Women's breasts are susceptible to particularly dangerous diseases. Therefore, every girl should be clearly aware that regular testing, ultrasound and other diagnostic measures can identify many diseases in the early stages. But let’s look in more detail at what mastopathy is and how this pathology manifests itself.
Diffuse mastopathy is accompanied by structural changes in the tissues of the mammary gland. The disease develops for various reasons and can develop into breast cancer.
Diffuse mastopathy of the mammary glands is a pathology in which connective tissue grows in the mammary gland. Initially, this process is benign, but in the absence of adequate timely treatment, it can transform into a malignant tumor.
Changes usually affect the entire breast, rather than individual parts. Other pathological names: mammary dysplasia, diffuse fibroadenomatosis, dyshormonal hyperplasia.
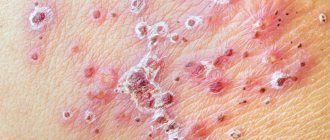
Connective elements replace epithelial tissue and grow in the chest in the form of unformed granular threads and nodules. As a result, the structure of the lobules and ducts of the gland is disrupted, the compaction increases in size, and the diffuse form of mastopathy can turn into nodular.
Diffuse mastopathy of the mammary glands is observed in 75% of women with severe symptoms and in 55-65% of women with asymptomatic disease. The age group where diffuse fibrous mastopathy of the mammary gland or diffuse cystic mastopathy of the mammary glands is most often observed is from 30 to 50 years. But in medical practice, cases have also been identified under the age of 30 years and over 50 years, although with menopause the possibility of this condition occurring sharply decreases.
Classification of the disease
Depending on the nature of changes in breast tissue, the following types of dyshormonal hyperplasia are distinguished:
- diffuse (multiple compactions predominate);
- fibrocystic (characterized by the formation of cysts and fibroadenomas);
- focal mastopathy (single nodes).
The sclerosing type of mastopathy deserves special attention - the most oncological form with the deposition of calcium salts (calcified) in the tissues.
Diffuse fibrous mastopathy of the mammary glands is most often detected in young patients during puberty; it is of a benign nature, characterized by the presence in the tissue of the mammary glands of nodules consisting of cysts of various sizes. Usually everything affects both breasts, and upon palpation the nodes can be easily felt. The cystic form is common among women during menopause.
According to the degree of tissue change, breast dysplasia can be: mild, moderate or severe.
Diagnostic methods for determining diffuse mastopathy:
- examination of the mammary glands and their palpation, identification of painful sensitive areas without clear boundaries;
- mammography: determines the form of the disease and the presence or absence of malignant elements;
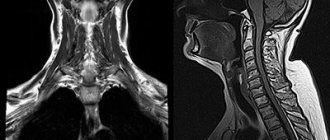
- ultrasound - shows an increase in glandular tissue, fibrous changes in the structure of the lobar septa and duct walls;
- ductography – reveals deformation of the milk ducts;
- analysis of a nipple smear is necessary to exclude pathologies similar in characteristics to mammary dysplasia (actinomycosis, syphilis or mammary tuberculosis).
Further diagnosis of diffuse mastopathy includes analysis of sex and thyroid hormones, biopsy and magnetic resonance imaging of the mammary glands, blood tests for tumor markers, and ultrasound of the pelvic organs.
Treatment of diffuse fibrocystic mastopathy
Fibrocystic mastopathy (FCM), a benign lesion of the mammary gland, is characterized by a spectrum of proliferative and regressive tissue changes with a violation of the ratio of epithelial and connective tissue components. In recent years, there has been a steady increase in this pathology throughout the world (A. G. Egorova, 1998; V. I. Kulakov et al., 2003). Mastopathy occurs in 30–70% of women of reproductive age; with gynecological diseases, its frequency increases to 70–98% (A. V. Antonova et al., 1996).
In premenopausal women it occurs in 20% of women. After menopause, new cysts and nodes, as a rule, do not appear, which proves the participation of ovarian hormones in the occurrence of the disease.
It is currently known that malignant diseases of the mammary glands occur 3–5 times more often against the background of benign neoplasms of the mammary glands and in 30% of cases with nodular forms of mastopathy with proliferation phenomena. Therefore, in the anticancer fight, along with early diagnosis of malignant tumors, timely detection and treatment of precancerous diseases is no less important.
There are non-proliferative and proliferative forms of FCM. At the same time, the risk of malignancy in the non-proliferative form is 0.86%, with moderate proliferation - 2.34%, with pronounced proliferation - 31.4% (S. S. Chistyakov et al., 2003).
The main role in the occurrence of FCM is assigned to dishormonal disorders in a woman’s body. It is known that the development of the mammary glands, regular cyclical changes in them at puberty, as well as changes in their function during pregnancy and lactation occur under the influence of a whole complex of hormones: gonadotropin-releasing hormone (GnRH) of the hypothalamus, gonadotropins (luteinizing and follicle-stimulating hormones), prolactin, human chorionic gonadotropin, thyroid-stimulating hormone, androgens, corticosteroids, insulin, estrogens and progesterone. Any imbalance of hormones is accompanied by dysplastic changes in mammary gland tissue. The etiology and pathogenesis of FCM have not yet been definitively established, although more than a hundred years have passed since the description of this symptom complex. An important role in the pathogenesis of FCM is played by relative or absolute hyperestrogenism and progesterone deficiency. Estrogens cause proliferation of the ductal alveolar epithelium and stroma, and progesterone counteracts these processes, ensures differentiation of the epithelium and cessation of mitotic activity. Progesterone has the ability to reduce the expression of estrogen receptors and reduce the local level of active estrogens, thereby limiting the stimulation of breast tissue proliferation.
Hormonal imbalance in breast tissue towards progesterone deficiency is accompanied by edema and hypertrophy of intralobular connective tissue, and proliferation of ductal epithelium leads to the formation of cysts.
In the development of FCM, an important role is played by the level of prolactin in the blood, which has a diverse effect on the tissue of the mammary glands, stimulating metabolic processes in the epithelium of the mammary glands throughout a woman’s life. Hyperprolactinemia outside of pregnancy is accompanied by swelling, engorgement, pain and swelling in the mammary glands, more pronounced in the second phase of the menstrual cycle.
The most common causes of mastopathy are hypothalamic-pituitary diseases, thyroid dysfunction, obesity, hyperprolactinemia, diabetes mellitus, lipid metabolism disorders, etc.
The cause of dyshormonal disorders of the mammary glands can be gynecological diseases; sexual disorders, hereditary predisposition, pathological processes in the liver and biliary tract, pregnancy and childbirth, stressful situations. FCM often develops during menarche or menopause. In adolescence and young women, the diffuse type of mastopathy with minor clinical manifestations, characterized by moderate pain in the upper outer quadrant of the mammary gland, is most often detected.
At 30–40 years of age, multiple small cysts with a predominance of the glandular component are most often detected; the pain syndrome is usually severe. Single large cysts are most typical for patients aged 35 years and older (A. L. Tikhomirov, D. M. Lubnin, 2003).
FCMs also occur in women with a regular two-phase menstrual cycle (L. M. Burdina, N. T. Naumkina, 2000).
Diffuse FCM can be:
- with a predominance of the ferrous component;
- with a predominance of the fibrous component;
- with a predominance of the cystic component.
Diagnosis of breast diseases is based on examination of the mammary glands, palpation, mammography, ultrasound, puncture of nodules, suspicious areas and cytological examination of punctate.
Examination of the mammary glands of reproductive age must be carried out in the first phase of the menstrual cycle (2–3 days after the end of menstruation), since in the second phase, due to engorgement of the glands, there is a high probability of diagnostic errors (S. S. Chistyakov et al., 2003) .
When examining the mammary glands, the appearance of the glands is assessed, paying attention to all manifestations of asymmetry (contours, skin color, position of the nipples). Then the examination is repeated with the patient's hands raised. After the examination, the mammary glands are palpated, first with the patient standing and then lying on her back. At the same time, the axillary, subclavian and supraclavicular lymph nodes are palpated. If any changes are detected in the mammary glands, mammography and ultrasound are performed.
Ultrasound of the mammary glands is becoming increasingly popular. This method is harmless, which allows the study to be repeated many times if necessary. In terms of information content, it is superior to mammography in the study of dense mammary glands in young women, as well as in identifying cysts, including small ones (up to 2-3 mm in diameter), while without additional interventions it makes it possible to judge the condition of the epithelium lining the cyst and carry out differential diagnosis between cysts and fibroadenomas. In addition, when examining lymph nodes and mammary glands with diffuse changes, ultrasound is the leading one. At the same time, with fatty involution of mammary gland tissue, ultrasound is significantly inferior in information content to mammography.
Mammography - radiography of the mammary glands without the use of contrast agents, performed in two projections - is currently the most common method of instrumental examination of the mammary glands. Its reliability is very high. So, for breast cancer it reaches 95%, and this method allows you to diagnose non-palpable (less than 1 cm in diameter) tumors. However, this method is limited in application. Thus, mammography is contraindicated for women under 35 years of age, during pregnancy and lactation. In addition, the information content of this method is insufficient when studying dense mammary glands in young women.
Despite the universally recognized connection between diseases of the mammary glands and genitals, Russia has not developed the concept of an integrated approach to the diagnosis and treatment of diseases of the mammary glands and organs of the reproductive system. A comparison of changes in the mammary glands with uterine fibroids and inflammatory diseases of the genitals showed that the frequency of pathological changes in the mammary glands with uterine fibroids reaches 90%, nodular forms of mastopathy more often occur when uterine fibroids are combined with adenomyosis (V. E. Radzinsky, I. M. Ordiyants, 2003). Based on these data and the fact that more than half of women with benign breast diseases suffer from uterine fibroids, adenomyosis and endometrial hyperplasia, the authors classify women with these diseases as a high-risk group for breast diseases.
In inflammatory diseases of the female genital organs, the frequency of benign diseases of the mammary glands was significantly lower - only in every fourth; nodular forms were not identified.
Consequently, inflammatory diseases of the genitals are not the cause of the development of FCM, but may be accompanied by hormonal disorders.
A mammological study of women of reproductive age with various gynecological diseases revealed a diffuse form of mastopathy in every third patient, and a third of women had a mixed form of FCM. The nodular form of mastopathy was determined in patients with a combination of uterine fibroids, genital endometriosis and endometrial hyperplasia.
Treatment of patients with nodular forms of benign diseases of the mammary glands begins with puncture with fine-needle aspiration. If cells with dysplasia in a nodular formation or cancer cells are detected during a cytological examination, surgical treatment is performed (sectoral resection, mastectomy) with urgent histological examination of the removed tissue.
Depending on the results of the examination, treatment of gynecological pathology, mastopathy, and correction of concomitant diseases is carried out.
Diet is important in the treatment and prevention of breast diseases: the nature of nutrition can affect the metabolism of steroids. An increased amount of fat and meat products is accompanied by a decrease in androgen levels and an increase in estrogen levels in the blood plasma. In addition, special importance is attached to a sufficient content of vitamins in the diet, as well as coarse fiber, since its anti-carcinogenic properties have been proven.
In recent years, the frequency of use of herbal medicines in the treatment of benign diseases of the mammary glands has increased.
V.I. Kulakov and co-authors (2003) used Wobenzym and herbal medicine when treating patients with various forms of mastopathy accompanied by mastalgia. The effectiveness of treatment of mastalgia after 3 months was 65%.
Many studies are devoted to the treatment of this pathology, but the problem remains relevant today (L. N. Sidorenko, 1991; T. T. Tagieva, 2000).
To treat mastopathy associated with mastalgia, various groups of drugs are used: analgesics, bromocriptine, night primrose oil, homeopathic drugs (mastodinone), vitamins, potassium iodide, oral contraceptives, herbal remedies, danazol, tamoxifen, as well as natural progesterone for transdermal use. The effectiveness of these remedies varies. Pathogenetically, the most substantiated method of treatment is the use of progesterone preparations.
Since the late 80s. last century, injectable (Depo-Provera) and implanted (Norplant) progestogens are widely used for therapeutic and contraceptive purposes (A. G. Khomasuridze, R. A. Manusharova, 1998; R. A. Manusharova et al., 1994). Long-acting injectable drugs include medroxyprogesterone acetate in the form of Depo-Provera and norethindrone enanthate. The mechanism of action of these drugs is similar to that of the progestin components of combined oral contraceptives. Depo-Provera is administered intramuscularly at 3-month intervals. The most common complications resulting from the use of Depo-Provera are prolonged amenorrhea and intermenstrual bleeding. Our research data showed that the drug does not have a negative effect on normal tissue of the mammary glands and uterus, while at the same time it has a therapeutic effect in hyperplastic processes in them (R. A. Manusharova et al., 1993). Long-acting drugs also include the implantable drug Norplant, which provides contraceptive and therapeutic effects for 5 years. For many years, it was believed that hormonal drugs should not be prescribed to patients with FCM from the time the disease is diagnosed until the indication for surgical treatment. At best, symptomatic therapy was carried out, consisting of prescribing a collection of herbs, iodine preparations, and vitamins.
In recent years, as a result of research, the need for active therapy, in which hormones play a leading role, has become obvious. With the accumulation of clinical experience in the use of Norplant, reports appeared about its positive effect on diffuse hyperplastic processes in the mammary glands, since under the influence of the gestagenic component in the hyperplastic epithelium, not only inhibition of proliferative activity consistently occurs, but also the development of decidual-like transformation of the epithelium, as well as atrophic changes in the epithelium of the glands and stroma. In this regard, the use of gestagens is effective in 70% of women with hyperplastic processes in the mammary glands. A study of the effect of Norplant (R. A. Manusharova et al., 2001) on the condition of the mammary glands in 37 women with a diffuse form of FCM showed a decrease or cessation of pain and tension in the mammary glands. During a control study after 1 year, ultrasound or mammography showed a decrease in the density of the glandular and fibrous components due to a decrease in areas of hyperplastic tissue, which was interpreted as regression of hyperplastic processes in the mammary glands. In 12 women, the condition of the mammary glands remained the same. Despite the disappearance of mastodynia, the structural tissue of the mammary glands did not undergo any changes. The most common side effect of Norplant, like Depo-Provera, is menstrual irregularity in the form of amenorrhea and intermenstrual bleeding. The use of oral gestagens for intermenstrual bleeding and combined contraceptives for amenorrhea (for 1 - 2 cycles) leads to the restoration of the menstrual cycle in the vast majority of patients.
Currently, oral (tablet) gestagens are also used to treat FCM. Among these drugs, duphaston and utrozhestan are the most widely used. Duphaston is an analogue of natural progesterone, completely devoid of androgenic and anabolic effects, safe for long-term use and has a progestogenic effect.
Utrozhestan is a natural micronized progesterone for oral and vaginal use. Unlike synthetic analogues, it has beneficial advantages, which consist primarily in the fact that the micronized progesterone included in its composition is completely identical to the natural one, which leads to an almost complete absence of side effects.
Micronized utrogestan is prescribed 100 mg 2 times a day, duphaston 10 mg 2 times a day. Treatment is carried out from the 14th day of the menstrual cycle for 14 days, 3–6 cycles.
Combined oral contraceptives are prescribed to block ovulation and eliminate cyclical fluctuations in the levels of sex hormones.
Danazol is prescribed 200 mg for 3 months.
GnRH agonists (diferelin, zoladex, buserelin) cause temporary reversible menopause. Treatment of mastopathy with GnRH agonists has been carried out since 1990.
The first course of treatment is usually prescribed for 3 months. Treatment with GnRH agonists inhibits ovulation and ovarian function, promotes the development of hypogonadotropic amenorrhea and the reversal of mastopathy symptoms.
For cyclic hyperprolactinemia, dopamine agonists (parlodel, dostinex) are prescribed. These drugs are prescribed in the second phase of the cycle (from the 14th to 16th day of the cycle) before the onset of menstruation.
In recent years, various herbal remedies that have anti-inflammatory analgesic and immunomodulatory effects have become widespread. The fees are prescribed in the second phase of the menstrual cycle and are used for a long time.
One of the most effective means of treating mastopathy is a combined homeopathic drug - mastodinone, which is a 15% alcohol solution with extracts of medicinal herbs cyclamen, chilibuja iris, tiger lily. The drug is available in bottles of 50 and 100 ml. Mastodinon is prescribed 30 drops 2 times a day (morning and evening) or 1 tablet 2 times a day for 3 months. Duration of treatment is not limited
Mastodinone, due to its dopaminergic effect, leads to a decrease in elevated levels of prolactin, which contributes to the narrowing of the ducts, a decrease in the activity of proliferative processes, and a decrease in the formation of the connective tissue component. The drug significantly reduces blood flow and swelling of the mammary glands, helps reduce pain, and reverse the development of changes in the tissue of the mammary glands.
In the treatment of diffuse forms of mastopathy, the drug Klamin, which is a plant adaptogen with antioxidant, immunocorrective, hepatoprotective activity, has an enterosorbent and mild laxative effect, has become widespread. One of the most important characteristics of Klamin is the presence of iodine in its composition (1 tablet contains 50 mcg of iodine), which in areas with iodine deficiency completely covers its deficiency.
The drug phytolon, which is an alcohol solution of the lipid fraction of brown algae, has a high antioxidant and immunostimulating effect. The active principle is copper derivatives of chlorophyll and trace elements. The drug is prescribed orally in the form of drops or externally. Together with a complex of herbs it has a good absorbing effect.
If there are concomitant diseases, it is necessary to treat them. When diffuse FCM is combined with uterine fibroids, endometrial hyperplasia, adenomyosis, it is necessary to additionally add pure gestagens (utrogestan, duphaston) to the therapy.
We observed 139 women who complained of aching pain, a feeling of fullness and heaviness in the mammary glands, intensifying in the premenstrual days, sometimes starting in the second half of the menstrual cycle. The age of the patients ranged from 18 to 44 years. All patients underwent examination and palpation of the mammary glands, and attention was paid to the condition of the skin, nipple, shape and size of the mammary glands, and the presence or absence of discharge from the nipples. In the presence of discharge from the nipples, a cytological examination of the discharge was performed.
All women underwent ultrasound of the mammary glands, and in the presence of nodes, ultrasound and non-contrast mammography; according to indications, a puncture of the formation was performed, followed by a cytological examination of the obtained material. Using ultrasound of the mammary glands, the diagnosis of the diffuse form of FCM was confirmed in 136 cases.
The menstrual cycle was disrupted by the type of oligomenorrhea in 84 women, 7 of the observed patients had polymenorrhea, and in 37 patients the cycle was apparently preserved, but functional diagnostic tests revealed anovulation. In 11 women, the menstrual cycle was not disrupted, but they had pronounced symptoms of premenstrual syndrome, which were observed in every menstrual cycle and affected the patient’s quality of life.
In 29 patients, mastopathy was combined with hyperplastic processes in the uterus (uterine fibroids, endometrial hyperplasia), in 17 - with adenomyosis, in 27 patients, along with mastopathy, there were inflammatory diseases of the genitals, in 9 women pathology of the thyroid gland was detected. Those examined often had extragenital pathology, and 11 close relatives had benign and malignant diseases of the genitals and mammary glands.
Based on the examination results, gynecological pathology, mastopathy and other concomitant diseases were treated. For the treatment of mastopathy in 89 patients, progestogel, gel, 1% - natural micronized local progesterone of plant origin was used. The drug was prescribed in a dose of 2.5 g of gel on the surface of each mammary gland 1-2 times a day, including during menstruation. The drug does not affect the level of progesterone in the blood plasma and has only a local effect. The use of progestogen was continued for 3 to 4 months. If necessary, patients were prescribed a course of maintenance therapy: vitamins E, B, C, A, PP. In addition, sedatives (tincture of valerian, lemon balm, motherwort) and adaptogens (Eleutherococcus, ginseng) were prescribed.
In 50 women, mastopathy was treated with mastodynon, which was prescribed 1 tablet 2 times a day in two courses, 3 months each, with an interval between courses of 1 month. The main active component of the drug Mastodinon is Agnus castus extract, which acts on dopamine D2 receptors of the hypothalamus and reduces the secretion of prolactin. A decrease in prolactin secretion leads to regression of pathological processes in the mammary glands and relieves pain. Cyclic secretion of gonadotropic hormones with normal prolactin levels restores the second phase of the menstrual cycle. At the same time, the imbalance between the levels of estradiol and progesterone is eliminated, which has a positive effect on the condition of the mammary glands.
Ultrasound was performed 6–12 months after the start of treatment. Positive dynamics were considered to be a decrease in the diameter of the ducts, the number and diameter of cysts, as well as their disappearance.
After the treatment (for 4–6 months), all 139 women showed positive dynamics within 1 month, which was expressed in a decrease and/or cessation of pain and a feeling of tension in the mammary glands.
During control ultrasound 6–12 months after the end of treatment, a decrease in the density of the glandular and fibrous components was noted due to a decrease in areas of hyperplastic tissue, which was interpreted as regression of the hyperplastic process in the mammary glands. In 19 women with a diffuse form of FCM and in 3 with fibroadenoma, an objective examination and ultrasound revealed no changes in the condition of the mammary glands, however, all patients noted an improvement in their condition (pain, a feeling of tension and fullness in the mammary glands disappeared).
Side effects when using the drugs Mastodinone and Progestogel were not noted in any observation.
The use of these drugs is pathogenetically justified.
There is no treatment algorithm for the treatment of mastopathy. Conservative treatment is indicated for all patients with a diffuse form of mastopathy.
R. A. Manusharova, Doctor of Medical Sciences, Professor
E. I. Cherkezova , Candidate of Medical Sciences
RMAPO, Andrology Clinic, Moscow
Occurrence and development of the disease
This disease is polyetiological, that is, it develops under the influence of a complex of factors. Among them are some diseases, genetic predisposition, lifestyle, reproductive characteristics of the body, and unfavorable environmental situation.
But the physiological cause of diffuse mastopathy always lies in a hormonal imbalance - an excess of estrogen and prolactin and a deficiency of progesterone.
The development of diffuse fibrocystic mastopathy of the mammary glands is influenced by hypothyroidism - insufficient production of hormones by the thyroid gland. Unfavorable factors include obesity, adrenal diseases, hepatitis, diabetes mellitus, cholecystitis.
Symptoms and signs of the disease
The main symptom is pain in the mammary glands (mastalgia), which occurs in the second half of the cycle. The pain is severe, tearing, sometimes aching and can spread to the armpits, shoulders, back, neck, and hypochondrium.
The breasts swell, its tissues evenly thicken, and upon palpation the woman can feel small granular formations. These signs of diffuse mastopathy decrease after the onset of menstruation and disappear in the first half of the cycle only in the early stages of the disease. In the last stages of mastalgia, these sensations are constantly present.
Hormonal imbalance (high levels of estrogen and prolactin and lack of progesterone) leads to the following symptoms:
- delayed menstruation;
- menstruation is painful or completely absent;
- severe symptoms of premenstrual syndrome (drowsiness, irritability, tearfulness);
- brittle and dull hair, dry skin.
Less commonly, with mastopathy, when the nipples are pressed, a whitish, gray-greenish liquid or mixed with blood is released.
Risk factors
Reproductive risk factors include:
- absence of pregnancy and childbirth, infertility;
- abortion;
- late first birth (after 30-35 years);
- refusal to breastfeed or short duration of breastfeeding;
- early onset of menstruation (before 12 years);
- pathology of the genital organs (ovarian dysfunction, adnexitis, oophoritis, etc.).
The risk increases with alcohol abuse and smoking, the habit of sunbathing topless in solariums and in the sun, as well as with chronic stress, poor diet, and lack of regular sex life.
Symptoms of mastopathy
For mastopathy, the most typical complaints are:
- breast tenderness,
- a feeling of increasing their volume,
- engorgement and swelling of the glands,
- the presence of clear or colostrum-like fluid discharge from the nipples of the mammary glands.
Pain may radiate to the armpits, shoulder and shoulder blade. The most common is a combination of symptoms of mastopathy and premenstrual syndrome. The main complaints in these conditions are: headache (often migraine-type), swelling of the face and limbs, nausea, less often vomiting, impaired bowel function, flatulence. With the neuropsychic form of premenstrual syndrome, complaints such as irritability, depression, weakness, tearfulness and aggressiveness may be associated. Difficulties in determining the cause of pain are due to the fact that pain can occur not only with pathology of the mammary gland, but also with cervicothoracic osteochondrosis, radiculoneuritis, intercostal neuralgia and is eliminated with appropriate therapy.
Treatment of the disease
Drug therapy is selected by the attending physician depending on the form and stage of mastopathy:
- antiestrogens;
- competent selection of oral contraceptives;
- gestagens also have an antiestrogenic effect;
- thyroid hormones;
- diuretics;
- NVPS for pain and swelling;
- sedative;
- vitamins, food additives, potassium iodide;
- phytotherapy;
- homeopathy to reduce prolactin;
- adaptogens;
- ointments and creams are prescribed for topical use.
Treatment of diffuse mastopathy involves a diet with a predominance of vegetables, fruits, herbs, dairy products, sources of iodine (seaweed, cod liver, plums).
Nuts, fish, legumes are useful. It is not allowed to include smoked foods, coffee, cocoa, tea, chocolate, animal fats, flour products, marinades and salty foods in the daily diet.
The effectiveness of therapy is increased by physical activity and physiotherapy (electrophoresis, mud therapy, galvanization, therapeutic baths). Thermal effects - sauna, steam bath, hot compresses on the chest and wraps, as well as solarium or sunbathing are prohibited.
If any symptoms indicating diffuse mastopathy are detected, you should immediately visit an oncologist-mammologist for a comprehensive diagnosis and prescribe a treatment regimen. You can make an appointment with a doctor either by calling +7 (495) 995-00-34 or by writing in the feedback form on our website.
How to prevent disease
To prevent widespread breast mastopathy, it is important:
- lead a healthy lifestyle;
- have a regular sex life;
- eliminate stressful situations;
- promptly treat gynecological and hormonal diseases;
- use modern contraception;
- Wear comfortable underwear that does not compress your breasts.
Self-examination and visits to a mammologist, carried out regularly, at least once a year, will help to detect the disease in time.
You can make a diagnosis and undergo a consultation with an experienced specialist in our clinic. The medical center is located at: Moscow, 2nd Tverskoy-Yamskaya lane, 10.
Breast tumor
Facts of the degeneration of a benign tumor into cancer are described only for atypical ductal hyperplasia and for benign processes with proliferation and dysplasia. All of these conditions cannot be determined by examination, ultrasound, mammography or other non-invasive tests. They can only be detected by a biopsy and examination under a microscope of the formation that was found using the above non-invasive diagnostic methods.
Even the detection of atypical hyperplasia, dysplasia or proliferation does not guarantee the development of breast cancer: these conditions only increase the risks by a maximum of 4 times. In most women, these conditions never develop into cancer.
Not every tumor found in the breast is necessarily malignant or will become so!