Leukopenia is a pathological condition that is characterized by a decrease in leukocytes in the blood (less than 4 x 109/l), including all cells of the leukocyte formula (neutrophils, monocytes, lymphocytes, basophils). Such changes may be reactive, or may be indicators of a malfunction of the bone marrow, which produces white blood cells.
This condition is caused by massive destruction of young blood cells and a decrease in the formation of mature leukocytes, which are the basis for the proper functioning of the immune system.
| Leukocytes are protective blood cells that are an integral part of the immune system. They “destroy” foreign elements, produce biologically active substances, and take part in inflammatory processes. · Therefore, an imbalance of leukocytes leads to a decrease in the body’s defenses, thereby increasing its vulnerability to various types of infections. The severity of the pathological process depends on the rate of reduction of leukocytes in the blood. |
In some clinically healthy people, leukopenia is considered normal.
However, in most cases, a decrease in leukocytes is a pathological condition that develops against the background of primary or secondary causes.
By origin they are:
- Endogenous (hormonal imbalance, inflammatory process in the body, genetic predisposition).
- Exogenous (bacteria, viruses, fungi, parasites).
Infectious and non-infectious.
Causes of the disease
The causes of leukopenia may be due to:
Diseases of blood cells (bone marrow)
- Myelofibrosis;
- Aplastic anemia;
- Enlarged spleen;
- Myelodysplastic syndrome.
Congenital pathologies
- Kostman's syndrome;
- Myelocathexis;
- Kidney failure;
- Itsenko-Cushing syndrome;
- Gensler's syndrome.
Infectious diseases
- ARVI;
- Hepatitis;
- Rubella;
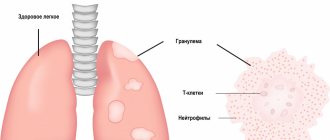
- Tuberculosis;
- HIV.
Purulent pathologies
- Endometritis;
- Cholangitis;
- Sepsis;
- Lung abscess.
Autoimmune disorders
- Allergy;
- Lupus erythematosus;
- Rheumatoid arthritis;
- Thyroiditis;
- Sarcoidosis.
Deficiency of the vitamin-mineral complex
- B vitamins (especially B2, B6, B9 and B12);
- Copper;
- Zinc.
Taking medications
- Cyclosporine;
- Interferon;
- Minocycline;
- Penicillin.
Oncological pathologies and methods of their treatment
- Blood cancer;
- Chemotherapy;
- Radiation therapy;
- Bone marrow transplantation.
Redistribution of leukocytes
- Shock conditions;
- Hard physical labor.
During the process of redistribution, leukocytes temporarily “leave” the bloodstream, switching to the kidneys, lungs, and capillaries.
Prolonged contact with chemicals, radiation, viral infections, hereditary factors can also negatively affect the level of leukocytes in the blood.
Leukopenia in children usually manifests itself against the background of viral infections (acute respiratory infections, influenza, measles, chicken pox), taking certain medications (interferon, antibiotics, antihistamines) or a poor diet (lack of protein, folic acid, zinc).
At the same time, a critical decrease in leukocytes (below 1.5x 109/l) is a reason for an urgent and comprehensive examination.
According to the severity of leukopenia, they are distinguished:
- Mild degree - 1.5x 109/l;
- Leukopenia 2 degrees - 0.5-1 x 109/l;
- Severe leukopenia (agranulocytosis) – less than 0.5x 109/l.
Acute agranulocytosis in children usually indicates a dangerous change in the functioning of the bone marrow.
The World Health Organization adopted the 10th revision of the International Classification of Diseases (ICD) as a single regulatory document, according to which leukopenia was assigned code D72.8.0.
Classification
As already mentioned, one type of syndrome is physiological. It occurs quite rarely, in approximately no more than 10 percent of people.
These people do not experience any inconvenience, their immunity is not reduced, and there are no health complaints.
But if the syndrome arose due to any disease, it is already a pathological syndrome.
In a small proportion of the population, the syndrome is hereditary rather than acquired.
In rare cases, an insufficient number of white blood cells is the result of their movement into the vessels. In this case, redistribution syndrome is diagnosed. When the number of leukocytes decreases throughout the bloodstream, a true syndrome is diagnosed.
Neutropenia is the most common type of syndrome. There are several stages:
- Light stage: from 1000 to 1500 neutrophils (one of the types of leukocytes) in 1 μl of blood;
- Moderate stage: from 500 to 1000 in 1 µl;
- Severe stage: less than 500 µl in 1 ml.
The syndrome can be acute or chronic. Acute lasts from several hours to several days. The syndrome is chronic and can last up to several years.
Symptoms
Leukopenia, as a rule, is determined accidentally during a preventive study, since it does not have specific clinical symptoms.
The first signs of a decrease in leukocytes may appear when bacterial, viral or infectious complications are involved in the pathological process.
What this entails:
- Increased body temperature;
- The appearance of aphthae on the mucous membranes of the mouth;
- Increased gum bleeding;
- Pustular infections;
- Tachycardia;
- Headache;
- Anxiety;
- Pain in the left hypochondrium (associated with an enlarged spleen).
All symptoms of leukopenia must be carefully examined, so in this case, consultation with a doctor is mandatory.
Leukopenia: causes, symptoms, diagnosis, treatment
Oncological hospital in Moscow / Leukopenia
Cancer treatment at the Moscow Oncology Hospital
Leukocytes is the general name for a group of blood cells that includes lymphocytes, monocytes, eosinophils, neutrophils and basophils. They are different in structure and function, but they also have something in common - they all participate in the body’s immune defense against external and internal foreign agents.
Normally, the number of leukocytes ranges from 4.5 to 10 thousand cells per microliter (µl) of blood. Leukopenia is a decrease in the number of leukocytes per unit volume.
Degrees of leukopenia
Depending on the number of leukocytes in a certain volume of blood, several degrees of leukopenia are distinguished, each of which requires special tactics. It is clear that the higher the degree of leukopenia, the more the protective function suffers, and the more vulnerable the body is to infections.
- I Art. – reduction in the number of leukocytes to no more than 3 thousand cells/μl;
- II Art. – decrease in the number of leukocytes from 2 to 2.9 thousand cells/μl;
- III Art. – the leukocyte count drops to 1-1.9 thousand cells. /µl;
- IV Art. – the number of leukocytes is less than 1 thousand cells/μl.
Leukopenia can be acute when it lasts no more than 3 months, and chronic when it lasts longer than this period. The duration of its existence is of great clinical importance. For example, even critical leukopenia of 0.1 thousand cells/µl is complicated by an infectious process in only one patient out of four, if it lasts no more than a week; if it persists for one and a half months, infectious complications occur in 100%.
Causes of leukopenia
Cancer patients often suffer from leukopenia. Sometimes this is due to primary damage to the bone marrow due to tumors of the blood system. Sometimes metastases of other tumors develop in it.
All this suppresses the normal process of white blood cell production, and bone marrow cells are replaced by tumor cells. At the same time, the formation of other blood cells - red blood cells and platelets - also suffers. Therefore, patients suffer not only from leukopenia, but also from anemia and increased bleeding.
The influence of chemotherapy and radiotherapy is the most common and significant cause of leukopenia in cancer patients. Rapidly dividing bone marrow cells are extremely sensitive to the effects of radio rays and toxic chemotherapy drugs. In this case, all hematopoietic germs in the bone marrow are also affected, reaching their greatest severity by the first or second weeks from the start of treatment.
Symptoms of leukopenia
Minor leukopenia can only be detected by a clinical blood test. More pronounced symptoms have external manifestations, some of which are caused by concomitant anemia and thrombocytopenia. Patients note:
- increased body temperature;
- general weakness;
- dizziness;
- feeling of lack of air;
- pain in bones and joints;
- stomach ache.
Infectious complications are common in patients with severe leukopenia. First of all, the mucous membrane of the mouth and oropharynx, which is initially abundantly populated with bacterial flora, is affected. It begins to actively manifest itself as immunity declines. Ulcerative necrotic stomatitis develops.
Cystitis is not uncommon; a specific manifestation of leukopenia in women is increased, lengthened and irregular menstrual bleeding.
Severe intestinal damage may develop - necrotizing enteropathy.
Sepsis - generalized inflammation provoked by a local focus of infection - is the most dangerous complication of leukopenia with a high percentage of deaths.
Treatment of leukopenia
Mild leukopenia does not require drug treatment, but infection prevention measures are increased. Patients are especially careful about hygiene, including oral hygiene, avoid crowds of people, eat only thermally processed food, and douse vegetables and fruits with boiling water after washing.
Leukopenia of a more pronounced degree requires isolation of the patient in a sterile box, where personnel communicate with him, observing all the rules of asepsis and antiseptics. Such patients may be prescribed:
- hormonal drugs;
- colony-stimulating factors;
- agents that improve cellular metabolism and accelerate cell regeneration;
- antibiotics for prophylactic purposes.
Prevention of leukopenia in the European clinic
At the European Clinic, the cellular composition of the blood is always carefully monitored, including the number of leukocytes. These indicators are monitored with redoubled attention when prescribing chemotherapy and radiation therapy.
Following the standards in the mode of their use, as well as preventing negative effects with the help of accompanying therapy, allows us to minimize their damaging effect on blood cells.
If leukopenia develops, an experienced oncologist-hematologist working in the clinic takes part in treatment.
Contact us
How to treat leukopenia
Before starting treatment for leukopenia, it is necessary to conduct a comprehensive medical diagnosis, determine the type of leukopenia (neutropenia, lymphopenia, eosinopenia, monocytopenia, agranulocytosis) and the cause of its occurrence. Since any therapeutic effect should always be aimed at eliminating the root cause of a particular disorder.
| For the most accurate and reliable result, it is recommended to undergo a repeat blood test after some time. |
Moreover, not every decrease in leukocytes requires therapeutic intervention; it all depends on the volume and severity of the pathological process.
The Spizhenko Clinic conducts:
- Determining the cause of leukopenia and therapeutic correction if necessary.
- Bone marrow transplantation.
In case of severe oncological processes of the blood system, stem cell transplantation is performed.
- Splenectomy.
In the absence of a positive result in the treatment of autoimmune leukopenia.
Why does the syndrome appear in a cancer patient?
The causes of the syndrome in cancer are various. Here are some of them:
- Metastasis of atypical cells to the bone marrow. In this case, cancer cells displace healthy tissue. As a result, the process of formation of blood cells is disrupted.
- Autoimmunity. The immune system acts on its own leukocytes, and they are rapidly destroyed
- Cytostatic effect. The target of chemotherapy drugs is not only atypical cells, but also some healthy tissues.
- Consequences of radiation therapy.
The danger of the syndrome is that a reduction in the number of leukocytes reduces the body’s defenses and increases its susceptibility to various types of infectious invasions.
Leukopenia and agranulocytosis
The proportion of leukopenic conditions among other diseases of the blood system is quite large. Statistical data indicate an increase in the number of patients with severe leukopenia in recent years. Often the development of this pathology is in some connection with the use of new bacteriostatic agents in medical practice, with exposure to ionizing radiation, as well as with an increase in episodes of allergic diseases. In assessing leukopenic conditions, the doctor should avoid two opposing trends: in some cases, there is no due attention to leukopenia, which is the beginning of a severe pathology of the blood system, and the necessary preventive and therapeutic measures are not taken; in others, any decrease in the number of leukocytes is regarded as a symptom of a severe pathology with unfounded the use of potent leukopoietic drugs (drugs that enhance the intensity of the formation of these blood cells). Therefore, to correctly assess the significance of “individual” leukopenia, it is necessary, if possible, to find out its causes and mechanism of development, since only such a solution to the issue ensures the success of treatment and preventive measures in each individual case. Leukopenias are often combined with a significant decrease in the number of neutrophils in the peripheral blood, therefore, in essence they are neutropenia or granulocytopenia (respectively, a decrease in the number of neutrophils and granulocytes).
The causes of granulocytopenia, with all their diversity, are divided into exogenous (acting from the outside), endogenous (arising in the body itself) and hereditary. The first group of factors includes some substances that have a toxic effect, such as benzene, toluene, arsenic, mercury; some medications; radiation; infectious diseases.
Endogenous causes of neutropenia may be a violation of the endocrine regulation of granulocytopoiesis, i.e., the formation of granulocytes (thyrotoxicosis, adrenal insufficiency, dysfunction of the pituitary gland), increased spleen function, allergic conditions.
The listed leukopenias are classified as functional. But leukopenia and neutropenia can be a manifestation of a violation of bone marrow hematopoiesis in systemic blood pathologies: acute leukemia, hypo- and aplastic conditions. In some cases, it is not possible to identify the causative factor leading to the development of granulocytopenia. Recently, there are fewer and fewer such forms.
In recent years, a special group of hereditary neutropenias (constant and periodic neutropenias) has been identified. In addition, leukopenia can be symptomatic in the form of an unstable hematological sign in some diseases.
Moderate asymptomatic leukopenia without any clinical manifestations are discovered by chance and are one of the secondary and optional symptoms of various diseases. They are characterized by a moderate decrease in the number of leukocytes (up to 3.0-4.0 H 109/l) and mild granulocytopenia (40-60% of the total number of neutrophils). The functional properties of leukocytes are not changed. Myelopoiesis is not impaired. Bone marrow is normal. There are also no changes in the formation of red blood cells and platelets. Such leuko- and neutropenia are most often purely symptomatic, accompanying a number of diseases not related to the blood system (thyrotoxicosis, gastritis, enterocolitis, cholecystitis, and many others).