Detailed description of the study
The purpose of diagnosis is to identify pathogens in a stool sample submitted for research. The required amount of material is distributed over a selective—pathogen-specific—nutrient medium, after which the sample is placed in a thermostat. To successfully isolate a pure culture, a number of requirements must be met: maintain a certain level of humidity, ambient temperature, and oxygen concentration. After a few days, the results are assessed. This method is called bacteriological, its implementation period is from 7 to 10 days.
Listeria (Listeria monocytogenes) is a rod-shaped bacterium with rounded ends, the length of which does not exceed two micrometers, and is an intracellular parasite. It differs in that it is able to maintain viability in a wide temperature range (from +3-4 to 40 or more degrees Celsius). Moreover, even in conditions of negative temperatures it does not always die. Sensitive to the acidity and humidity of the environment, the presence of organic compounds in it. The concentration of microorganisms naturally increases in the spring and summer, and decreases in winter.
Listeria causes the infectious disease "listeriosis", which belongs to typical sapronoses, when pathogens are localized and multiply in inanimate objects of nature: soil, leaf lining, etc.
Pathogenic microorganisms enter the human body by consuming contaminated water, vegetables, fruits and berries that have not been sufficiently purified. Less commonly - through the mucous membranes of the eyes, respiratory and genital tracts, through the skin (if its integrity is violated). Transplacental transmission is possible (from an infected mother to the fetus). It is an opportunistic infection, that is, the full clinical picture “unfolds” only in people with reduced immunity. The pathogenicity of the bacteria is not so high as to provoke the development of the disease in individuals with a normal immune system.
After penetration into the body, they spread through the blood and lymphatic vessels to the organs with the most active lymph and blood supply. They damage the liver, kidneys, structures of the central nervous system, spleen, and are concentrated in the lymph nodes. The incubation period varies significantly in duration: from several weeks to one and a half to two months. The infection occurs acutely - up to 3 months, subacutely or chronically (more than six months).
Manifestations of the disease depend on the initial state of the body and the organs in which the pathological process is localized. Among others, the following signs of listeriosis may be observed:
- Conjunctivitis, pain and pain in the eyes, purulent discharge;
- Ulcerative skin defects;
- Rash of various localizations, accompanied by intense itching, increased skin sensitivity;
- Enlarged and painful lymph nodes;
- Aches in muscles, bones, joints;
- Increased body temperature, in severe cases - up to 38-39 ° C;
- Pain when swallowing;
- Dyspeptic disorders (nausea, repeated episodes of vomiting), cramping dull pain in the abdominal area;
- Itching and discharge from the genital tract;
- Cough, shortness of breath, chest discomfort;
- Urinary disorders, pain in the lumbar region;
- General symptoms of intoxication (drowsiness, headache, loss of appetite).
At-risk groups:
- Pregnant women: more than 25% of the total number of confirmed diagnoses;
- Newborns: the disease is characterized by a severe course and a high mortality rate, in approximately 2 cases out of 10, and when infected during childbirth - up to 50%;
- Weakened patients;
- Elderly persons;
- People with concomitant diseases accompanied by suppression of the activity of the immune system, for example, with acquired immunodeficiency syndrome - AIDS;
- Livestock production workers.
The variety of clinical manifestations of listeriosis significantly complicates its timely detection. Despite the fact that a wide range of laboratory and instrumental diagnostic methods are currently used - from smear microscopy to molecular genetic analysis with the identification of specific antigens and antibodies - the “gold standard” remains bacteriological culture of biomaterial.
Listeria monocytogenes
Listeria monocytogenes
- a type of gram-positive bacteria, the causative agent of a deadly human disease - listeriosis.
Facultative anaerobe. Listeria monocytogenes
can grow and multiply inside host cells.
The bacteria look like short rods with rounded ends, have a diameter of approximately 0.4-0.5 microns and a length of about 0.5-2 microns. Does not form a dispute. Listeria monocytogenes
is highly resistant in the external environment, growing in a wide temperature range, from +1 to +45°C and in high salt concentrations.
Listeria monocytogenes
can grow in refrigerated foods or remain viable in brine. At 70°C they die after half an hour, and at 100°C - after 3–5 minutes.
Listeria monocytogenes is the causative agent of listeriosis.
Listeriosis is not a widespread infection. In terms of the number of identified cases, it is significantly inferior to salmonellosis and campylobacteriosis, but exceeds them in mortality and severity of the clinical course. Listeriosis is typically caused by eating food contaminated with Listeria monocytogenes
.
It is an important public health problem. According to official statistics, approximately 1,600 cases of listeriosis are detected in the United States per year, 260 of which are fatal. Listeria monocytogenes
most often affects older people, pregnant women, newborns, and adults with weakened immune systems. However, listeriosis can also affect people outside these risk groups.
Human infection with listeria occurs as a result of*:
- consumption of infected products of animal origin (dairy products, meat products, poultry products), vegetables and fruits, seafood eaten raw or thermally insufficiently processed
- inhalation of dust contaminated with listeria
- contact with sick or listeria-carrying animals
- intrauterine transmission of the pathogen through the placenta or through contact of a newborn with the birth canal of a postpartum mother
- contact of newborn children with infected care items and medical instruments in maternity hospitals.
Symptoms of listeriosis most often include fever and muscle pain, which may precede diarrhea or other gastrointestinal symptoms. Almost all patients with listeriosis have infections in which Listeria monocytogenes
has spread beyond the gastrointestinal tract.
Symptoms in pregnant women typically include fever and other nonspecific symptoms such as fatigue and pain. Listeriosis during pregnancy can lead to miscarriage, stillbirth, premature birth, or life-threatening infections in the newborn.
In other groups of patients, symptoms of listeriosis may include headache, stiff neck, confusion, loss of balance, and seizures, in addition to fever and muscle pain.
In patients with normal immunity, listeriosis can cause fever, acute gastroenteritis, or be asymptomatic.
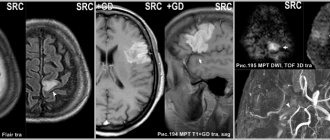
Listeria monocytogenes
is also “responsible” for approximately 5% of all cases of acute bacterial meningitis. It can also cause brain abscess, meningoencephalitis, cerebritis and other infectious diseases of the central nervous system.
By Order of the Ministry of Health and Social Development of Russia No. 1664n dated December 27, 2011 “On approval of the nomenclature of medical services,” medical services were included in the nomenclature of medical services, section 26.
* Sanitary and epidemiological rules SP 3.1.7.2817-10 “Prevention of listeriosis in humans”, approved by Resolution of the Chief State Sanitary Doctor of the Russian Federation of December 29, 2010 N 186.
Listeriosis in ICD-10
In the International Classification of Diseases, 10th revision (ICD-10), in Class I. “Some infectious and parasitic diseases (A00-B99)”, in the block “A30-A49 Other bacterial diseases”, listeriosis is allocated a separate three-character code A32 with the following content:
A32 Listeriosis
.
Included: listeria foodborne infection. Excluded: neonatal (disseminated) listeriosis (P37.2).
- A32.0 Cutaneous listeriosis
- A32.1† Listeriosis meningitis and meningoencephalitis (listeria: meningitis (G01*), meningoencephalitis (G05.0*)
- A32.7 Listeria septicemia
- A32.8 Other forms of listeriosis. Listeria: cerebral arthritis† (I68.1*), endocarditis† (I39.8*). Oculoglandular listeriosis
- A32.9 Listeriosis, unspecified
Notes. A cross † marks the main codes of the underlying disease that must be used. An asterisk indicates optional additional codes that relate to the manifestation of a disease in a separate organ or area of the body that represents an independent clinical problem.
Antibiotics active against Listeria monocytogenes
When treating listeriosis, the antibiotic of choice is ampicillin. Of the antibacterial agents described in this reference, the following are active against Listeria monocytogenes
: clarithromycin, ciprofloxacin, oflaxacin, roxithromycin, tetracycline, vancomycin, azithromycin.
Listeria monocytogenes strain in the treatment of pancreatic cancer
Listeria monocytogenes
strains for immunotherapy of malignant pancreatic tumors . The attenuated strain ΔactA/ΔinlB allows increasing the production of pro-inflammatory cytokines and chemokines, increasing antitumor immunity (Lizotte P et al. Attenuated listeria monocytogenes reprograms M2-polarized tumor-associated macrophages in ovarian cancer leading to iNOS-mediated tumor cell lysis (TUM4P.908) / The Journal of Immunology. May 1, 2014 vl.192 (1 Supplement) 138.9).
Listeria monocytogenes in the taxonomy of bacteria
According to modern classification, the species Listeria monocytogenes
belongs to the genus
Listeria
(Listeria), which is included in the family
Listeriaceae
, order
Bacillales
, class
Bacilli
, phylum
Firmicutes
, <group without rank>
Terrabacteria group
, kingdom Bacteria.
On the website GastroScan.ru in the “Literature” section there is a subsection “Microflora, microbiocenosis, dysbiosis (dysbacteriosis)”, containing articles addressing the problems of microbiocenosis and dysbiosis of the human gastrointestinal tract.
Back to section
What else is prescribed with this study?
Listeria, DNA (Listeria monocytogenes, PCR) scraping, quality.
19.43. Scraping 1 day
430 ₽ Add to cart
Determination of pathogen sensitivity to antibacterial drugs (DDM)
01. 1 day
490 ₽ Add to cart
Determination of pathogen sensitivity to bacteriophages
03. 1 day
220 ₽ Add to cart
Determination of pathogen sensitivity to an expanded range of antibacterial drugs
02. 2 days
600 ₽ Add to cart
Determination of pathogen sensitivity to an expanded range of antibacterial drugs, with determination of the minimum inhibitory concentration (MIC, MIC)
13. 2 days
960 ₽ Add to cart
Determination of sensitivity to antibacterial drugs of ESBL strains
05. 1 day
320 ₽ Add to cart
Determination of sensitivity to antibacterial drugs of MRSA strains
06. 1 day
320 ₽ Add to cart
Determination of sensitivity to antibacterial drugs of the entire spectrum of isolated microflora
09. 1 day
320 ₽ Add to cart
Listeria, L.monocytogenes DNA in blood
Listeria, L.monocytogenes DNA in blood, qualitative
— qualitative determination of L.monocytogenes DNA in blood using the polymerase chain reaction (PCR) method with real-time detection. The PCR method allows you to identify the desired section of genetic material in a biological material and detect single molecules of microorganism DNA that are not detected by other methods. The principle of the method is based on a multiple increase in the number of copies of DNA sections specific to a given pathogen.
Using PCR analysis, it is possible to diagnose infection in the acute period and identify cases of carriage.
Listeria monocytogenes
is a gram-positive bacterium that causes the deadly disease listeriosis.
Listeriosis
- an infectious disease from the group of zoonoses. The reservoir of infection in nature is many types of rodents and domestic animals (chickens, ducks, rabbits, pigs, cows). Listeria is stable in the external environment, persisting for a long time in feces, soil, grain, and can multiply at refrigerator temperatures (+4–6 ºС), but quickly die when heated and under the influence of disinfectants.
In most cases, the main route of infection is the consumption of infected vegetables and fruits and animal products. Contact with animals can also be a source of infection.
The groups most at risk for contracting listeriosis are: pregnant women, newborns, and people with weakened immune systems.
The incubation period is 2–4 weeks.
Clinical signs of listeriosis
The clinical picture of the disease depends on its form. Acute - accompanied by chills, fever, an erythematous rash in the area of large joints, enlarged and painful lymph nodes. In nervous forms, meningeal symptoms appear.
Sometimes in the clinical picture the symptoms of acute gastroenteritis, pyelitis, and endocarditis are in the foreground. Transplacental infection of the fetus is possible during pregnancy. Congenital listeriosis is characterized by the development of a septic condition, which leads to the death of children. Clinical diagnosis is difficult; laboratory confirmation, bacteriological cultures of throat smears are required; blood, cerebrospinal and amniotic fluid, etc. can also serve as material.
Indications:
- suspicion of listeriosis in acute intestinal infections;
- the presence of symptoms of damage to the meninges in the case of a history of infectious diseases;
- erased symptoms in individuals at risk of developing listeriosis.
Preparation
No special preparation is required. It is recommended to take blood no earlier than 4 hours after the last meal.
Blood is drawn into the appropriate tube strictly up to the mark.
Immediately after filling and removing the test tube from the holder, it must be carefully turned 5–10 times 180° to mix the sample with the filler.
Do not shake! Interpretation of results
The result of the study is expressed qualitatively: found” or “not found”.
Normally the result is negative.
"Detected":
- DNA fragments specific for Listeria monocytogenes were found in the analyzed sample of biological material; Listeria monocytogenes infection.
"Not detected":
- DNA fragments specific for Listeria monocytogenes were not found in the analyzed sample of biological material or the concentration of pathogen DNA in the sample was below the sensitivity limit of the test.
References
- Yushchuk, N.D., Vengerova, Yu.Ya. Infectious diseases: national guidelines. - M.: GEOTAR-Media, 2009. - P. 503–513.
- Zaitseva, E.A. System for the analysis of microbiological and molecular genetic markers for identifying highly virulent strains of Listeria monocytogenes: abstract. dis. Doctor of Medical Sciences, 2010. - 27 p.
- Duysenova, A.K., Dmitrovsky, A.M., Shopaeva, G.A. and others. Infectious diseases: modern realities. Health of Kazakhstan, 2016. - No. 01/44.
- Information collection of statistical and analytical materials. Infectious morbidity in the constituent entities of the Russian Federation in 2017-2018. Part 3. - M.: Federal Center for Hygiene and Epidemiology of Rospotrebnadzor, 2021. - 304 p.
- Khramov, M.V., Kostenko, Yu.G., Bataeva, I.V. Listeriosis: laboratory diagnostics in modern conditions: Proceedings of the II National Congress of Bacteriologists, 2021. - T. 6(3).
Listeriosis (Listeria monocytogenis) (qualitative DNA determination)
Listeriosis (synonyms: listerellosis, Tigris disease, neurellosis, granulomatosis of newborns) is an infectious disease from the group of zoonoses. In humans, the disease occurs either in the form of acute sepsis (with damage to the central nervous system, tonsils, lymph nodes, liver, spleen), or in a chronic form (erased).
The causative agent of the disease was first described by S. Halfes (1911). It was identified by D. Murray et al. (1926) from sick rabbits and guinea pigs at the Cambridge University nursery; in connection with the ability to cause pronounced monocytosis in the experiment, the pathogen received the species name monocytogenes. The name of the genus Listeria (in honor of Joseph Lister) was proposed by W. Pirie (1927), who studied the causative agent of the rodent epizootic in South Africa. In 1929, A. Nyfelt isolated bacteria from a person suffering from tonsillitis with high monocytosis. Later, K. Bern observed cases of the disease caused by them in postpartum women and newborns (1935). The causative agent is the motile, non-spore-forming gram-positive bacillus Listeria monocytogenes, the type species of the genus Listeria. It can form a capsule, transform into L-forms and parasitize inside cells, causing a slow latent development of infection. Listeria is microaerophilic, unpretentious and grows on ordinary media even at room temperature. They have a set of somatic and flagellar antigens, which makes it possible to distinguish among them 7 main serovars, many of which are divided into subtypes. The most common are Listeria serovars 1-4. The bacteria are pronounced saprophytes and are highly resistant in the external environment. They tolerate low temperatures well, as psychrophilic microorganisms are able to reproduce at 4-6 ° C in various objects (soil, water, on plants, in corpses and food products). Maintain a 6-20% concentration of table salt for a long time. The sun's rays inactivate them within 2-15 days, a 2.5% solution of formaldehyde or NaOH - after 20 minutes, a solution of bleach (100 mg of active chlorine in 1 liter) - after 1 hour. At 62 °C they die after 35 minutes, at 100 °C - within 5-10 minutes. They are sensitive to broad-spectrum antibiotics, although strains resistant to them are also known. The reservoir and sources of infection are many species of wild and synanthropic rodents, as well as various environmental objects. The disease affects domestic and farm animals (pigs, small and large livestock, horses, rabbits, less often cats and dogs), as well as domestic and ornamental birds (geese, chickens, ducks, turkeys, pigeons, parrots and canaries). Listeria has been found in foxes, minks, raccoons, arctic foxes, wild ungulates, birds, in fish and seafood, and in many natural environments. A particularly favorable environment for their reproduction is the surface layers of low-quality silage. The pathogen is released from the body with various secretions (urine, milk, blood, semen, cerebrospinal fluid, rectal mucus, amniotic fluid, etc.). The period of infectiousness of animals lasts indefinitely. An infected person can be a source of perinatal and neonatal pathology. Postpartum women and newborns can excrete the pathogen within 10-12 days after birth. The transmission mechanism is varied (fecal-oral, contact, airborne, transplacental), the main one is fecal-oral. Animals become infected through listeria-contaminated water and feed, from rodents or their carcasses. Blood-sucking insects, especially pasture ticks, play a certain role in maintaining stationary foci of the disease. By becoming infected from rodents and other sick animals, they contribute to the spread of the infection by transmitting the bacteria to other animals. The mechanisms of human infection are varied. More often, infection occurs through the alimentary route through contaminated water and food products of animal origin, especially in the absence of reliable heat treatment and long-term storage at relatively low temperatures. Possible infection from eating fresh vegetables. The possibility of aerogenic contamination occurring during the processing of animal raw materials (wool, bristles, leather, skins, feathers, down) has been established. The contact route of transmission is known, through cuts and abrasions on the skin when various secretions of sick animals get into them. The possibility of transmission of bacteria from person to person has been identified, and cases of sexual transmission have been described. Listeriosis is especially dangerous for pregnant women due to perinatal transmission of the pathogen from mother to child (transplacentally or during childbirth). Cases of postpartum aerogenic, contact and food infection of newborns from the mother, medical personnel or environmental objects infected by them have been described. People's natural susceptibility is low. Diseases occur most often in the elderly, newborns, and in people with immunodeficiencies. Post-infectious immunity is weakly expressed. Basic epidemiological signs. The disease has all the features of a saprozoonosis infection and is widespread. It is most often found in areas with temperate climates and soils rich in organic fertilizers. The spread of listeriosis is facilitated by large-scale human economic activity associated with the introduction of advanced soil cultivation technology, the construction of livestock complexes, feed mills, centralized enterprises for the processing and sale of raw materials of animal origin, food warehouses and storage facilities. In Russia, 50-80 cases of listeriosis are registered annually, which does not reflect the actual incidence rate. Sporadic and group diseases are possible. The risk group includes pregnant women and newborns. The incidence of the disease is occupational in nature among workers in livestock and poultry farms, as well as in primary processing shops at meat and poultry plants. The incidence is more often recorded in the spring and summer. As a nosocomial infection, listeriosis is most relevant for obstetric hospitals, where sporadic cases and outbreaks of listeriosis have occurred, and pregnant women and newborns are considered risk groups. The entry points for infection can be the mucous membranes of the gastrointestinal tract and respiratory tract, eyes, as well as damaged skin. With the lymphogenous and hematogenous spread of pathogens, an acute febrile state occurs, and listeria is fixed in the lymph nodes and internal organs - tonsils, lungs, liver and spleen, kidneys and adrenal glands, central nervous system, etc., where bacteria multiply. The inflammatory process in the lymph nodes is accompanied by their enlargement, but suppuration does not develop. In severe cases, the disease takes on the features of listeriosis sepsis; at the same time, small numerous necrotic nodules (listeriomas) are formed in the lymph nodes and internal organs (including the central nervous system), which include listeria, reticular and monocytic cells, nuclear detritus, and altered polymorphonuclear leukocytes. During pregnancy, listeriomas can form in the placenta, which subsequently leads to infection of the fetus with the development of a generalized form of infection. The occurrence of the disease is facilitated by immunodeficiency states and tumors. Those who have recovered develop persistent post-infectious immunity. The disease can acquire an acute, subacute, chronic and abortive course, usually prone to recurrence. The following main clinical forms of listeriosis are distinguished: anginal-septic, nervous, ocular-glandular, septic-granulomatous (in fetuses and newborns), mixed. There are cases of long-term asymptomatic listeria carriage.
Incubation period. Varies from several days to 1.5 months.
Anginous-septic form . Seen most often. The main clinical manifestation is tonsillitis. It can be catarrhal or follicular, clinically indistinguishable from streptococcal tonsillitis. Usually in such cases the disease progresses favorably within 5-7 days and ends with complete recovery. With ulcerative-membranous listeria sore throat, the body temperature rises to 38.5-39 °C, a cough and runny nose are possible, and a sore throat is characteristic. In patients, marked hyperemia of the mucous membrane of the oropharynx, enlargement and looseness of the tonsils, and the formation of filmy deposits or ulcers covered with films are noted on them. Regional lymph nodes are enlarged and painful on palpation. Ulcerative membranous tonsillitis is characterized by changes in the hemogram - leukocytosis, an increase in ESR and especially an increase in the number of mononuclear cells (up to 70% or more). The duration of the disease in cases of its favorable course is 12-14 days. At the same time, ulcerative-membranous and, much less frequently, follicular listeriosis tonsillitis, as the process progresses, can lead to the development of sepsis, which is observed mainly in adults. High fever takes on a remitting nature, facial hyperemia, conjunctivitis, a polymorphic rash on the skin, and white plaque on the tonsils are noted. Hepatolienal syndrome develops, and in some cases mild meningeal symptoms appear. Severe monocytosis remains in the blood. The outcome of listeria sepsis with timely and complete treatment is favorable. Nervous form . Manifests itself in the form of listeria meningitis, meningoencephalitis or brain abscess. The clinical characteristics of these conditions do not differ significantly from the corresponding nosological forms of other bacterial etiologies. Monocytosis in the peripheral blood is noted in the nervous form of the disease only in its early period; later leukocytosis and granulocytosis are detected. The cerebrospinal fluid usually remains transparent, cerebrospinal fluid pressure and protein content are increased, cytosis is mixed, and glucose and chloride levels change slightly. Damage to the peripheral nervous system can be observed - paresis and paralysis of individual muscle groups, polyradiculoneuritis. In immunodeficiency conditions, including HIV infection, the nervous form of listeriosis manifests itself as an opportunistic infection. Ocular-glandular form. Rarely observed; it usually results from contact with infected animals. Patients experience increased body temperature and decreased visual acuity. Conjunctivitis develops with swelling of the conjunctiva and numerous follicles on it, swelling of the eyelids, narrowing of the palpebral fissure, enlargement and slight soreness of the parotid and cervical lymph nodes. The cornea remains unchanged. The disease lasts a long time, from 1 to 3 months. Septic-granulomatous form. Observed in fetuses and newborns. During pregnancy, listeriosis can occur in erased and atypical forms or in the form of asymptomatic carriage and in such cases remains unrecognized. If the fetus is infected intrauterinely in the early stages of pregnancy, its death or severe developmental anomalies (hydrocephalus, microgyria, etc.) are possible. Listeriosis in newborns is characterized by a severe course. Manifested by high fever, respiratory and circulatory disorders: dyspnea, cyanosis, deafness of heart sounds. Possible vomiting, mucous stool, exanthema of a roseolous-papular nature. With the development of purulent meningitis, death is most often observed. Clinically, listeriosis in newborns is rarely recognized due to its similarity to other intrauterine infections. In infants, listeriosis begins as an acute respiratory viral infection with an increase in body temperature, runny nose, cough, then small-focal bronchopneumonia or purulent pleurisy develops. Some patients experience exanthema of a maculopapular nature, enlarged liver, jaundice, meningeal symptoms, sometimes convulsions, and paralysis. Characteristic monocytosis in the hemogram is rare. When recovering from this form of listeriosis, 15-20% of children remain with disorders of the peripheral nervous system and central nervous system. Chronic listeriosis. It is distinguished by the paucity of clinical manifestations during exacerbations of the disease: short-term fever with catarrhal symptoms, quite often dyspeptic disorders or sometimes symptoms of chronic pyelonephritis are observed.