Cytomegalovirus infection is currently one of the most relevant in the structure of infectious pathology. The keen interest of specialists in this problem is due not only to the possibility of developing severe forms of this disease in newborns and children in the first year of life, but also to the potential risk of prognostically unfavorable consequences. The principles of treatment of children with CMVI provide for the simultaneous solution of several problems, including the prevention of further development and generalization of the pathological process, as well as the prevention of the formation of residual effects and disability. Treatment of children with CMV infection includes regimen, diet, etiotropic drugs, symptomatic medications, as well as immunotherapy and immunocorrection.
- Features of the infectious agent
- Methods of transmission of the disease
- Classification according to ICD-10
- Symptoms in a child
- Cytomegalovirus in infants
- Consequences in children
- Treatment of a child
Cytomegalovirus infection (CMVI, cytomegaly) is a widespread viral disease characterized by diverse manifestations, which may be asymptomatic or lead to severe generalized forms of the disease with damage to internal organs and the central nervous system, which in children often leads to disability.i Therefore, pediatricians All over the world there is an important issue of concern - how to treat cytomegalovirus in children.
Features of the infectious agent
The causative agent of CMV is the DNA virus Cytomegalovirus hominis, which was discovered in the middle of the last century. According to the international classification, CMV belongs to the group Human Herpesvirus-5 (herpes virus type 5) and has properties common to all members of the Herpesviridae family. The human CMV genome is the largest of all herpesvirus genomes.
Infection with cytomegalovirus in different countries is quite high. From 20 to 60% of children and from 40 to 95% of adults in the world are infected with this virus. Among pregnant women, the frequency of detection of antibodies to CMV according to various studies ranges from 40 to 90%. Primary CMV develops in approximately 1%. Intrauterine infection of the fetus in expectant mothers with primary CMV during pregnancy reaches 30-50%.ii But only 5-18% have manifest congenital CMV, which is characterized by a severe course and can be fatal.
Once CMV enters the body, it persists there for life. However, most people are not even aware of its presence. According to researchers, CMV infection is most widespread in developing countries, and in developed countries, in regions with low socioeconomic status. The incidence of CMV is endemic and does not vary seasonally. Endemicity is the constant presence of infectious diseases or their groups in certain territories, due to specific local natural and geographical conditions. The WHO Regional Office for Europe classifies CMV infection as a group of diseases that determine the future of infectious pathology.
Currently, an increase in the incidence of cytomegalovirus is observed in all countries of the world, which is associated both with an increase in the quality of diagnosis and with a true increase in the disease. It has been established that many seronegative women (with the absence of antibodies to CMV in the blood) of childbearing age have a high risk of infection during pregnancy and the birth of a child with congenital CMV infection.
Content
- Causes and routes of infection
- Symptoms
- Methods for diagnosing the disease
- Treatment
Cytomegalovirus is one of the types of herpes. Almost every person on earth is a carrier of the herpes virus, and most people become infected with it in childhood.
Most of the time the virus is in a “dormant” state. However, some of its manifestations can be hazardous to health.
Cytomegalovirus enters the body, like all other types of herpes. If a person’s immunity is normal, this virus may not manifest itself in any way for an unlimited amount of time.
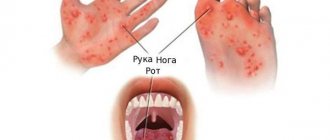
Routes of infection with CMV
The source of the virus can be urine, nasopharyngeal secretions, cervical mucus and vaginal secretions, semen, breast milk, tears, saliva, and blood. In other words, CMV can be transmitted through feeding, transfusion of blood and its preparations, contact with secretions and excreta deposited on toys and household items, as well as through all biological fluids and body secretions (saliva, urine, etc.), coughing (contact -domestic route of infection).
Scientists identify two most vulnerable periods in human life when cytomegalovirus is transmitted from person to person. First of all, this is the period of a child’s life up to 5 years. Also, transmission of the virus to a baby can occur in utero through the placenta during pregnancy, during breastfeeding, through contact and airborne droplets.[iii] The second critical period is the age of 16-30 years, when infection is most often carried out sexually.
In expectant mothers with latent CMV infection, the fetus is not always affected. A necessary condition for this is an exacerbation of the infection in the mother with the development of viremia (a condition of the body in which viruses enter the bloodstream and can spread throughout the body) and subsequent infection of the fetus. The likelihood of intrauterine disease is always significantly higher when the mother is infected during pregnancy.
Cytomegalovirus infection according to ICD 10
According to the International Classification of Diseases, congenital CMV and acquired forms are distinguished, manifested in the form of pneumonia, hepatitis, pancreatitis, infectious mononucleosis, chorioretinitis, thrombocytopenia and other diseases.
Cytomegalovirus infection is also classified according to clinical manifestations:
- latent;
- subclinical;
- clinically expressed (manifest) forms (can occur as acute, subacute and chronic infections).
The severity of the disease can be mild, moderate or severe.
With mild severity and strong immunity, damage to internal organs is insignificant and is not accompanied by functional disorders. With moderate severity, damage to internal organs is observed, which are accompanied by functional disorders. The severe form is characterized by severe intoxication and damage to internal organs with severe functional impairment.
Among the possible outcomes of the disease:
- clinical recovery with elimination of the virus from the body or its persistence in the urine;
- damage to the central nervous system with the elimination of the virus from the body or its preservation in the urine;
- death;
- transformation of the virus into a latent form.
Classification
There is no globally accepted classification system for cytomegalovirus infection (CMVI). In practice, the classification developed in 1980 is used. According to this system, CMVI is divided into:
- Congenital, can be acute, chronic.
- Acquired, can be acute, latent, generalized.
CMV infection is classified according to the duration of its course:
- Spicy.
- Protracted
- Chronic
- Recurrent.
Depending on the severity of the course, there are mild, moderate, and severe forms of the course.
Cytomegalovirus in a child: symptoms
With CMV, the incubation period ranges from 2 to 4-12 weeks. The perinatal development of the disease can be judged by identifying clinical signs of the disease in the newborn. Congenital CMV appears no later than during the first two weeks of a child’s life. If symptoms are observed later, this indicates acquired CMV infection in the postpartum period. Moreover, a child can become infected both from the mother through saliva, breast milk, and from nursing staff through airborne transmission of pathogens. Infection can also occur when donated blood is transfused into a newborn.
There are three forms of acute congenital cytomegalovirus infection:
The first form with a triad of symptoms:
a) jaundice, which in its manifestations resembles hyperbilirubinemia in newborns with gradual disappearance over two to three months;
b) hepatosplenomegaly is a secondary pathological syndrome that accompanies the course of many diseases and is characterized by a significant simultaneous increase in the size of the liver and spleen;
c) hemorrhagic syndrome - a pathological condition characterized by increased bleeding of blood vessels and manifested by petechiae (small hemorrhages on the skin), ecchymosis (large hemorrhages in the skin or mucous membrane), nasal and umbilical bleeding, hemorrhages in the sclera, hematemesis and melena - black tarry feces , which are formed due to heavy bleeding from different parts of the gastrointestinal tract.
The second form of cytomegalovirus infection
manifests itself as encephalitis with mild clinical symptoms and the following symptoms:
- increased drowsiness, convulsions, enlarged lymph nodes, impaired sucking and swallowing, tremors of the limbs;
- hypotension followed by hypertension.
Third form of CMV
manifests itself as damage to visceral organs and is characterized by high mortality in the first weeks of life.
Cytomegalovirus in infants
According to statistics, the majority of newborns do not develop CMV infection due to the presence of a high level of protective antibodies in the pregnant woman or they experience the infection in an asymptomatic form.
However, of all congenitally infected children, approximately 10% are born with symptoms of the infectious process. The nature of the damage to the fetus and newborn depends on the timing of infection and is characterized by a variety of manifestations - from serious developmental defects and generalized forms to the asymptomatic course of the infection. Of course, most often the source of infection with cytomegalovirus infection in newborns and children of the first year of life, born uninfected from mothers seropositive for CMV, is the mothers themselves. The most significant transmission factor in this case is breast milk containing the virus.
It is advisable to carry out examination of the newborn in conjunction with examination of the mother. Diagnosis of CMV infection is carried out on the basis of data from specific laboratory tests, including a blood test to detect IgG antibodies.
Prevention
Pediatricians recommend standard measures to strengthen the immune system:
- hardening;
- nutritious nutrition rich in vitamins and minerals;
- supporting vitamin courses in the autumn-winter period;
- moderate physical activity;
- walks and outdoor activities.
There is no vaccination against this disease. The developed vaccine has an effectiveness of no more than 50% and has not been widely used.
To prevent infection of the fetus, women are advised to get tested for the presence of antibodies at the planning stage of pregnancy and subsequently monitor their stress levels and immunity.
Consequences of cytomegalovirus infection in children
In the next two years after birth or later, if CMV is present in the body, a child may have defects in vision, hearing, teeth, behavioral disorders, mental retardation, and cerebral palsy.iv
In many cases, cytomegalovirus is dangerous to the life and health of a child. In the acute form of congenital CMV, the death of children occurs in the first weeks or months of life, most often from associated bacterial infections. Children who have had an acute form of the disease experience an undulating course of the chronic form of CMV infection. Congenital malformations of the central nervous system often form, in particular microcephaly - in almost 40% of cases. Chronic hepatitis may develop, in rare cases turning into cirrhosis. Changes in the lungs in 25% of children are characterized by the development of pneumosclerosis and fibrosis.
If primary CMV infection is detected during the first two trimesters of pregnancy, in some cases the question of terminating the pregnancy may arise, since predicting the likely outcome of a pregnancy complicated by the virus is not an easy task. CMV differs from other TORCH infections in that fetal lesions caused by the infection can occur during all three trimesters.
Specific diagnostics
The main direction in the prevention of CMV is compliance with the rules of personal hygiene, individual protection when in contact with patients with cytomegalovirus. It is especially important to follow preventive recommendations for people at risk:
- Patients who have undergone transplantation.
- Pregnant women.
- HIV-infected.
- Patients suffering from immunodeficiencies.
Means for specific prevention are under development. The only drug that allows prophylaxis in patients after transplantation is letermovir. It has not yet found widespread use; it is recommended for use only in the USA.
How to treat cytomegalovirus in children
With active CMV infection, a special daily regimen and adherence to a certain diet recommended by the doctor are indicated. Comprehensive drug treatment and the use of antiviral drugs that fight the virus and prevent the development of complications are also necessary. One of these drugs, which is approved for the treatment of children from the first days of life, is the antiviral drug VIFERON, which is used for CMV infection and related diseases. Antiviral properties allow it to block the reproduction of the virus, and the immunomodulatory effect helps restore immunity. The drug was developed as a result of fundamental research in the field of immunology, which proved that in the presence of antioxidants (vitamins C, E and others), the antiviral effect of the main active ingredient, interferon, is enhanced.
Instructions for use for newborns and premature babies
Recommended dose of the drug VIFERON Suppositories for newborns, incl. premature babies with a gestational age of more than 34 weeks - the drug 150,000 IU daily, 1 suppository 2 times a day after 12 hours. The course of treatment is 5 days.
Premature newborns with a gestational age of less than 34 weeks are prescribed VIFERON 150,000 IU daily, 1 suppository 3 times a day every 8 hours. The course of treatment is 5 days.
The recommended number of courses for the treatment of cytomegalovirus in children is 2-3 courses. The break between courses is 5 days. According to clinical indications, therapy can be continued.
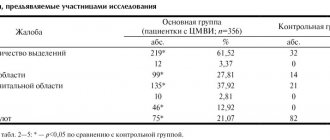
Thus, according to studies published in the article “Efficacy of treatment with recombinant interferon-α2b (Viferon®) in premature newborns with severe intrauterine infections,” the drug VIFERON, when administered rectally, has a positive effect on the clinical manifestations and outcome of the disease, as evidenced by a statistically significant reduction in mortality (3.7 times) of premature children with IUI (intrauterine infections) compared to the group of children who received basic standard treatment without the drug VIFERON1.
Instructions for use for pregnant women
VIFERON is also used to treat cytomegalovirus in pregnant women. Thus, according to research, the use of the drug to reduce the development of pathological conditions in a child helps reduce the development of severe forms of intrauterine infections (IUI) by 1.7 times, and moderate forms of IUI by 1.9 times; reducing the number of children with intrauterine growth retardation by 1.7 times; reducing cases of asphyxia by 1.9 times; reducing the number of newborns with central nervous system damage by 2.3 times; optimal functional maturation of the child’s immune system due to antigenic stimulation of the fetal immune system.2
One of the main advantages of suppositories in the treatment of pregnant women and newborns is their gentle effect on the body. When using the drug in the form of suppositories, the liver and stomach do not experience additional stress. Candles (suppositories) do not contain dyes and sweeteners, like syrups and other oral medications. Consequently, their use minimizes the risk of allergic reactions.
Reference and information material
Author of the article
Gerasimenko Igor Olegovich
General doctor
- A.A. Kushch, M.V. Degtyareva, V.V. Malinovskaya, I.G. Soldatova, R.R. Klimova, A.A. Adieva, V.V. Serova, E.G. Getia, A.A. Tsibizov, Z.S. Gadzhieva. “The effectiveness of treatment with recombinant interferon-α2b (Viferon®) in premature newborns with severe intrauterine infections,” Children's infections 2009.
- Bocharova I.I., Malinovskaya V.V., Aksenov A.N., Bashakin N.F., Guseva T.S., Parshina O.V. “The influence of viferon therapy in mothers as part of the treatment of urogenital infections during pregnancy on the immunity parameters and health status of their newborns,” 2009.
List of materials used
- https://cyberleninka.ru/article/n/tsitomegalovirusnaya-infektsiya-u-detey
- [ii] https://www.medlinks.ru/article.php?sid=53773
- [iii] https://www.nrcii.ru/patsientam/zabolevaniya/tsitomegalovirus.php
- [iv] https://www.lvrach.ru/2018/04/15436945/
- [v] https://cyberleninka.ru/article/n/effektivnost-lecheniya-rekombinantnym-interferonom-2-viferonom-u-nedonoshennyh-detey-s-tyazhelymi-vnutriutrobnymi-infektsiyami
- [vi] https://www.fesmu.ru/elib/Article.aspx?id=210455
Loading...
Take other surveys
Treatment
Drug therapy is used when a child is infected as a newborn or in severe cases of the disease. Treatment is not aimed at completely getting rid of the virus, which is physically impossible, but at reducing its activity. Antiherpetic drugs are most often used for treatment. To draw up a treatment plan, contact your pediatrician.
Sources:
- A.I. Smirnova, E.V. Rossikhina, N.S. Dupin. The role of cytomegaloviruses in obstetric pathology and neonatology // Vyatka Medical Bulletin, 2010.
- R.Zh. Seisebaeva, A.E. Almaganbetova, F.N. Kasymbekova, E.S. Ataibekova, G.M. Abdrakhmanova. Epidemiology of congenital cytomegalovirus infection // Bulletin of KazNMU, 2021, No. 1
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.