aldosterone in the zona glomerulosa of the adrenal glands. Aldosterone is also involved in extrarenal regulatory mechanisms, increasing potassium secretion in the intestines and salivary glands. Normally, the intestine accounts for about 5% of potassium excretion, but in renal failure, intestinal excretion increases to 30–50%.
- An increase in plasma potassium concentration is an aldosterone-independent stimulator of Na+/K+- ATPase in the distal segments of the tubules, which, as we remember, helps to increase potassium secretion by the kidneys;
- Increasing the rate of diuresis and Na delivery increases the rate of K secretion;
- In conditions where sodium delivery is impaired (hyponatremia, the effect of drugs: amiloride, triamterene, etc.), the electrochemical gradient causing K secretion decreases.
Extrarenal mechanisms regulating K concentration
Insulin
Physiological insulin levels play an important role in regulating potassium levels. Insulin is a stimulator of Na+/K+-ATPase in liver cells, muscles, and fat cells, which promotes the entry of K+ into the cell. Therefore, in conditions accompanied by a lack of insulin production (diabetes), hyperkalemia often develops.
Catecholamines
Catecholamines, especially beta-2 agonists, stimulate the Na+/K+ ATPase of cells and lead to the movement of K+ into the cell. Administration of epinephrine, albuterol, or salbutamol reduces blood potassium levels, but isoproterenol and beta-1 agonists have no effect on potassium levels. Alpha adrenergic agonists, such as phenylephrine, interfere with the entry of potassium into the cell, thereby increasing its plasma concentration.
Acid-base state
With a decrease in pH by 0.1 U, the concentration of potassium in plasma increases by 0.6 mmol/l (ranging from 0.3 to 1.3 mmol/l), and, accordingly, decreases with increasing pH. However, it has been observed that respiratory acidosis causes less change in potassium concentration than metabolic acidosis.
Pseudohyperkalemia
Pseudohyperkalemia is a phenomenon of increased potassium concentration in vitro with normal values in vivo. Pseudohyperkalemia can be considered when the difference in potassium concentration between the analyzed sample and the patient's plasma is more than 0.5 mmol/L. This condition can be caused by many reasons: thrombocytosis more than 750,000 per mm3, leukocytosis with a cell count more than 50,000 per mm3, hereditary spherocytosis, hemolysis in the blood sample, late separation of plasma and red blood cells, use of inappropriate anticoagulants for the blood sample, incorrect venipuncture, as well as clenching a fist during puncture. According to studies, the use of a tourniquet for venipuncture does not play any role in the development of pseudohyperkalemia.
Causes of hyperkalemia
I. Increased intake of potassium into the body:
Exogenous:
- Foods containing a significant amount of potassium (for example, bananas, etc.);
- Potassium chloride salts;
- Potassium, which is part of penicillin G;
- Collins preservative solution;
- Blood transfusion (increasing the amount of potassium during long-term blood storage);
- Geophagy;
- Medicinal plants: alfalfa, dandelion, nettle, spurge, etc.
Endogenous:
- Increased hemolysis;
- Increased physical activity;
- Gastrointestinal bleeding;
- Increased catabolism;
- Rhabdomyolysis;
- Tumor disintegration.
II. Decreased renal potassium excretion:
1. Chronic kidney disease;
2. Acute renal failure;
3. Disturbance of distal tubular secretion (primary and secondary):
- Primary disorder of tubular secretion;
- Systemic lupus erythematosus;
- Sickle cell anemia;
- Obstructive uropathy;
- Consequences of kidney transplantation;
- Kidney amyloidosis;
- Tubulointestinal nephritis;
- Papillary necrosis.
4. Disorders of the renin-angiotensin-aldosterone system:
- Medicines: ACE inhibitors and AT receptor blockers, NSAIDs, calcineurin inhibitors (tacrolimus, cyclosporine), heparin, lithium preparations, aldosterone antagonists (spironolactone);
- Primary hypoaldosteronism;
- Chronic adrenal hyperplasia;
- Primary hyporenism;
- Hyporenic hypoaldelateralism (type IV renal tubular acidosis);
- Adrenal insufficiency: - Primary (Addison's disease); — Destruction of the adrenal glands as a result of the development of infectious diseases (HIV, CMV, Mycobacterium tuberculosis, Mycobacterium avium); - Blockade of sodium channels of main cells caused by taking various drugs such as triamterene, amiloride, trimethoprim, pentamidine, etc.; - Gordon's syndrome.
5. Impaired sodium transport in the distal canals:
- Chronic heart failure;
- Cirrhosis of the liver;
- Salt wasting nephropathy;
- Kidney failure.
III. Movement of potassium between cells:
1. Hyperglycemia;
2. Use of certain medications:
- Non-selective beta blockers;
- Succinylcholine;
- Mannitol;
- Digoxin (Na+/K+-ATPase inhibitor);
- Somatostatin;
- Intravenous administration of amino acids (arginine, lysine, epsilon-aminocaproic acid);
3. Acute metabolic acidosis caused by mineral acids;
4. Action of herbs (Na+/K+-ATPase inhibitors): oleander, foxglove, yew berries, kendar, Siberian ginseng, etc.;
5. Excessive physical activity;
6. Acute hemolysis;
7. Fluoride poisoning;
8. Hyperkalemic periodic paralysis;
Clinical manifestations
As mentioned earlier, the toxic effect of hyperkalemia is manifested in the depolarization of the membranes of cardiac and skeletal muscle cells.
Cardiac manifestations of hyperkalemia include: peaked T-waves, prolongation of the PR interval, widening of the QRS complex along with the disappearance of atrial electrical activity, ventricular fibrillation (VF), and asystole. VF and asystole may be the initial manifestations of hyperkalemia, however, even with potassium levels above 9 mmol/l, ECG manifestations may be absent.
From the neuromuscular system, hyperkalemia is manifested by diarrhea, abdominal pain, myalgia and flaccid paralysis. Factors that aggravate the manifestations of hyperkalemia are concomitant metabolic disorders, such as metabolic acidosis, hypocalcemia or hyponatremia.
Mortality from hyperkalemia in hospitalized patients ranges from 1.7 to 41%. Cardiac causes make the greatest contribution to these figures. Mortality studies for hyperkalemia have found that treatment is often inadequate or not treated at all.
Treatment
Hyperkalemia is a life-threatening condition and must be treated promptly. Potassium levels ≥ 6 mmol/L are considered to require more aggressive therapy. When the upper limit of normal is less than that, the goal of treatment is to remove excess potassium from the body and prevent recurrent episodes of hyperkalemia by finding the causes and eliminating them.
As soon as an increase in potassium levels is registered in the patient, then, depending on the severity of the condition, an examination is carried out using the ABCDE algorithm, and electrocardiographic monitoring in 12 leads is also established. During ECG monitoring, possible manifestations of conduction and excitability disorders are identified: pointed T-waves, flat P waves or their absence, sinusoidal waves, prolongation of the PR interval, expansion of the QRS complex, ventricular tachycardia.
If abnormalities are detected on the ECG, calcium supplementation is prescribed. Calcium is a direct antagonist of potassium-induced intracellular depolarization and, when administered, is capable of normalizing the membrane potential.
Recommended doses of calcium: calcium gluconate 10% - 30 ml or calcium chloride 10% - 10 ml. The drugs are administered intravenously as a bolus over 5–10 minutes; good intravenous access is required for this. The effect of calcium supplements develops within a few minutes, but does not last long (30–60 minutes); if necessary, a second dose can be administered after 5 minutes. However, it is worth remembering the danger of developing life-threatening arrhythmias when using these drugs in patients with concomitant digoxin intoxication: therefore, during the administration of calcium, it is necessary to monitor the patient even more carefully.
The next step in the treatment of hyperkalemia is the administration of insulin. As stated earlier, insulin has a strong hypokalemic effect, regardless of blood glucose levels. There are many insulin administration regimens for hyperkalemia: the most common is the intravenous administration of 10 units of fast-acting insulin against the background of an infusion of 25–50 grams of glucose, followed by monitoring blood glucose levels. In the presence of significant hyperglycemia (more than 250 mg/dL or 13.9 mmol/L), insulin administration without concomitant administration of glucose is acceptable. This administration regimen allows reducing potassium levels by more than 0.5 mmol/L in all patients. The hypokalemic effect of the glucose-insulin mixture develops after 10 minutes, and the maximum effect (decrease in potassium concentration from 0.65 to 1 mmol/l) is achieved by 30 minutes and lasts from 4 to 6 hours.
The next option is the use of catecholamines. Catecholamines activate the Na+/K+-ATPase of cells and promote the transition of potassium into the cell. For these purposes, it is advisable to use beta-2 agonists (adrenaline, albuterol, terbutaline, salbutamol, salmeterol) intravenously or through a nebulizer or metered dose inhaler. These drugs can reduce potassium levels from 0.5 to 1.5 mmol/l. The onset of the hypokalemic effect occurs after 3–5 minutes, reaching a maximum by 30 minutes when administered intravenously and by 60 minutes when using a nebulizer; the total duration of action is from 3 to 6 hours. For inhalation via a nebulizer, it is preferable to use albuterol 10–20 mg or salbutamol 10–20 mg. Side effects of beta-2 agonists include tremor and tachycardia, as well as, if hypoglycemia develops, masking of its symptoms. The use of bicarbonate for hyperkalemia has not been shown to be effective and, given the risk of hypernatremia and fluid overload, is not recommended as initial or monotherapy.
Removing potassium from the body
Diuretics
Loop or thiazide diuretics may play an important role in the treatment of chronic hyperkalemia. However, their use in acute hyperkalemia is limited due to significant losses of sodium when the required potassium level is achieved, as well as disturbances in water balance. Patients also often have renal failure, which limits the use of diuretics.
Ion exchange resins
Sodium polystyrene sulfonate (Keoxalate) is an ion exchange resin that exchanges potassium cations for sodium. Also widely used is the calcium drug resonium, which binds and removes excess potassium. During prolonged contact (for at least 30 minutes) in the intestine with potassium-secreting cells, each gram of the drug binds from 0.65 to 1 mmol of potassium, which is then excreted in the feces. These drugs can be used either per rectum using an enema or orally in the form of tablets.
The main limitation of the use of resins is the development of osmotic diarrhea after 2 hours with a maximum after 4–6 hours, as well as the likelihood of developing intestinal necrosis. The use of resins is contraindicated in patients with intestinal obstruction or intestinal ischemia and in the early postoperative period after kidney transplantation. Ion exchange resins can be used as monotherapy for chronic hyperkalemia or mild acute hyperkalemia with potassium levels less than 6 mmol/l with evaluation of treatment effectiveness.
Dialysis
Removing potassium from the body by hemodialysis or other renal replacement therapy (RRT) is the most effective method currently available. Different dialysis modes differ in the speed at which the effect develops. Conventional hemodialysis reduces potassium levels much more quickly than peritoneal dialysis or continuous regimens (continuous venovenous hemofiltration, continuous venovenous hemodialysis, or continuous venovenous hemodiafiltration).
Studies have shown that with hemodialysis, the rate of potassium reduction can reach 25–50 mmol/hour, with a significant decrease in plasma potassium levels (about 1.3 mmol/L) during the first hour of therapy. During conventional hemodialysis, which usually involves simultaneous ultrafiltration and dialysis, potassium removal by ultrafiltration accounts for about 15% of the total potassium removed, and by dialysis the remaining 85%. The amount of potassium removed depends on the potassium content of the dialysate and its gradient with plasma, the duration of the dialysis session, the size and permeability of the filter membrane, and the volume of ultrafiltration.
After taking urgent measures to reduce potassium levels, it is necessary to analyze the patient’s medical history, diet, medications taken (stop taking medications that increase potassium levels), and eliminate the causes that can lead to recurrent hyperkalemia. Subsequently, until the potassium level stabilizes in these patients, it is recommended to monitor it every 2 hours and, if necessary, repeat the measures according to the algorithm.
3. Symptoms and diagnosis
The clinical picture of hyperkalemia is not specific enough, so preliminary, presumptive diagnosis requires a doctor to have a lot of experience, attention and vigilance in this regard. Most often, changes in the ECG in combination with patient complaints of tachycardia (accelerated heartbeat), general malaise and constant weakness cause alarm. In more severe cases, cardiac abnormalities caused by excess potassium may take the form of arrhythmia, asystole, ventricular fibrillation, and ultimately cardiac arrest.
The diagnosis is established by comparing the existing clinical manifestations, the electrocardiographic picture and the results of laboratory tests (determining the concentration of potassium in the blood plasma). Depending on the most likely causes, an additional specialized examination is prescribed - for example, nephrological or endocrinological.
About our clinic Chistye Prudy metro station Medintercom page!
What symptoms indicate an increase in potassium in the blood?
Symptoms of hyperkalemia are caused by impaired transmission of nerve impulses to muscle tissue and changes in the properties of the myocardium (excitability and contractility).
Weakness increases to the point of paralysis
A patient with other chronic diseases complains of:
- muscle weakness;
- a feeling of heart failure in the chest, periodically a feeling of fading and stopping;
- nausea, lack of appetite.
Prolonged hyperkalemia leads a person to exhaustion.
In children, symptoms of hyperkalemia include:
- low mobility;
- flaccid paralysis in the muscles;
- bradycardia;
- decrease in blood pressure.
4.Treatment
With moderate and severe severity, hyperkalemia requires emergency intensive care due to the threat of cardiac arrest. One of the emergency measures is the intravenous administration of a special solution (calcium, insulin, glucose), but its effect is short-lived, and after relief of life-threatening symptoms, further therapy is required. Potassium-absorbing sorbents are prescribed (which ensures its excretion in feces); diuretics are used if renal function is preserved. Stop taking any medications that in one way or another affect the circulation of potassium in the body. Limit potassium intake from food. Since hyperkalemia is almost always secondary, a diagnostic examination (if the cause of the detected hyperkalemia is unknown) and treatment of the underlying disease are mandatory.
Classification
Most often in clinical practice, hypokalemia is divided into:
- light
- K+ content 3-3.5 meq/l. - severe
- K+ level below 3 mmol/l.
Separately, pseudohypokalemia is distinguished, which has no symptoms and does not require treatment. A false test result can be obtained if the patient has a very high level of leukocytes (leukocytes actively absorb K+). This happens, for example, with leukemia or severe infection. Falsely elevated readings are also possible if the K+ concentration is determined in blood stored for a long time at room temperature.
Popular questions about hypokalemia
What is hypokalemia?
This is a condition characterized by a decrease in plasma potassium concentration below 3.5 mmol/l.
What does low potassium in the blood mean?
The reason may be different - from insufficient intake of macronutrients from food to dysfunction of the adrenal cortex. To install it, you need to conduct a detailed examination.
How to determine the lack of potassium in the body?
There are no specific symptoms of deficiency of this element. Hypokalemia can be suspected by increasing muscle weakness, increased fatigue, and heart rhythm disturbances. Potassium deficiency can be confirmed by laboratory tests.
Symptoms of hypokalemia
In some patients, hypokalemia may occur without any symptoms. The clinical picture and its severity are determined to a greater extent not by the K+ concentration, but by the rate of its decrease. Muscle weakness is one of the first symptoms. Sometimes muscle twitching (fasciculations) and tetanic convulsions (spasms) occur. Inhibition of the excitability of CNS neurons leads to the development of symptoms of psychasthenia (drowsiness, apathy, poor concentration).
Due to the slow motility of the gastrointestinal tract during meals, a feeling of satiety sets in very quickly, and heaviness in the epigastrium is disturbing. Constipation is typical. The conduction system of the heart is especially sensitive to a decrease in K+ - tachycardia and interruptions in heart function appear. Due to hypotension, dizziness begins. With primary hyperaldosteronism, on the contrary, symptoms of arterial hypertension are always observed (heaviness and pain in the back of the head, tinnitus). Patients are also concerned about increased diuresis and a constant feeling of thirst.