Erythremia is a tumor clonal disease of the hematopoietic system, in which there is proliferation of erythroid, granulocytic and megakaryocytic lineages of hematopoiesis with predominant activation of erythropoiesis. At the same time, an increase in the level of red blood cells and hemoglobin, thrombocytosis and leukocytosis is noted in the blood. Almost all patients with erythremia are carriers of the JAK2V617F mutation.
- How does erythremia develop?
- Symptoms of erythremia
- Stages of erythremia
- Diagnosis of erythremia
- Treatment of erythremia
- Prognosis for erythremia
How does erythremia develop?
The causes of erythremia are still unknown. It is believed that this is a multi-stage disease in which, under the influence of external factors, the genome of a normal cell is damaged, which leads to its malignant transformation and the formation of a tumor cell clone that replaces normal hematopoiesis.
Almost all patients have a mutation in the JAK2 gene. Exon 14 is usually affected; 90-96% of patients have the V617F mutation. 2% of patients have mutations in exon 12. Damage to other genes, in particular MPL, CALR, is very rarely detected. All of these genetic pathologies are specific to erythremia, so their determination is necessary to confirm the diagnosis.
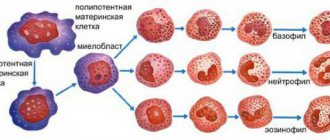
So, molecular genetic disorders cause activation of the JAK-STAT signaling pathway, which leads to increased proliferation of hematopoietic sprouts and an increase in the number of blood cells.
Monocytes and megakaryocytes (platelet precursors) produce a variety of cytokines - biologically active molecules that stimulate fibrotic changes, the formation of new blood vessels, which ultimately leads to osteosclerosis and bone marrow fibrosis. In addition, massive production of cytokines contributes to the development of tumor intoxication, which aggravates the general condition of patients.
There is also a disruption in the connection of stem cells with the microenvironment. This provokes the formation of foci of hematopoiesis outside the bone marrow. The liver and spleen are primarily affected.
Polycythemia is a chronic disease in which the bone marrow produces an excess amount of red blood cells. In many patients, the number of platelets and white blood cells in the blood also increases. As a result, the blood becomes thicker and more viscous, blood flow in small vessels is disrupted, and the likelihood of thrombus formation—blood clots that clog the lumen of blood vessels and disrupt the blood supply to organs—increases.
Polycythemia vera is quite rare and develops slowly. Most often it occurs in people over 40-50 years of age, but isolated cases have been observed in younger people and even children. In the initial stages, it is asymptomatic, so it is often diagnosed accidentally during an examination related to another disease.
If left untreated, polycythemia can be life-threatening. However, modern approaches to therapy can achieve very good results: patients get rid of most of the negative manifestations of the disease.
Synonyms Russian
Polycythemia vera, polycythemia vera, primary polycythemia, erythremia, Vaquez disease, Osler-Vaquez disease.
English synonyms
Erythremia, Osler-Vaquez Disease, primarypolycythemia, splenomegalicpolycythemia, polycythemiarubravera, erythrocytosismegalosplenica, cryptogenicpolycythemia.
Symptoms
- Weakness.
- Dyspnea.
- Headache.
- Frequent bleeding.
- Heaviness in the stomach.
- Pain in muscles and joints.
- Redness of the skin.
- Itching, especially after taking a warm shower or bath.
General information about the disease
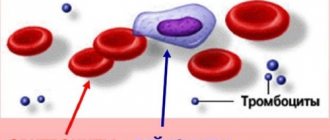
All blood cells are formed in the bone marrow from a single blood stem cell. It gives rise to a lymphoid stem cell and a myeloid stem cell. Lymphocytes are formed from the lymphoid stem cell, and other types of leukocytes, platelets and erythrocytes are formed from the myeloid stem cell. Mature red blood cells are biconcave cells that do not have a nucleus. The main function of red blood cells is to transport oxygen from the lungs to tissues and carbon dioxide from tissues to the lungs. This function is carried out by hemoglobin, which occupies most of the red blood cell and gives this cell its characteristic red color. In addition to the respiratory function, red blood cells are involved in maintaining acid-base balance, and also transport amino acids, fats, proteins and toxins on their surface. Red blood cells exist for 120 days and are then destroyed in the liver and spleen.
Erythropoiesis (formation of red blood cells) is a complex multi-stage process, the main regulator of which is the protein erythropoietin. It is produced in the kidneys and partly in the liver, and its amount increases when the level of oxygen in the blood decreases (hypoxia). Normally, during hypoxia, the amount of erythropoietin increases, which activates the formation of red blood cells in the bone marrow. However, with polycythemia vera, the level of erythropoietin not only does not increase, but may even be reduced. Increased formation of red blood cells is associated with increased sensitivity of bone marrow cells to erythropoietin. The reasons for such changes have not been fully elucidated, but it is known that in polycythemia vera there are disturbances in the Janus kinase 2 gene and the EpoR gene, which carry information about the number of erythropoietin receptors and their sensitivity.
Thus, with polycythemia, an excess amount of red blood cells is formed, the blood volume increases, and it becomes thicker. Blood flow in small vessels is disrupted. As a result, blood pressure increases and frequent bleeding occurs, in particular bleeding gums. Due to impaired blood circulation, the tips of the fingers, nose, and mucous membranes acquire a bluish-red tint. The oxygen supply to tissues deteriorates, which negatively affects the functioning of the entire body. A change in blood viscosity increases the likelihood of thrombosis - blockage of blood vessels with blood clots, which leads to disruption of the functioning of organs and tissues. This can manifest itself as a heart attack or stroke. The liver and spleen enlarge, and foci of hematopoiesis appear in them.
Along with true, primary polycythemia, the cause of which is unknown, secondary polycythemia is isolated, in which an increase in the production of red blood cells is caused by increased levels of erythropoietin in response to a lack of oxygen in the tissues, for example, with chronic bronchitis or heart disease. In this case, polycythemia is only a consequence and disappears when the underlying disease is treated.
Who is at risk?
- Men.
- People over 40 years old.
- Representatives of the Caucasian race.
- Patients whose relatives had polycythemia.
Diagnostics
Laboratory diagnostics
- Complete blood count (without leukocyte formula and ESR)
- Red blood cells. Their levels are usually significantly elevated.
- Leukocytes. Their concentration can be increased mainly due to neutrophils.
- Platelets. Platelet levels may also be elevated.
- Hemoglobin is a protein that is part of red blood cells and is involved in the transport of oxygen. In polycythemia it is usually elevated.
- Hematocrit This is the ratio of red blood cell volume to total blood volume. In polycythemia it is usually elevated.
- Reticulocytes are immature red blood cells. They enter the blood from the bone marrow and mature within 2-3 days, turning into mature red blood cells. With polycythemia, their excess may be observed, which indicates their accelerated formation in the bone marrow.
- Erythropoietin. With polycythemia vera it is usually very low.
- Vitamin B12. Plays an important role in the synthesis of nucleic acids (compounds involved in the storage and transmission of hereditary information) necessary for the formation of red blood cells. An increase in its level in polycythemia indicates the intensity of red blood cell formation.
- The main blood electrolytes are sodium, potassium, calcium,
Symptoms of erythremia
Clinically, erythremia manifests itself in two syndromes:
- Plethora (plethora). This syndrome is characterized by an increase in the number of circulating red blood cells. Symptomatically manifested by headaches, dizziness, attacks of rapid heartbeat, itchy skin and visual disturbances. The skin and mucous membranes have a bluish tint. Vascular complications are also possible: thrombosis, erythromelalgia (redness of the fingers, pain and burning sensation in them).
- Myeloproliferative syndrome - develops as a result of hyperplasia of hematopoietic germs. Symptomatically manifested by weakness, fever, sweating, itchy skin, bone pain. With the breakdown of granulocytes, a disturbance in urate metabolism is observed, which leads to the development of gout, kidney stones and urate diathesis.
Publications in the media
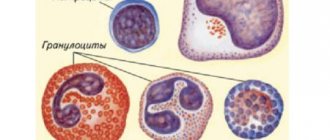
Polycythemia vera (polycythemia vera) is a neoplastic disease accompanied by an increase in the number of red blood cells, white blood cells and platelets. The source of tumor growth is the precursor cell of myelopoiesis. Frequency. 0.6 cases per 10,000 population. The predominant age is elderly. Genetic aspects • Polycythemia vera (*263300, ) • Hereditary isolated erythrocytosis (*133100, 133110, ) • Polycythemia with increased ATP content (*102900, ) - increased pyruvate kinase activity with a decreased content of 2,3-diphosphoglycerate. Pathogenesis • Increased proliferation of all three lineages of hematopoiesis (with a predominance of erythrocyte) leads to an increase in Ht, a decrease in blood flow in tissues and a decrease in their oxygenation, an increase in cardiac output • The appearance of foci of extramedullary hematopoiesis in the liver and spleen.
Clinical picture • Plethoric syndrome •• Headache •• Dizziness •• Visual impairment •• Angina pain •• Skin itching •• Paresthesia •• Arterial hypertension •• Tendency to thrombosis (less commonly, hemorrhagic syndrome) • Myeloproliferative syndrome •• General weakness • • Increased body temperature •• Bone pain •• Feeling of heaviness in the left hypochondrium •• Splenomegaly (less commonly, hepatomegaly) as a result of the appearance of foci of extramedullary hematopoiesis and venous stagnation. Laboratory research . Trephine biopsy of the bone marrow (three-line hyperplasia of the bone marrow with a predominance of erythropoiesis, absence of iron deposits). Differential diagnosis . Other polycythemias • Primary •• Erythrocytosis familial type •• Erythrocytosis of the Volga region (endemic foci) • Secondary •• Physiological erythrocytosis due to poor tissue oxygenation ••• Low pO2 (for example, in high mountains) ••• COPD accompanied by hypoventilation ••• Cardiac shunt from right to left ••• Hemoglobinopathies with high oxygen affinity ••• Carboxyhemoglobin in “smokers' polycythemia” ••• Deficiency of erythrocyte 2,3-diphosphoglycerate ••• Hereditary increase in ATP content in erythrocytes ••• Insufficiency of 2,3-diphosphoglycerate mutase • • Increased erythropoietin levels ••• Kidney disease ••• Hypernephroma or renal carcinoma ••• Renal cyst and hydronephrosis ••• Bartter's syndrome ••• Kidney transplantation ••• Erythropoietin-producing tumors ••• Hypersecretion of the adrenal cortex ••• Exogenous androgens •• Relative erythrocytosis (pseudopolycythemia, false polycythemia) - increased Ht due to decreased plasma volume (excessive diuresis, nasogastric drainage, severe gastroenteritis, especially in young children, burns). The erythrocyte mass remains within normal limits. Diagnostic criteria . The diagnosis confirms the presence of three main criteria or a combination of the first two main criteria and any of two additional criteria • Main criteria •• Increased erythrocyte mass •• Arterial blood oxygen saturation above 92% •• Splenomegaly • Additional criteria - leukocytosis, thrombocytosis, increased alkaline phosphatase activity of leukocytes and an increase in the concentration of vitamin B12 in the blood serum • Other criteria •• Hyperuricemia •• Hypercholesterolemia •• Increased concentration of histamine in the blood •• Reduced concentration of erythropoietin in the blood.
TREATMENT. Removal of red blood cells from the bloodstream or suppression of erythropoiesis, a combination of both methods is possible • Bloodletting as a method of eliminating red blood cells is the safest type of therapy, carried out until the Ht level decreases below 50%. Inhibition of the hematopoietic function of the bone marrow is necessary when it is impossible to correct Ht with bloodletting alone or when there is increased activity of other cell lineages • Radioactive phosphorus effectively regulates the activity of the bone marrow and is well tolerated; therapy is especially beneficial for patients in older age groups • Chemotherapy. Chlorambucil is quite effective, but a leukemic effect is possible. Currently, hydroxyurea (and its derivatives) is used for polycythemia vera. Current and prognosis . Survival is 7-10 years, without treatment - 2-3 years. With bloodletting, the main complications are thromboembolic and cardiovascular. After chemotherapy, neoplasia is possible, incl. leukemic transformation of bone marrow. Concomitant pathology • Budd–Chiari syndrome • Thrombosis of mesenteric arteries. Synonyms • Erythremia • Primary polycythemia • Vaquez disease • Osler disease • Vaquez–Osler disease
ICD-10 • D45 Polycythemia vera
Note. The term "polycythemia" means an increase in the number of red blood cells (regardless of the number of white blood cells and platelets). The term “erythrocytosis” is more accurate. Application. Gaisböck syndrome: polycythemia with arterial hypertension, plethora, swollen vessels of the head, neck, arms, enlargement of the left ventricle of the heart; Characterized by excess body weight, possible nosebleeds and stroke.
Stages of erythremia
During its development, erythremia goes through several stages. The first, also known as initial, can last more than 5 years. During this period, moderate manifestations of plethoral syndrome are mainly present. The blood test shows moderate erythrocytosis, and in the bone marrow there is an increase in the proliferation of all hematopoietic lineages with the exception of the lymphocytic lineage. The spleen is not enlarged, complications rarely develop.
The second stage of erythremia is polycythemia. It is divided into 2 substages A and B. Stage A lasts 5-15 years. It is characterized by an increase in the number of formed elements in the blood. As a result, a pronounced plethoric syndrome is formed, which is complicated by thrombosis, bleeding, and an increase in the size of the liver and spleen. In the blood test, cytosis increases; in the bone marrow, in addition to the proliferation of erythropoietic, granulocytic and thrombopoietic lineages, cicatricial changes are noted.
With erythremia in stage B, cytosis and clinical symptoms continue to increase. Foci of tumor growth form in the spleen, and cicatricial changes progress in the bone marrow.
Stage 3 of erythremia - anemic. Here, bone marrow fibrosis already develops, which leads to its depletion and a decrease in the level of blood cells. The disease can transform into acute leukemia.
Erythremia
In stage I, which lasts 5 years or more, there is a moderate increase in circulating blood, the spleen cannot be palpated. In the blood at this stage, moderate formation of red blood cells predominates. In the bone marrow, there is an increase in all hematopoietic germs. Vascular and visceral complications at this time are possible, but not frequent.
The identification of the initial (I) stage of erythremia is conditional. Essentially, this is a stage with few symptoms, more typical for older patients. The spleen is usually not palpable, but examination of it often reveals a slight enlargement. Thrombotic complications are also possible at this stage of the disease.
Stage IIA of the process - erythremic - is extensive, and myeloid transformation of the spleen is uncharacteristic for it. The duration of this stage is 10-15 years or more. The volume of circulating blood is increased, the spleen is enlarged, and a little earlier the liver may become enlarged. Thrombosis of arterial and venous vessels, hemorrhagic complications are observed more often at this stage. A blood test indicates “pure” erythrocythemia or erythrocythemia and thrombocytosis or panmyelosis and neutrophilosis with a band shift, an increase in the number of basophils. In the bone marrow, total three-line hyperplasia with pronounced megakaryocytosis is observed; reticulin and focal collagen myelofibrosis are possible.
Stage IIB also includes an erythremic, extensive process, but with myeloid metaplasia of the spleen. The increase in blood volume can be expressed to a greater or lesser extent, and an enlargement of the liver and spleen is observed. In the blood at this stage there is an increase in red blood cells, platelets with leukocytosis above 15 H 103 in 1 μl and a shift in the leukocyte formula to myelocytes, single erythrokaryocytes. In the bone marrow, as in stage IIA, an increase in granulocytic lineage may predominate, and reticulin and focal collagen myelofibrosis is possible.
Allergic complications and urate diathesis are often the leading ones in the clinical picture.
At this stage, the patient may be exhausted, worsening thrombotic complications and bleeding.
Stage III of erythremia is called anemic. Myelofibrosis may be expressed in the bone marrow; myelopoiesis is preserved in some cases and reduced in others. Myeloid transformation is observed in the enlarged spleen and liver. The outcome of erythremia at this stage can be acute leukemia, chronic myeloid leukemia, hypoplastic state of hematopoiesis, and hematological changes that are difficult to classify.
Arterial hypertension, which occurs with erythremia in 35-50% of cases, is caused by an increase in peripheral resistance in response to increased blood viscosity, the development of urate diathesis, chronic pyelonephritis, circulatory disorders in the renal parenchyma, thrombosis and sclerosis of the renal arteries.
Skin itching associated with washing, specific to erythremia, is observed in 50-55% of patients. For many patients, it becomes the main complaint; it arises not only from contact with water, but also spontaneously, affecting performance.
Frequent complications of the advanced stage of the disease are microcirculatory disorders with clinical manifestations of erythromelalgia, transient disorders of cerebral and coronary circulation and hemorrhagic edema of the legs, as well as thrombosis of venous and arterial vessels and bleeding. Already at this stage there may be hemostasis disorders, which often look like a latent thrombogenic danger, detected only in the laboratory and without clinical manifestations. At the same time, hemostasis disorders can be more pronounced, leading to local intravascular coagulation such as microthrombosis or to disseminated intravascular coagulation - DIC syndrome.
Diagnosis of erythremia
As part of the diagnosis of erythremia, the patient undergoes a comprehensive examination, which includes the following measures:
- Anamnesis and physical examination, during which the color of the skin of the face and extremities is assessed. The size of the liver and spleen must be determined.
- A detailed blood test, including counting the number of blood cells and erythrocyte indices.
- Trephine biopsy of the bone marrow followed by histological and histochemical examination.
- Determination of erythropoietin level.
- Molecular genetic testing for the presence of specific V617F mutations.
- Ultrasound of the liver and spleen to accurately determine their size.
The diagnosis of erythremia is made according to the 2021 WHO criteria, which distinguishes three major criteria and one minor one.
Major criteria for erythremia:
- The hemoglobin level is more than 160 g/l in women and more than 165 g/l in men.
- Hyperplasia of three myelopoiesis lineages in bone marrow trephine.
- The presence of a mutation in the JAK2 gene.
A minor criterion is a decrease in erythropoietin levels.
To make a diagnosis of erythremia, it is necessary either to have all three major criteria, or 1-2 major and one minor.
Treatment of erythremia
The main goals of treatment for erythremia are:
- Preventing the formation of blood clots and treating already developed thrombosis and thromboembolism.
- Reducing the level of tumor intoxication and controlling associated symptoms (fever, itching, weight loss).
- Reducing the risk of transformation into acute myeloid leukemia or myelofibrosis.
- Preventing the development of complications if surgical interventions or pregnancy are necessary.
To assess the likelihood of developing thrombosis during erythremia, risk stratification is carried out according to the following criteria:
- Age over 60 years.
- Presence of thrombosis in the past.
- Cardiovascular risk factors: arterial hypertension, excess weight, diabetes, physical inactivity.
If the patient does not have the listed factors, then he is classified as a low-risk group, in the presence of cardiovascular factors - as an intermediate one, and if he is over 60 years old and/or has a history of thrombosis, he is considered to be at high risk of thromboembolic complications. The platelet level does not affect the risk of thrombosis, but it plays a certain role in the development of bleeding. To prevent the development of thrombosis, it is necessary to eliminate cardiovascular risk factors, as well as prescribe antiplatelet agents.
In addition, the following methods are used to treat erythremia:
- Removing excess red blood cells in the blood. It can be carried out either using hemoexcursion (regular bloodletting) or erythrocytepheresis (removal of red blood cells directly).
- Cytoreductive therapy. Cytostatics and interferons are used.
- Treatment of complications of already developed thrombosis.
Hemoexcursions (bloodletting) for erythremia
Bloodletting is used to reduce the volume of circulating blood. The volume of hemoexcursion is 250-500 ml per procedure, after which the missing volume of fluid is replenished with saline solution. Or the second option is a preliminary infusion of antiplatelet agents together with saline in a volume exceeding the volume of blood removed. Sessions are carried out every other day until the hematocrit reaches 40-45%. For elderly patients, sessions are performed 2 times a week, or the volume of blood excursion is reduced.
Erythrocytopheresis
Erythrocytapheresis refers to methods of extracorporeal detoxification, which replaced bloodletting. It is based on the removal of red blood cells, followed by the return of plasma and replenishment of the volume with solutions of crystalloids or colloids. In one session, up to 400 ml of red blood cells can be removed.
Acetylsalicylic acid preparations
Acetylsalicylic acid, or aspirin, is prescribed to prevent thrombotic complications. Aspirin should be prescribed to every patient with erythremia unless there are contraindications. If they are present, clopidogel or ticlopidine is prescribed.
Cytoreductive therapy
Hydroxyurea
Theoretically, hydroskiurea can be used as part of first-line therapy in patients of any age. But due to the fact that it is genotoxic and can provoke a leukemic effect, such first-line treatment is not recommended for patients under 50 years of age and pregnant women. It is also necessary to discontinue treatment in case of intolerance and ineffectiveness of therapy. The criterion for intolerance to hydroxyurea is the presence of at least one of these symptoms:
- Exceeding the hematocrit by more than 45% 3 months after treatment with hydroxyurea at a dosage of 2000 mg/day.
- Lack of control of myeloproliferation. This may be indicated by a platelet level of more than 400×10 9 and a leukocyte level of more than 10×10 9 after 3 months of treatment.
- Presence of an enlarged spleen (more than 10 cm below the costal margin) or the inability to eliminate the symptoms of splenomegaly.
- Myelopenia when using minimal dosages of drugs - platelet level below 100×10*9 or hemoglobin below 100 mg/l.
- Ulcers on the legs.
- Damage to the skin and mucous membranes.
- Disruption of the gastrointestinal tract.
- Pneumonitis.
- Fever.
Interferon alpha
Interferon alfa is highly effective against erythremia and allows a molecular response to be achieved in some patients. It also relieves plethoral syndrome well, reducing the severity of itching. However, its widespread use is limited by poor tolerability. It is mainly recommended for patients under 50 years of age.
Busulfan
With the help of busulfan, active control of erythremia is possible, however, with long-term use, the risk of developing secondary leukemia increases. Therefore, it is used in patients over 70 years of age with intolerance to hydroxyurea and interferons.
Prognosis for erythremia
In general, the prognosis for erythremia is relatively favorable. The overall 10-year survival rate is about 75%. But the disease can transform into acute myeloid leukemia (5% risk) or myelofibrosis (slightly less than 10% risk).
Symptoms of erythremia (headaches, bone pain, paresthesia) can worsen the quality of life of patients. The main cause of death in patients is thrombosis, bleeding and severe infections, the risk of which increases when the pathology transforms into acute myeloid leukemia or myelofibrosis.
Treatment of erythremia at the Euroonko clinic is carried out using modern treatment protocols. In difficult cases, the decision is made collegiately by a council of specialists. We attach great importance to monitoring the patient during the period of remission. This also makes it possible to achieve an increase in the effectiveness of the treatment.
Book a consultation 24 hours a day
+7+7+78