Acute pyelonephritis is a nonspecific inflammatory disease of the kidneys. Bacterial attack plays a direct role in the occurrence of the disease. Penetration of bacterial agents into the kidneys occurs through the bloodstream or from the urinary tract.
The inflammatory process affects the pyelocaliceal system and interstitial renal tissues. Acute pyelonephritis most often affects women and small children. This is explained by anatomical features and physiology.
What are the stages of the disease?
The clinical course of acute pyelonephritis has several stages. Each of them develops in accordance with the pathomorphological changes occurring in the kidneys.
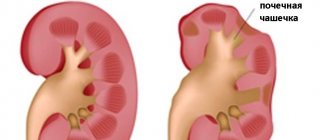
At the initial stage of pathological development, serous inflammation occurs. This stage is characterized by a slight increase in kidney tension and perivascular infiltration. If a specialist is contacted in a timely manner, the patient is prescribed conservative therapy, with the help of which the inflammatory process is replicated. The patient makes a full recovery. If there is no treatment at the initial stage, the disease will progress, and purulent-destructive kidney damage will subsequently occur.
The next stage is called apostematous pyelonephritis. This is an inflammatory disease when pustular formations are formed, localized in the renal cortex. If there is no adequate therapy, such pustules will merge and form a large purulent focus. It is called a kidney carbuncle. When this condition develops, the risk of kidney abscess formation increases. Purulent contents can spill into the perinephric tissue. If treatment is started in a timely manner, the infiltration lesion heals, scars are formed, which consist of connective tissues.
Pathomorphology
The following morphological forms of acute pyelonephritis are distinguished:
- purulent
- serous
- purulent with mesenchymal reaction
In chronic pyelonephritis, the inflammatory process is focal and polymorphic. Histological changes can be different; a common morphological sign is lymphohistiocytic infiltration. The same changes can occur with endemic Balkan nephropathy, chronic tubulointerstitial nephritis while taking analgesic drugs, and primary changes in the vessels of the kidneys. Chronic pyelonephritis differs from other kidney diseases by the simultaneous involvement of the pyelocaliceal system of the organ. Changes in the kidneys as the process progresses are characterized as focal, uneven and asymmetrical.
What are risk factors?
There are a number of extrasexual factors that increase the risk of developing acute pyelonephritis:
- Congenital or acquired anomaly, pathology of the structure of the kidneys and other organs of the urinary system.
- AIDS virus.
- Urolithiasis disease.
- Diabetes. With increased sugar content in the urine, pathogenic microorganisms will multiply.
- Age.
- The spinal cord and peritoneal organs are injured.
- Surgery or other medical intervention on the urinary system.
- Bacterial chronic disease, the presence of an infectious focus in the body.
The occurrence of acute pyelonephritis in a man may be associated with prostate disease and an increase in its size.
What is pyelonephritis
Pyelonephritis is an infectious nonspecific kidney disease caused by bacteria.
With pyelonephritis, the kidney tissue and the tubular system that removes urine are affected sequentially or simultaneously: tubules, calyxes, pelvis. The disease is very common; this diagnosis is given to 2/3 of patients who consult a urologist about pain and other urinary disorders. Pyelonephritis can be asymptomatic or occur as an acute inflammatory process. But even with a hidden course, there is a risk of impaired excretory function of the kidneys (renal failure) and the spread of infection throughout the body (sepsis).
Most often, children under 7 years of age, young women during pregnancy or at the beginning of sexual relations, and older men (against the background of prostate adenoma) suffer from pyelonephritis.
Why does acute pyelonephritis occur?
Movement of infection along an ascending path
The infection enters the bladder through the urethra, then spreads to the canals of the upper structures, then to the kidneys. This is the most common cause of the development of acute pyelonephritis.
This disease is more common in women. The fact is that their urethra is shorter and wider than that of men. The urethra is located in close proximity to the genitals and anus, as a result of which pathogenic microorganisms penetrate into the bladder and then into the kidneys without any difficulty.
As for men, acute pyelonephritis develops due to the presence of an obstruction in the urethra, when it becomes difficult to excrete urine. As a result, it stagnates. As an obstacle, we mean kidney stones, as well as if the prostate tissue has grown. The fluid accumulates, and infectious agents multiply and spread to the organs that produce and filter it.
Women can also develop acute pyelonephritis due to the presence of a cyst, stone, tumor formation, or stricture.
Vesiculourethral reflux
With vesiculourethral reflux, a certain amount of urine backflows. It will be located in the renal pelvis. This happens because the outflow through the ureter is obstructed.
This pathology, which causes inflammation in the kidneys, is in most cases diagnosed in children. An attack of an acute form of the disease in a child is dangerous due to its complications. Scarring of the kidney tissue may occur.
During puberty, an attack of acute pyelonephritis and tissue scarring occurs due to certain physiological characteristics. Namely:
- Low fluid pressure compared to an adult body.
- Children under 5 years of age are unable to completely empty their bladder.
- Reduced immune resistance of the child during the first years of life. This also includes a bacterial infection, since personal hygiene may be insufficiently observed, and there are also no bactericidal components in the urine.
- The disease is difficult to diagnose at an early stage.
- Unlike adults, the descending route of infection is more common in children. The cause may be tonsillitis, caries, scarlet fever and more.
There is a significant decrease in kidney function if tissue begins to scar. Approximately 10% of patients who require hemodialysis develop scar tissue due to pyelonephritis, which they suffered in childhood.
Infectious agent
The most common pathogenic microorganism that provokes the development of pyelonephritis is Escherichia coli. In addition, there are other causative agents of the disease. Namely:
- Staphylococci.
- Proteas.
- Enterococcus.
- Pseudomonas.
- Pseudomonas aeruginosa.
- Enterobacter.
- Pathogenic fungal microorganism.
If the infection moves along an ascending path, E. coli will be present in the urine discharged. It can be determined by undergoing laboratory testing. If the pathogen is introduced during instrumental manipulation, the causes of the disease include Klebsiella, Proteus, and Pseudomonas aeruginosa.
Pyelonephritis: clinical picture, diagnosis and treatment
Pyelonephritis is understood as a nonspecific inflammatory process in which not only the pelvis and calyces of the kidney are involved, but also, mainly, the renal parenchyma with predominant damage to its interstitial tissue.
Acute pyelonephritis should be understood as an acute infectious and inflammatory process in the renal parenchyma of varying degrees of intensity.
Chronic pyelonephritis can be a consequence of the transition of acute pyelonephritis to the chronic stage or arise from the very beginning as a primary chronic process. Chronic pyelonephritis is a sluggish, periodically exacerbating bacterial inflammation of the kidney and urothelium of the pelvis, followed by sclerosis of the parenchyma, complicated by hypertension and renal failure.
Pyelonephritis can be considered as an independent disease, as well as as a complication of a variety of diseases (acute renal failure, urolithiasis, prostate hyperplasia and cancer, gynecological diseases). Pyelonephritis occurs in a variety of circumstances: postoperative period, pregnancy. The incidence of pyelonephritis among men and women of different ages is not the same. In general, women predominate among patients with pyelonephritis. At the age of 2 to 15 years, girls suffer from pyelonephritis 6 times more often than boys; almost the same ratio remains between men and women of young and middle age. In old age, pyelonephritis occurs more often in men. This is due to the fact that for men and women of different ages there are characteristic urodynamic disorders and it is for this group of patients that diseases associated with urinary tract infections occur. In young women, inflammatory diseases of the genitals, defloration cystitis and gestational pyelonephritis are more common; in older men, prostatic hyperplasia is more common. An important role is played by age-related physiological changes in the organs of the urinary system: the elastic properties of the tissues of the urinary tract and their tone decrease, dyskinesias appear, leading to urodynamic disorders. The problem of the relationship between bacteriuria and pyelonephritis seems to be important from a practical point of view.
Pyelonephritis is usually accompanied by bacteriuria, which in some cases may precede the development of the disease. However, it may be absent in cases where there is obstruction of the corresponding ureter or a “localized” purulent focus in the kidney. The presence of bacteriuria does not mean that the patient has or will definitely develop pyelonephritis; however, the absence of bacteriuria does not contradict the diagnosis of pyelonephritis. Knowledge of diagnostic techniques and adequate treatment of urinary tract infections is necessary for doctors of various specialties.
There is no uniform classification of pyelonephritis. In clinical practice, it is customary to divide pyelonephritis according to the nature of its course into acute and chronic, primary and secondary (that is, uncomplicated or complicated). Complicated is pyelonephritis that occurs due to pre-existing urological pathology and urodynamic disorders. There are also pyelonephritis in children, pregnant women, the elderly (senile pyelonephritis), pyelonephritis developing in diabetes mellitus, etc.
Classification of pyelonephritis (N. A. Lopatkin)
Pyelonephritis:
- one-sided or two-sided;
- primary or secondary;
- acute or chronic;
- serous, purulent or necrotizing papillitis;
- phase of active inflammation, latent, remission;
- apostematous pyelonephritis, renal carbuncle, renal abscess, renal scarring, or pyonephrosis.
Etiology and pathogenesis
Causative agents of urinary infections. The most common causative agent of urinary tract infections is Escherichia coli; other gram-negative microorganisms, as well as staphylococci and enterococci, are less common. The role of the latter microorganisms increases in chronic processes and nosocomial infections. Approximately 20% of patients have microbial associations; the most common combination is Escherichia coli and enterococcus. The patient may experience a change in the causative agent of the infectious process, resulting in the appearance of multidrug-resistant forms of microorganisms. This is especially dangerous with uncontrolled and unsystematic use of antibacterial drugs. It should be noted that the patient’s own normal or opportunistic flora, which is normally present in the urinary tract, upon admission to the hospital is very quickly (within two to three days) replaced by hospital-acquired resistant strains. Therefore, infections that develop in a hospital are much more severe than those that occur at home. In addition to the “normal” bacterial flora, urinary tract infections are often caused by protoplasts and L-forms of bacteria. With pyelonephritis, a chronic infection can be maintained by protoplasts for a very long time, for many years.
Pathological anatomy
Acute and chronic pyelonephritis is characterized by focality and polymorphic morphological changes. With a bilateral process, kidney damage turns out to be uneven; as for a unilateral process, in this case, too, there is an unequal degree of damage to different areas. Along with healthy areas, foci of inflammation and sclerosis can be detected in the patient. In acute pyelonephritis, the kidney increases in size and its capsule thickens. During decapsulation, the surface of the kidney bleeds and, as a rule, perinephritis occurs. A section of the kidney reveals wedge-shaped areas of yellowish color, tapering towards the hilus. Microscopically, numerous perivascular infiltrates with a tendency to form abscesses are detected in the interstitial tissue. Pus and bacteria from the interstitial tissue penetrate the lumen of the tubules. Miliary abscesses in the cortex, considered a characteristic feature of apostematous nephritis, form in the glomeruli. At the same time, due to embolism of the capillaries around the tubules, pustules may appear in the medulla of the kidney. In addition, purulent gray-yellow stripes form in the medulla of the kidney, spreading all the way to the papillae. During microscopic examination, accumulations of leukocytes are found both in the straight tubules and in the surrounding tissue. This process can lead to necrosis of the papilla, which, however, is more typical for chronic pyelonephritis (Pytel Yu. A., 1967). The cause of necrosis of the papilla is considered to be a violation of the blood supply in it. Small abscesses can merge to form an abscess.
Diagnosis of pyelonephritis
The clinical picture of acute pyelonephritis is characterized by a combination of general and local signs of the disease. The first include severe general condition, extremely severe chills, high body temperature, severe sweating, changes in the blood, signs of general intoxication (nausea, vomiting, muscle and joint pain). Local symptoms: pain, spontaneous and provoked during examination of the patient, muscle tension in the lower back and hypochondrium, changes in urine. Sometimes there is frequent and painful urination. In recent years, there has been a tendency towards an asymptomatic and latent course of pyelonephritis, which makes it difficult to recognize not only its chronic, but sometimes its acute form. Acute pyelonephritis may remain unrecognized, and exacerbations of a process that has already become chronic in some cases go unnoticed or are interpreted incorrectly (acute respiratory infections, exacerbation of gynecological pathology, lumbago).
As a result, pyelonephritis is often diagnosed accidentally - during examination for another disease - or in the later stages of the disease (with the development of arterial hypertension, uremia, urolithiasis). The difficulty of diagnosis also lies in the fact that in subclinical form pyelonephritis can last for years. As a result, instrumental examination methods often make it possible to detect the disease quite late. Therefore, when diagnosing pyelonephritis, one must remember several key factors. Firstly, pyelonephritis affects mainly women. This is facilitated by the anatomical and physiological features of the female body, such as the relatively short and wide female urethra, which facilitates the development of an ascending infection (while in men it is long and tortuous, which prevents an ascending infection or “closes” it to the prostate, testicles and/or their appendages , seminal vesicles); topographic proximity of the genital tract and rectum, which are often sources of bacterial contamination; features of hormonal levels, which change significantly during pregnancy (with the development of ureteral hypotension), menopause (with the development of atrophic colpitis). The use of various contraceptives may also be a risk factor. Secondly, pyelonephritis develops quite rarely in boys and young men, in contrast to older men or old men, who often experience bladder outlet obstruction (due to adenoma or prostate cancer). Other reasons for the development of pyelonephritis in this category of patients include obstructive uropathy, vesicoureteral reflux (VUR), polycystic kidney disease (which may not be accompanied by a urinary infection) or an immunodeficiency state (diabetes mellitus, tuberculosis). Thirdly, with the help of targeted questioning, it is possible to identify clear signs of the development of pyelonephritis, even if it is asymptomatic. For example, the chills mentioned above with pyelonephritis can occur quite regularly over many months and years, not only in the cold, but also in the heat. The doctor's attention should also be drawn to episodes of cystitis, especially recurrent cystitis; however, one should remember the existence of cystalgia, dysuria and pollakiuria, not associated with a urinary infection - with prolapse of the pelvic floor, with kinking of the urethra in obese and elderly women, with sexual excesses, with abuse of salty and spicy foods, with hysteria and neurasthenia . An important symptom of pyelonephritis is nocturia, especially observed over many months and even years and not associated with excessive fluid intake at night. Nocturia is not specific for pyelonephritis; it simply reflects a decrease in the concentration function of the kidneys in any chronic progressive nephropathy. With pyelonephritis, nocturia develops quite early - due to damage to tubulostromal structures. Arterial hypertension (AH) is a companion and complication primarily of chronic pyelonephritis. Due to the high prevalence of hypertension, which correlates with age, this symptom is not very specific in elderly and senile people. However, the development of arterial hypertension in young people (especially in the absence of it in the family history) in combination with other symptoms of pyelonephritis should alert and prompt a diagnostic search in the appropriate direction. Further, there are a number of conditions that are likely to contribute to the development of pyelonephritis or are complicated by its formation. These include nephroptosis, PMR, urolithiasis, diabetes mellitus and some others. The role of these conditions should not be absolute, since they can sometimes last for years without leading to pyelonephritis. It is no coincidence, however, that the subject of debate still remains the question: what factors lead to damage to the renal parenchyma with its subsequent scarring - PMR itself, urolithiasis and other similar disorders, or the addition of a urinary infection. Factors that at first glance may seem secondary and indirect deserve close attention because the diagnostic criteria for pyelonephritis (primarily chronic) are quite vague and vague.
Laboratory diagnostics
Clinical urine analysis reveals a characteristic increase in the number of leukocytes (leukocyturia). A direct correlation between the degree of leukocyturia and the severity of pyelonephritis does not always exist. Test data should always be compared with complaints, anamnesis and clinical picture. For example, asymptomatic leukocyturia up to 40, 60 and even 80 or 100 leukocytes in the field of view, detected in a woman who has neither clinical manifestations nor a history of pyelonephritis, requires the exclusion of gynecological pathology. In another situation, for example, with a combination of high temperature and minimal leukocyturia, data from anamnestic, clinical, laboratory and instrumental examination are required. Proteinuria in pyelonephritis, as a rule, is minimal or completely absent, although in some cases this figure exceeds 1 g/l. The pH value of urine deserves attention. So, normally, the acidic reaction of urine during a urinary infection can change to alkaline (sharply alkaline). An alkaline reaction of urine, however, can also be observed in other conditions: impaired ability of the kidneys to acidify urine (with uremia), consumption of dairy and plant foods, pregnancy, etc. In addition, with an alkaline reaction of urine, destruction of blood leukocytes occurs, which can lead to erroneous interpretation of urine test results.
Urine culture. Theoretically, this method is almost ideal for identifying the pathogen and selecting an adequate antibacterial drug. However, in real clinical practice this is prevented by a number of objective reasons.
Firstly, a single urine culture gives at least 20% of false-positive results, and therefore triple culture is generally accepted; at the same time, it takes from several days to a week to obtain the results of triple culture, and in these conditions it is often necessary to start treatment without waiting for the culture results.
Secondly, it is problematic to collect the average portion of urine required for culture in infants, children, the elderly, people with paraplegia, women with menstrual or purulent vaginal discharge, in postoperative patients and postpartum women. Collecting urine using a catheter is currently not recommended due to the high risk of ascending infection.
Thirdly, in the absence of bacteriuria, the likelihood of culturing a bacterial culture is reduced. Finally, the question remains unresolved as to whether the very microbes that gave rise to growth actually support the inflammatory process in the kidneys. Nevertheless, urine culture is used to identify the causative agent of pyelonephritis and is important for the choice of antibacterial therapy. The detection of at least 100,000 microbial bodies per 1 ml of urine (102–103/ml) is considered reliable. Instrumental diagnostics are carried out using ultrasound, X-ray, radionuclide methods, and less often - endourological methods (cystoscopy, etc.).
Ultrasound examination (ultrasound). With ultrasound in patients with pyelonephritis, one can observe expansion of the renal pelvis, coarsening of the contour of the calyces, heterogeneity of the parenchyma with areas of scarring (the latter is usually determined only after years of chronic pyelonephritis). Delayed manifestations of the disease include deformation of the contour of the kidney, a decrease in its linear dimensions and parenchyma thickness, which, however, is not entirely specific and can be observed in other nephropathies. Thus, with glomerulonephritis, scarring and shrinkage of the kidney always occurs quite symmetrically, while with pyelonephritis, even a bilateral process can be characterized by asymmetry. Ultrasound can identify concomitant urolithiasis, VUR, neurogenic bladder, polycystic kidney disease, obstructive uropathy (for the diagnosis of which contrast contrast of the urinary tract can be used) and some other conditions that cause or support the chronic course of pyelonephritis.
Survey urography is not informative enough: it only allows one to identify the position and contours of the kidneys (if they are not covered by the shadows of intestinal loops) and X-ray positive stones. At the same time, radiocontrast methods have a number of advantages over ultrasound in terms of visualization of the urinary tract, detection of obstructive uropathy, urinary leaks, as well as in a number of other situations. As with ultrasound, the X-ray picture of chronic pyelonephritis is also not entirely specific and consists of coarsening or deformation of the calyces, dilatation and hypotension of the pelvis, deformation of the contours of the kidney and thinning of the parenchyma.
Computed tomography can be used to diagnose pyelonephritis, however, this method does not have significant advantages over ultrasound and is used mainly to differentiate pyelonephritis from tumor processes.
Radionuclide diagnostic methods include the use of 123I-sodium iodohippurate (hippuran), 99mTc-dimercaptosuccinic acid (DMSA) and 99mTc-diethylenetriamine pentaacetic acid (DTPA). It is believed that radionuclide methods make it possible to identify functioning parenchyma, delimiting areas of scarring, which has differential diagnostic and prognostic significance.
Treatment of pyelonephritis
An important place in the treatment of patients with acute pyelonephritis is occupied by regimen, nutrition, and the use of antibacterial agents. In case of urinogenous infection with the presence of an obstruction to the outflow of urine, the listed measures are effective only when eliminating urinary tract obstruction and urinary stasis. Also, during periods of exacerbation of the disease, methods aimed at improving microcirculation and detoxification are used. During the period of remission, herbal medicine is performed.
Antibiotic therapy. For acute pyelonephritis, the duration of therapy ranges from 5 days to 2 weeks. It is preferable to begin treatment with parenteral administration of antibacterial agents, then moving on to oral administration. Modern drugs include fluoroquinolones (tavanic 250-500 mg once daily) or β-lactams. III and IV generation of cephalosporins, semisynthetic or ureidopenicillins, monobactams, penems and β-lactamase inhibitors are also used: ceftriaxone (2 g once a day intramuscularly), cefazolin (1 g 3 times a day), amoxicillin (0.5 - 1 g 3 times a day intramuscularly, 0.25 or 0.5 g 3 times a day orally), ipipenem/cilastin (0.5 g/0.5 g 3 times a day intramuscularly), amoxicillin/clavulanic acid (amoxiclav, augmentin; 1 g 3 times a day intravenously, 0.25-0.5 g 3 times a day orally), ampicillin/sulbactam (Sultasin). Despite the potential oto- and nephrotoxicity (requiring monitoring of kidney function), aminoglycosides retain their positions: gentamicin, tobramycin (old generation). Netilmicin (new generation) has low toxicity, but is used infrequently due to its high cost. Amikacin should be prescribed when treating patients with resistant strains. At the beginning of treatment with aminoglycosides, high doses are recommended (2.5-3 mg/kg per day), which can then be reduced to maintenance doses (1-1.5 mg/kg per day). The frequency of administration can vary from 3 to 1 time per day (in the latter case, it is recommended to administer drugs at a dose of 5 mg/kg, which is considered more effective and less toxic). Modern tetracyclines (doxycycline, doxibene) and macrolides (sumamed, rulid) are also effective in the treatment of pyelonephritis. Therapeutic tactics for treating acute and exacerbations of chronic pyelonephritis are similar; in addition to the mentioned chemotherapy drugs, trimethoprim (Biseptol; 0.48 g 2-4 times a day) or nalidixic acid preparations (Nevrigramon, Negram; 1 g 4 times a day) and its modifications (Palin, Pimidel; 0.4) are also prescribed orally g 2 times a day). With chronic pyelonephritis, it is impossible to sterilize the urinary tract, so treatment is aimed at stopping exacerbations and preventing relapses. To do this, it is recommended to use courses of preventive chemotherapy, less intense than that prescribed in case of exacerbations. This tactic, however, is fraught with the development of flora resistance and side effects as a result of taking medications, so herbal medicine can serve as an alternative in this case to some extent. When choosing an antibiotic you should consider:
- previous treatment data;
- the need for dosing of antibacterial agents depending on kidney function;
- features of the pharmacokinetics of antibiotics;
- acidity of urine;
The duration of treatment depends on the clinical effect and elimination of the pathogen; therapy should be carried out in combination with bacteriological examinations of urine.
Chemotherapy prevention of relapses and recurrent infections
Prevention of exacerbations is carried out in patients with chronic pyelonephritis, occurring without significant exacerbations or against the background of constantly acting provocative factors (for example, in the presence of a stone in the renal pelvis). As a rule, antibacterial agents are prescribed in short courses of 7-10 days every month for 0.5-1 year. Usually, in the interval between courses of antibacterial therapy, herbal treatment is carried out. Antibacterial agents with bacteriostatic action are used - sulfonamides, nitrofurans, nalidixic acid. Against the background of such therapy, it is not possible to identify the pathogen, since the microorganism present at the beginning changes, as well as its resistance to antibacterial drugs. Therefore, it is advisable to carry out therapy sequentially with drugs from different groups, alternating the prescription of antibacterial agents with a different spectrum of antibacterial activity. In elderly patients, prophylactic use of antibacterial agents is usually not indicated, given the fact that the risk of complications of therapy may outweigh the potential benefits of treatment.
The prophylactic use of antibacterial agents in patients with pyelonephritis over 60 years of age may be considered justified in cases of frequent and severe relapses of infection, as well as in complicated pyelonephritis (prostate adenoma, urolithiasis, decompensated diabetes, neurological pathology with dysfunction of the pelvic organs), in the presence of asymptomatic bacteriuria, in the presence of a cystostomy or a ureteric-intestinal anastomosis. In elderly patients, non-drug measures are of paramount importance in the prevention of relapses and repeated kidney infections, including the selection of an adequate drinking regimen - 1.2-1.5 liters daily (should be used with caution in patients with impaired cardiac function), the use of herbal medicine.
Surgery
In cases where conservative therapy using antibiotics and other drugs, as well as ureteral catheterization in order to restore the patency of the upper urinary tract, are not successful, and the patient’s condition remains severe or worsens, surgical treatment is indicated. They operate mainly on purulent forms of pyelonephritis - apostemas and carbuncles of the kidney. The question of the nature of the operation is finally decided at the time of the surgical intervention itself and is determined both by the scale of the lesion and the pathogenesis of the disease. The purpose of the operation is to stop the progression of the purulent-inflammatory process in the affected kidney, prevent its occurrence in the healthy contralateral kidney, and restore the outflow of urine through the upper urinary tract if it is impaired. The surgical procedure consists of exposing the kidney (lumbotomy, decapsulation) and draining it by nephrostomy.
Conclusion
Treatment of patients with pyelonephritis should be comprehensive. In case of acute pyelonephritis, it should end with recovery; it is also necessary to exclude the possibility of the disease transitioning to the chronic stage. In case of chronic pyelonephritis, it is necessary to eliminate the active inflammatory process, eliminate the possibility of repeated attacks, and long-term follow-up of the patient. To achieve these goals, both etiotropic and pathogenetic therapy should be used. In the fight against infection, one should also not forget about increasing the body's resistance. Timely elimination of pathological changes in the kidneys and urinary tract predisposing to the occurrence of pyelonephritis makes it possible not only to prevent pyelonephritis, but also to achieve a better therapeutic effect if the disease has already occurred. All these measures can be considered as effective as possible, subject to the fruitful cooperation of doctors of all specialties - urologists and therapists, surgeons and gynecologists - in the treatment of patients with pyelonephritis.
A. D. Kaprin, Doctor of Medical Sciences R. A. Gafanov, K. N. Milenin RRC of X-ray Radiology, Ministry of Health of the Russian Federation, Moscow
Characteristics of microflora in complicated urinary tract infections
| Pathogens | % |
| Gram-negative | |
| Escherichia coli | 21 |
| Proteus spp. | 7 |
| Klebsiella spp. | 2 |
| Enterobacter agglomerans | 19 |
| Serratia marcescens | 4 |
| Pseudomonas aeruginosa | 18 |
| Acinetobacter spp. | 2 |
| Citrobacter spp. | 1 |
| Providencia spp., Morganella spp. | 5 |
| Gram-positive | |
| Staphyloccus epidermidis | 6 |
| Staphylococcus aureus | 3 |
| Staphyloccus saprophyticus | 4 |
| Enterococcus faecalis | 8 |
Signs of the disease in women
Women are most susceptible to developing pyelonephritis. Symptoms of the disease may vary depending on its form. As a rule, signs of acute pyelonephritis in a woman are:
- Change in the color and odor of urine. The fluid may become cloudy and contain bloody or purulent inclusions.
- Increased body temperature above 38 degrees. In some cases, there is a sharp change in indicators.
- Burning sensation when urinating, frequent visits to the toilet.
- Nausea, accompanied by vomiting, chills.
- Having a headache.
- Painful sensations when tapping with the edge of the palm in the kidney area.
Symptoms
Pyelonephritis is divided into acute and chronic.
Acute is divided into primary pyelonephritis, which can develop in a practically healthy person, and secondary, which, in turn, can be obstructive and non-obstructive. A secondary obstructive process occurs when the outflow of urine is disrupted (a tumor blocking the ureters, their blockage with a stone and other conditions), and a secondary non-obstructive process occurs as a result of ascending (urinogenic) infection in inflammatory diseases of the urinary tract (urethritis, cystitis).
Chronic pyelonephritis can be a consequence of acute or occur as an independent disease.
The symptoms of an acute disease differ from the symptoms of a chronic one, however, secondary obstructive pyelonephritis has some similarities with the chronic process, so it is often difficult to differentiate them, in such cases the formulation “not specified as acute or chronic” can be used.
Acute pyelonephritis
The acute process is characterized by a sharp onset with an increase in body temperature to 38-39 °C and chills. The general condition is disturbed - weakness, headache, thirst appear, and with severe intoxication, nausea and vomiting are possible. There is pain in the lower back on palpation and a positive Pasternatsky sign - sharp pain when tapping the kidney area on the affected side. In some cases, swelling and increased blood pressure may occur.
With secondary pyelonephritis, urination disorders may occur - difficulty, pain, burning. Visually, the urine may become cloudy, mixed with flakes.
Chronic pyelonephritis
It may occur without a pronounced clinical picture, accompanied by minor disturbances in the general condition: weakness, lethargy, periodically low-grade fever, mild pain in the lumbar region with irradiation to the groin area and the anterior surface of the thigh.
With a long ongoing process, the patient develops signs of intoxication (weakness, chills, anemia), swelling of the face in the morning, frequent urination, and frequent nighttime urges to go to the toilet. Arterial hypertension may develop in 50-75% of cases.
Pain on palpation and a positive Pasternatsky sign are also present in the chronic form, however, if acute pyelonephritis is more often one-sided, then chronic pyelonephritis often affects both kidneys.
During chronic pyelonephritis, stages of remission and exacerbation are distinguished. In some cases, there are no symptoms, and the pathology is detected by chance, based on test results.
Features in certain categories of patients
The symptoms of pyelonephritis have characteristics in children and the elderly. In children, symptoms of intoxication often come to the fore; abdominal syndrome may develop - pain is localized in the abdomen, and not in the lumbar region. In elderly and senile age, the disease often occurs with a blurred clinical picture; local symptoms (pain syndrome) are dominated by general symptoms (weakness, fever, intoxication).
Signs of pyelonephritis in men
Male patients are diagnosed with the disease less frequently than females. This is due to differences in the urinary system. The reasons for the development of pyelonephritis may be diseases that impede the outflow of urine from the kidneys.
As a rule, in males the disease occurs in a chronic form. Signs of the development of pyelonephritis in men are:
- Decreased appetite. Rapid fatigue of the body.
- Difficulty in urinating.
- Moderate intensity pain in the lumbar region.
- Constant thirst.
- Frequent urge to urinate.
In some cases, male patients experience bloody inclusions in their urine. This may indicate displacement of kidney stones.
Epidemiology
In the CIS countries, according to statistics, there are 15-16 cases of acute pyelonephritis per 100,000 population. There are also 18 cases of chronic pyelonephritis per 1000 population.
The peak incidence of pyelonephritis occurs in three age periods. The first one is up to 3 years old. For every 8 sick girls there is 1 sick boy. The second peak of incidence occurs during active reproductive age - from 18 to 35 years. For every 7 sick women there is 1 sick male. Elderly and senile age is the third peak of incidence. Starting from the age of 60, the number of sick women and men becomes equal. Among patients over 70 years of age, the majority are men, since they develop tumor and hypertrophic processes in the prostate gland, which disrupts the dynamics of urine.
In the first two age periods, girls and women are more likely to get sick, which is explained by the peculiarities of the hormonal status, which changes during pregnancy and leads to dilatation, hypotension and dyskinesia of the urinary tract. Also another reason is the anatomical and physiological characteristics of the urethra (it is short, the rectum and genital tract are located nearby). The increase in female morbidity is also influenced by the use of oral contraceptives.
Signs of the disease in children
In childhood patients, when the disease manifests itself, a sharp change in body temperature is observed. The indicator exceeds 38 degrees. The disease is accompanied by nausea, vomiting, chills, and girdle pain in the abdomen and lower back. In some cases, constant drowsiness is possible.
If symptoms appear in a child, you should immediately contact a specialist. It is impossible to diagnose pyelonephritis without the presence of appropriate education. The specialist will conduct diagnostic measures and prescribe the necessary treatment. Failure to go to the clinic in a timely manner can lead to the development of complications.
Signs of pyelonephritis in pregnant women
In some cases, the disease occurs in pregnant women. The form of pyelonephritis in pregnant women can be either acute or chronic. Most often the disease manifests itself at the end of the second, beginning of the third trimester.
The occurrence of pyelonephritis is promoted by an increase in the volume of the uterus. It begins to put pressure on the ureters, disrupting the normal flow of urine. With stagnation in the kidneys, pathogenic microorganisms begin to multiply.
During pregnancy, a woman's kidneys are subject to high stress. The disease can occur simultaneously with cystitis. It is impossible to diagnose pyelonephritis in a pregnant woman without specialized education and experience.
Lifestyle and prevention
During treatment and during the recovery period, diet No. 7 is indicated. Adequate hydration is important. Vigorous activity should be kept to a minimum. Patients receiving outpatient treatment can begin work two weeks after their condition returns to normal, that is, on average 21 days after the onset of the disease.
Prevention of OP consists of reducing the intensity of sexual life, conducting a preventive course of antibiotic therapy (for example, for bacteriuria in pregnant women), as well as early detection and treatment of cystitis.
If prophylactic measures have not eliminated the pathogen or reinfection or relapse (reinfection less than two weeks after completion of a course of antibiotics) has occurred, the patient should be carefully examined for anatomical, functional, or structural abnormalities of the kidneys.
What complications can there be?
With improper treatment or its absence, complications may develop. The pathology is especially dangerous for pregnant women and people with diabetes. The pathology is amenable to therapeutic treatment. Untimely or incorrect treatment contributes to the development of complications, in some cases leading to the death of the patient.
One of the complications of the disease is sepsis. If left untreated, pathogenic bacteria multiply rapidly. Once the limit is reached, microorganisms enter the bloodstream. Thus, the infection spreads throughout the body. The complication in some cases ends in the death of the patient.
In addition to sepsis, other complications may develop, such as kidney abscess, emphysematous pyelonephritis, kidney carbuncle, etc.
Diagnostic measures
If any symptoms appear, you should immediately contact a specialist. The doctor will examine, interview the patient and prescribe the necessary diagnostic measures. This allows the specialist to prescribe the correct treatment depending on the degree of development of the disease and its form. To make a diagnosis, the doctor:
1. Collects anamnesis based on the patient’s words and the studied medical documentation. The specialist pays attention to infectious diseases suffered by the patient, as well as disorders of the urinary system.
2. Interviews and examines the patient.
3. Prescribes laboratory tests and diagnostic measures using specialized equipment.
4. Tests prescribed for the diagnosis of pyelonephritis
5. To make a correct diagnosis, the specialist prescribes tests. In order to detect pyelonephritis, the following tests must be performed:
6. General blood and urine analysis.
7. Biochemical blood test.
8. Zimnitsky test.
9. Urinalysis according to Nechiporenko.
10. Bacteriological analysis of urine.
The results of blood tests can determine the presence of inflammation in the body. It is indicated by an excess of the norm in the concentration of leukocytes and the erythrocyte sedimentation rate. In addition, the biochemical composition will change.
The urine collection procedure may affect the test results. Correct collection of biomaterial involves performing a morning toilet of the external genitalia and further collecting urine. To collect biomaterial, a specialized plastic container with a lid is used. With pyelonephritis, a general urine test shows an increased level of bacteria and leukocytes. When urine density is low, its pH is alkaline. There is protein and glucose in the urine. In some cases, bloody inclusions are possible.
Conducting research using specialized equipment
To make the correct diagnosis and prescribe treatment, specialists use instrumental diagnostic methods. The doctor resorts to this method after interviewing and examining the patient. Diagnosis is carried out using the following methods:
Ultrasonography. This diagnostic method allows you to determine the density of organs and their sizes. The doctor pays attention to changes and deviations from the norm. The reflection of ultrasonic waves (echogenicity) increases in chronic pyelonephritis, and decreases unevenly in acute pyelonephritis.
CT scan. Allows the specialist to get the most complete picture.
Excretory urography. A diagnostic method that allows you to examine the kidneys and urinary tract. The patient is given a radiopaque contrast agent intravenously. After an X-ray examination, it is possible to determine the structural features of the organs of the urinary system. Contraindication to excretory urography is individual intolerance to drugs.
Cystography. The method involves filling the bladder with a radiopaque substance by excretory urography or by introducing it through the urethra. Cystography is performed to detect vesicoureteral reflux.
When carrying out diagnostic measures for female patients, the specialist prescribes a gynecological examination.