1.General information
“Algomenorrhea” literally means a disturbed, irregular menstrual cycle in mandatory combination with pain syndrome (“algo-”). Thus, this term differs from the narrower ones: “dysmenorrhea” (cycle irregularity); “algomenorrhea” or “menalgia” (painful menstruation).
However, even without terminological nuances it is obvious: algodismenorrhea is a complaint that is heard in the gynecologist’s office much more often than any other.
Epidemiological estimates, including for Russia, vary widely. The most commonly reported (or repeated from sources from the 1990s) prevalence of algomenorrhea is 40-55% among women aged from menarche to 45 years. However, in a number of publications, the incidence of “painful menstrual syndrome” is estimated much more pessimistically - up to 80% or, conversely, more optimistic - 8-10% (which seems to be clearly underestimated).
Meanwhile, the medical and social significance of the problem is undeniable. Algomenorrhea sharply reduces a woman’s quality of life, limiting her social functioning and negatively affecting her psychological state. When severe, this symptom complex leads to temporary disability. Finally, algodismenorrhea is often the only sign of latent gynecological pathology, which, even being severe and dangerous, does not manifest itself in anything else until a certain moment.
A must read! Help with treatment and hospitalization!
Video reviews of consultations and services of a gynecologist in our clinic
Ekaterina, 35 years old. Clinical examination
Katerina V. - pregnancy management
Irina, 25 years old, Tula
Anastasia, 30 years old - treatment by a gynecologist, pregnancy management
.
Gynecologists at our clinic
Gaponova Natalia Mikhailovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
Main areas of practical activity: treatment of infectious and inflammatory diseases of the pelvic organs, ovarian dysfunction, menstrual irregularities, correction of menopausal disorders, minimally invasive treatment methods in gynecology, intimate surgery. Pregnancy management, female infertility.
Kulik Svetlana Vladimirovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 2000, she graduated from the medical faculty of the Volgograd Medical Academy. Has additional professional retraining in gynecology-endocrinology, operative hysteroscopy, ultrasound diagnostics in obstetrics and gynecology.
Work experience in the specialty is 12 years.
Ivanova Natalya Vladimirovna
Obstetrician-gynecologist, doctor of the highest category, candidate of medical sciences
In 1983 she graduated from Voronezh State Medical Institute named after. N.N. Burdenko. Areas of professional interests: recurrent miscarriage, plastic surgery of the labia minora and majora, vaginal restoration after traumatic childbirth.
32 years of experience in the specialty.
Kavun Irina Sergeevna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 1987 she graduated from the medical faculty of the Yaroslavl State Medical Institute. Doctor of the highest category. Has professional retraining in ultrasound diagnostics in obstetrics and gynecology, surgical obstetrics and gynecology, endoscopy.
Work experience in the specialty is 25 years.
Smirnova Lyudmila Evgenievna
Obstetrician-gynecologist. Candidate of Medical Sciences. Doctor of the highest category.
Engaged in the diagnosis and treatment of diseases of the female reproductive system and pregnancy management. He is engaged in scientific work.
Work experience 16 years.
Buga Marina Vladimirovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 1987 she graduated from the medical faculty of the Kazan State Medical Institute. Has retraining in gynecology-endocrinology, ultrasound diagnostics in obstetrics and gynecology. Specializes in the treatment of diseases of the female reproductive system.
Work experience in the specialty is 25 years.
2. Reasons
Primary and secondary algodismenorrhea are two fundamentally different forms of the syndrome.
Primary, or functional, is characterized by the absence of pathological changes in the genitourinary system that could be objectified by existing diagnostic methods. In other words, it hurts where there seems to be nothing to hurt, since all organs and structures are anatomically correct, intact (not damaged), functionally sound and not affected by any pathological process. Various hypotheses in this regard are currently being put forward and discussed. Thus, one cannot ignore the role of the psychological factor: primary algodysmenorrhea usually affects nulliparous young women or young girls, especially those of asthenic physique, with certain features of psychophysical infantilism, neurasthenic or labile-hysteroidal personal constitution. These features create the preconditions for anxiety-neurotic disorders associated with anticipation of the onset of menstruation, corresponding discomfort or further pain, if painful menstruation has already been experienced. Sometimes primary algodismenorrhea is noted already at menarche or shortly after the start of the menstrual cycle. A psychogenic decrease in the pain threshold, according to this hypothesis, leads to the fact that any physiological sensations associated with a neurotic dominant, to which normally the brain simply “does not pay attention,” are perceived in advance as painful in disorders of this kind.
Without detracting from the significance of the psychogenic factor, supporters of the biochemical hypothesis see the main cause of primary algodismenorrhea in the abnormal, excessive production of prostaglandins - biologically active substances that regulate many processes (including changes in the muscle tone of the uterus, the “behavior” of blood vessels, inflammatory responses, the intensity of pain, and many others). .). If they are in excess, transient spasms and ischemic phenomena may occur, i.e. deficiency of blood supply to the uterine endometrium. Just as the brain is notified of ischemia or myocardial infarction by an intense pain signal, menalgia can be caused in a similar way. This interpretation is currently recognized by most experts and is satisfactorily confirmed by clinical practice.
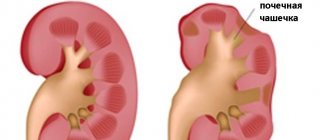
As for secondary algodismenorrhea, it is always a consequence of one or another organic pathology.
The most common cause is endometriosis, but painful menstruation can also be caused by urogenital infections or inflammation of a different nature, benign and malignant neoplasms, adhesions, etc.
Visit our Gynecology page
3. Symptoms and diagnosis
By definition, the leading and obligate (mandatory for diagnosis) symptom is pain accompanying the period of menstruation or occurring immediately before it. The severity of pain can be so great that a woman literally falls out of her usual way of life for several days, losing her ability to work and the ability to carry out any active activity. Many patients experience irradiation of pain in the back, legs, groin and other areas. In addition, the etiology of algodismenorrhea determines the presence of additional symptoms in various combinations: weakness, headache, flatulence, dyspepsia, dysuria, general malaise with fever, dry mouth, syncope, etc.
The primary task in diagnosing algodismenorrhea is to identify or confirm organic pathology.
In other words, first of all it is necessary to establish whether the pain syndrome is primary (psychogenic or hormonally caused), or whether it is just the tip of a pathological iceberg, otherwise progressing latently. For the purpose of differential diagnosis, the anamnesis is carefully studied, the nature of the complaints, the mental and somatic characteristics of the patient, her age, social and reproductive status are analyzed. A thorough laboratory and instrumental examination is prescribed (the choice of methods today is very wide and is determined by the gynecologist, based on specific indications and the most likely clinical assumptions). Only after background gynecological diseases and endocrine disorders have been conclusively excluded can we say that algodismenorrhea is of a primary (functional, essential) nature.
About our clinic Chistye Prudy metro station Medintercom page!
Popular questions
Good afternoon
There were complaints of severe pain in the lower abdomen during menstruation. The doctor prescribed me to take Duphaston for 10 days, and then, from the 1st day of my period, to take Dicyclen for 6 months. Is it possible to drink duphaston during menstruation? And should diecyclen be taken only during menstruation? Hello! Taking duphaston helps regulate the cycle due to the correction of phase 2, so its use ends on day 26 with a regular cycle. Next, you are prescribed a contraceptive drug that is taken on a 21-day, 7-day break regimen for 6 months. This will relieve pain during menstruation.
I have lingering pain in the lower abdomen before my period. During sex I feel a strong unpleasant odor and sometimes pain during intercourse. My discharge is white and of medium thickness. Menstruation lasts for six days: the first three days are very heavy, the remaining days are droplets. I have been recovering from this disease for three years now. The doctors told me that I have endometritis, thrush and a whole series of other incomprehensible words. At another hospital, upon examination, I was told that I had cervical erosion. The third hospital reported that I had papillomas and vaginitis. I don’t know which of these hospitals to trust((
Hello! It is impossible to establish an accurate diagnosis without examination. I recommend conducting the examination again.
Hello, I am suffering from very severe pain in the lower abdomen, clear discharge and my cervix has dropped very much!
Hello! You need to see a doctor as soon as possible and conduct an examination - ultrasound of the pelvic organs to exclude acute gynecological pathology.
Hello. A week ago, pain began when urinating, after which there was also pain, only plus a burning sensation in the vagina. Cause and treatment. Thank you.
Hello!
To determine the cause, an examination is carried out - a general urine test, Nechiporenko's test, bacteriuria, as well as an ultrasound of the bladder and kidneys. Based on the results, the urologist can accurately formulate a diagnosis and recommend treatment. Burning in the genital tract - this can be either a descending path of inflammation or an isolated disease. This also requires clarification. For an accurate diagnosis, contact a specialist
4.Treatment
It should be noted, in continuation of the comparative analysis of the primary and secondary forms, that there is still an idea that algodismenorrhea is something like a “growing disease” that occurs all the time, does not require treatment and disappears without a trace after marriage and first birth. This is not only wrong, but often the exact opposite of what actually happens. It is with the onset of regular sexual activity, with the onset of pregnancy, during the gestation period that latent pathology of the reproductive system can manifest itself, the harbinger or only symptom of which was previously “ordinary” menstrual pain. No pain syndrome should accompany critical days - for the female body this is a completely normal physiological process, and it should not turn into a painful disease with a cyclical course. Therefore, the very complaint that many patients perceive as something inherent in almost any woman, insignificant and not worthy of mention in a conversation with a doctor - painful menstruation - is in fact a clear reason for contacting a gynecologist, even if there are no other complaints or violations.
Based on the results of the examination (see above), one or another treatment regimen is prescribed; It is obvious that these schemes are too individual and diverse (depending on the form and specific etiology of algodismenorrhea) to be described in detail or even listed. Let us only note that the most effective is an integrated approach, including, first of all, treatment of the underlying disease (if it is identified, i.e. in the secondary form of algomenorrhea), prostaglandin inhibitors (nonsteroidal anti-inflammatory drugs, NSAIDs), according to indications - painkillers, antispasmodics, sedatives, vitamin complexes, physiotherapeutic procedures.
Attention is necessarily paid to the normalization of lifestyle and psychological microclimate; with primary algodismenorrhea, a special course of psychocorrection is often also necessary.
Folk remedies for algodismenorrhea
It is important to understand that with algodismenorrhea it is forbidden to self-medicate; therapy can only be carried out by an experienced gynecologist. However, before the popularization of this disease, several folk remedies appeared that can help partially relieve (but not cure!) the pain symptom at home.
- Infusion of elecampane root: 1 tablespoon per 500 ml of boiling water, heat for 15 minutes in a water bath and leave for half an hour in a warm place. Drink the strained solution 1 tablespoon three times a day.
- Herbal tea made from chamomile and lemon balm (mix 1:1) is a recognized natural pain reliever. 40 grams of dried plants are poured with 1 liter of boiling water: after an hour the drink is ready for use. 3 days before the start of menstruation, you need to drink 100 g of tea 3 times a day before meals.
- Pour 2 tablespoons of dried hare cabbage into 500 ml of boiling water and let stand for an hour. Drink half a glass of the strained infusion 3 times a day. Course of treatment: three times, 2 weeks of admission alternated with 2 weeks of rest after menstruation.
- A week before critical days, the following infusion relieves tension and pain: in a 2:1 ratio, eucalyptus and eleutherococcus leaves are poured into a glass of boiling water and infused for 30 minutes. Take 2 tablespoons three times a day before meals.
- A decoction of dandelion roots copes well with the symptoms of algodismenorrhea. 8-10 days before the expected period, 1 teaspoon of dandelion root is poured into a glass of water and boiled over low heat for 5 minutes, after which it is placed in a dark place for two hours. Half a glass of this drink with the addition of mint or lavender leaves 2 times a day before meals perfectly relieves nervousness, calms you down and relieves pain.
- A proven method is a three-week course of infusion of mantle and yarrow. To prepare it, mix the plants 1:1, add a liter of hot water and leave for 30 minutes. 2-3 glasses of decoction will relieve severe menstrual pain.
- A herbal mixture of valerian root, mint leaves and chamomile flowers will relieve irritability and put your nerves in order. In a ratio of 1:1:2 herbs, pour 200 ml of boiling water and let it brew. Take 2 tablespoons 15-20 minutes after breakfast, lunch and dinner.
- Make a collection of black elderberry and lemon balm flowers in a 1:2 ratio. Pour a tablespoon of the mixture into a glass of boiling water, hold for 20 minutes in a warm place and drink in one gulp. If necessary, you can drink another glass of this decoction in the evening.
- To normalize the painful menstrual cycle, a collection of equally proportionally mixed peppermint, motherwort pentaloba, birch buds, and chamomile is recommended (take 200 ml 4 times a day).
In addition, for algodismenorrhea, traditional medicine often uses such medicinal plants as: anise, chamomile, caraway seeds, fennel, fennel, hops, motherwort five-lobed, oregano, viburnum, lemon balm.
It is important to remember that these recipes only alleviate symptoms and sometimes enhance the effect of medications, but are not full-fledged therapy. And if you do not have the desire or opportunity to prepare decoctions according to folk recipes yourself, try evening primrose oil GINOCOMFORT - this drug is a source of Omega-6 polyunsaturated fatty acids, and its course use helps reduce the manifestation of premenstrual syndrome.
Evening primrose blocks the production of prolactin, which can cause pain, and also improves the synthesis of substances responsible for regulating the menstrual cycle.
The product was created by specialists from the pharmaceutical company VERTEX and has a complete list of necessary documents and certificates.
Cardiologist Herman Gandelman about painful menstruation. Source – JIt Zdorovo