Local therapist
Serebryakova
Oksana Evgenievna
Experience 27 years
Local therapist, candidate of medical sciences, member of the Russian Scientific Medical Society of Therapists
Make an appointment
The patient's condition is considered febrile if the body temperature rises above 37.2°C. This condition is not an independent disease, but is regarded as a sign of a serious pathology - an inflammatory process, infection, oncology. Less commonly, body temperature rises when taking certain medications and during heat stroke. Also, the temperature can fluctuate around the specified value during the day - decrease at night during sleep and increase in the evening due to intense exercise. For a healthy person, the range of daily fluctuations usually does not exceed 0.6°C.
Classification of fever
Depending on the level of body temperature, the following method of classifying fever is used:
- subfebrile temperature within 37.2 - 37.9°);
- febrile temperature at 38.0 – 38.9°C;
- pyretic temperature at 39.0 – 40.9 °C;
- hyperpyretic temperature starts at 41°C.
Attempts to cope with the rise in temperature are selected depending on its level. For low-grade fever, intervention is not recommended. The exception is pathology, when even a slight increase in temperature causes significant inconvenience to the patient. As the parameter increases, measures must be taken to stabilize it. Moreover, in the overwhelming majority of cases, the symptoms of fever indicate a serious problem in the body, to which it reacts by attempting to destroy the cause through high temperature or defeat it through the production of antibodies. Even if the temperature has been reduced, it is necessary to seek medical help and undergo the recommended diagnostics to clarify the cause of the fever and the immune response.
Basic information about the pathological symptom
What is typical for hectic fever? Until recently, people classified this pathological condition as a disease characterized by a significant increase in body temperature. However, modern medicine classifies it not as a separate disease, but as a peculiar reaction to various irritants, which are certain pyrogenic substances.
Thus, we can safely say that hectic fever is a pathological process that is aimed at protecting and adapting the body. It should be especially noted that without medical control, this condition poses a rather serious threat to the patient’s life.
Symptoms
With a slight increase in temperature, a person does not feel any discomfort and continues to lead his usual lifestyle. Rarely, there may be a feeling of discomfort due to temperature differences and a feeling of heaviness in the head area. When the temperature rises to 38.0 °C or more, characteristic “feverish” symptoms appear:
- redness of the skin of the face and body;
- inflamed eyes, caused by increased tear production;
- intense sweating associated with the body’s attempt to reduce the increased temperature;
- headache;
- aches in muscles and joints;
- decreased appetite;
- rapid breathing;
- drowsiness, immobility.
Children may experience a different course of the febrile process. “Red” fever is characterized by a slight deterioration in the condition, maintaining a comfortable temperature of the extremities and relatively stable health. With “white” fever, the child becomes lethargic, his skin turns pale and acquires a bluish tint, the pulse becomes faster, and blood pressure is higher.
Origin and list of diseases
Hectic fever is characteristic of many ailments. Before listing them, it is necessary to identify why such a condition occurs in the first place.
As is known, hyperthermia is a polyetiological secondary condition. The process of restructuring in the work of the thermoregulation center begins with the activity of certain pyrogenic substances in the body. Moreover, the latter are divided into exogenous, or infectious, and non-infectious, that is, endogenous.
So why does hectic fever develop?
What diseases does it occur in? This pathological condition can develop for 2 different reasons. Let's look at them right now:
- An infectious process manifested in the form of inflammatory diseases. These include tuberculosis, influenza, sepsis of the blood, as well as internal organs.
- Non-infectious origin. This condition can cause tissue necrosis, oncology, allergies, blood transfusions and internal hemorrhages.
Diagnostics
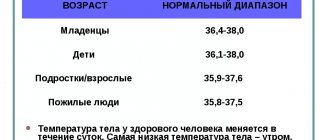
You can check your body temperature by measuring it with a mercury or electronic medical thermometer. It is placed in the armpit so that the shoulder fits tightly to the chest and a sealed space is maintained inside the armpit. In children and weakened patients, the hand with the thermometer should be held. The measurement duration is about 10 minutes. When assessing the actual indicator, you should focus on the level of 36.4-37.2 ° C - a temperature in the specified range is considered normal.
When measuring temperature in young children, use a special rectal thermometer designed to measure body temperature through the anus. However, this method has several contraindications. These are anal fissures, pronounced hemorrhoids and inflammation of the rectum, which excludes any additional trauma to the mucous membrane. The measurement is taken with the patient positioned on his side, with his knees pressed to his chest. The thermometer is inserted into the anus so that the measuring tip goes completely inside. To obtain the desired parameter, 2-3 minutes are enough, and the range of 37.1–37.9 ° C is considered normal.
An oral method of measuring temperature, for which a safe electronic thermometer is used, is considered acceptable. The normal variant here is the range of 36.7 -37.4°C. However, the data may be distorted due to the patient's recent consumption of hot or cold foods and drinks.
Establishing the fact of a febrile state is only part of the diagnostic measures. The doctor needs to find out what caused the increase in body temperature. For a more precise diagnosis of fever, the patient is referred to:
- radiography;
- ultrasonography;
- blood and urine tests;
- other diagnostic procedures.
Periodic fever syndromes
These syndromes refer to diseases that cause periodic (episodic) fever that do not have an infectious (viral, bacterial) cause. In pediatrics, children with these syndromes do relatively well between episodes of fever.
Many of these syndromes are hereditary and result from mutations in genes. The name of the syndromes depends on: defect (mutation); clinical features of the syndrome, affected parts of the body, the age of the child (at the initial manifestations of the syndrome) and the ethnicity of the child and parents. Most of these syndromes have specific treatments, often based on understanding the problem caused by the genetic defect.
Familial Mediterranean fever (FMF) is the most common periodic fever syndrome. Patients with this syndrome suffer from repeated episodes of fever accompanied by abdominal, chest and joint pain and swelling. The disease usually affects people of Mediterranean and Middle Eastern descent, typically Sephardic Jews, Turks, Arabs and Armenians. The diagnosis of familial Mediterranean fever can be made from the discovery of a gene mutation, which is diagnosed more often in populations where the disease is considered very rare, such as Italians, Greeks and Ashkenazi Jews. Exacerbations (relapses of fever) of FMF begin before the age of 20 years in approximately 90% of patients, and in more than half of patients, the disease appears before the age of 10 years. So, FMF is a genetic disease. The gene responsible is MEFV, named after the Mediterranean Sea, and affects a protein called pyrin, which plays a role in the natural control of inflammation. When this gene is mutated, inflammation cannot be properly regulated, and patients experience episodes of fever and other symptoms (infection, trauma, menstruation, or psychological stress can cause these episodes). FMF is inherited as an autosomal recessive disorder (meaning that although the child may have the condition, neither parent will show symptoms of the condition). In this case, the child receives two mutated genes, one from the mother and one from the father (such parents are called “carriers” or “carriers”), often someone in the family (“extended family”) has a similar disease. If one child has the disease and the parents are carriers, 25% of the other children in that family have a chance of getting FMF. If one child has FMF and one parent also has FMF, there is a 50% chance that the other child will develop FMF. FMF fever is not contagious.
The main symptoms of the disease (FMF) are recurrent fever accompanied by pain in the abdomen, chest or joints. However, not all children will necessarily have all the symptoms, and symptoms may change over time. Episodes of fever usually resolve without treatment and last one to four days. Most children are completely healthy between episodes, but for some children, frequent episodes do not allow full recovery and these children do not develop properly. Some of these "attacks" can be so painful that the patient or family seeks medical attention from an emergency (or urgent care) service. For example, severe abdominal attacks may mimic acute appendicitis, and therefore some patients undergo appendectomy. Chest pain may be so severe that it may be difficult for the patient to breathe deeply. Usually only one joint is affected at a time, most often the ankle or knee. The joint may be so swollen and painful that the child cannot walk. About a third of these patients develop a red rash along the involved joint. In some children, the only symptom of the disease may be episodes of joint pain and swelling, which are misdiagnosed as acute rheumatic fever or juvenile idiopathic arthritis. Joint swelling usually resolves within 5-14 days. In approximately 5-10% of cases the disease can become chronic. Some children report pain in their leg muscles. Relatively rarely, children suffer from relapse of pericarditis, myositis, meningitis and orchitis. Frequent episodes of illness can affect the child and family's life, including school attendance.
The most severe complication of FMF if left untreated is the development of amyloidosis. Amyloid is a protein that deposits in certain organs in children with chronic inflammatory diseases that are not well controlled. The most common site of amyloid deposition is the kidney, but amyloid can also be found in the intestines, skin, and heart. In adults, the disease often takes a milder and less hidden course and is more difficult to diagnose than in children (the risk of developing amyloidosis is lower in adults).
Although FMF is a genetic disorder, the genetic mutation does not occur in all children with FMF, so the diagnosis of FMF is still based on clinical signs. FMF is suspected in children with episodic fever, an ethnic background typical of FMF, and/or a family history of FMF or, in advanced cases, unexplained renal failure. Children often initially have episodes of fever without other symptoms, so close monitoring of sick children is required (family members should write a diary documenting the episodes and a description of what is happening) until a clinical diagnosis is made by a specialist. Because most children do not have typical episodes, it can take a long time to suspect FMF and make a correct diagnosis. In general, inflammation tests become positive during an episode and return to normal, or nearly normal, after the episode ends. The urine sample is also tested for the presence of protein.
FMF cannot be completely cured, but the syndrome can be well controlled with lifelong use of colchicine. Thus, while episodes are usually completely preventable in 60% of patients, partially preventable in 33% of cases, and approximately 5% of patients do not respond to colchicine therapy, amyloidosis is preventable in 100% of patients. If the patient stops taking the drug, episodes often occur after missing only one dose, and the risk of amyloidosis reoccurring is quite high. Colchicine prevents episodes from starting, but does not affect an episode that has already started. Therefore, the dose of colchicine should not be increased during an active episode of illness. Colchicine is a safe drug with minor side effects (the most common side effect is diarrhea) that usually respond to dose reduction. Other methods include reducing the consumption of milk or dairy products, and sometimes it is necessary to give medicine to treat diarrhea. Other side effects include nausea, vomiting and abdominal cramps. Children treated with colchicine should have their blood and urine tested at least twice a year.
TRAPS is an autosomal dominant genetic disease (one gene defect is sufficient to transmit the disease in families). This means that one of the parents has the disease or that the gene defect has been created again in a child with the disease (de novo mutation). Besides episodes of fever, other symptoms include: abdominal pain, diarrhea, restlessness, painful red skin rash, muscle pain and swelling around the eyes. The gene defect was discovered relatively recently. The former name for this syndrome was familial fever. TRAPS is a rare disease, but since the gene mutation has been identified, a large number of patients have been found with varying clinical features. Thus, the actual incidence of this syndrome is not yet known. This disease affects both men and women equally, and onset probably occurs in late childhood or adulthood. The first cases were reported in patients with Irish-Scottish ancestry; however, the disease has also been identified in almost all ethnic groups.
TRAPS is caused by a gene defect in a protein called tumor necrosis factor receptor (TNFR), which results in an increase in the patient's normal inflammatory response. The protein that causes inflammation is called tumor necrosis factor (TNF) because the receptor (TNFR) that normally binds to TNF is missing when attempting to control its activity. Infection, injury, or psychological stress may cause episodes. However, not every person who has the gene defect will have clinical signs of TRAPS.
The main symptoms are recurrent episodes of fever, usually lasting two or three weeks, accompanied by chills and intense muscle pain in the trunk and upper extremities. The rash is typical: red and painful, which is a reflection of inflammation of the skin and muscles. The rash moves from one place to another on the body, usually from the arms and legs to the torso. Most patients feel muscle spasms during attacks, which gradually increase in strength and also move from one part of the body to another. Abdominal pain with nausea and vomiting is also common. Inflammation of the lining covering the front of the eye (conjunctiva) and/or swelling occurring around the eye is common. Other less common symptoms include: chest pain, due to inflammation of the pleura or pericardium. As with FMF, amyloidosis is the most severe late complication of TRAPS and often results in large amounts of protein in the urine and kidney failure. Symptoms of the disease vary in severity from person to person and also depend on the duration of the episodes and the time between them (the duration of the clear intervals). The reasons for this are based in part on differences in the specific gene defect. The diagnosis is confirmed only by genetic tests showing a genetic defect in the TNFR gene.
Nonspecific anti-inflammatory drugs, including the use of steroids, help relieve symptoms, but long-term use of steroids leads to serious side effects. Giving a drug similar to the TNF receptor called Enbrel (a drug used to treat juvenile idiopathic arthritis) has been shown to be an effective treatment in some patients when it is given at the onset of an attack or even as a preventative measure. Patients with TRAPS typically have episodes of exacerbation of symptoms throughout their lives.
HIDS (hyperimmunoglobulin D syndrome) is an autosomal recessive genetic syndrome that causes episodic high fever with skin rash, swollen lymph nodes in the neck, abdominal pain, vomiting and diarrhea. The disease begins in early childhood. The name of this disease comes from the fact that most patients have very high amounts of immunoglobulin type D. The most severe form of this disease begins at birth and is called mevalonic aciduria. These patients also have symptoms of nervous system damage and suffer from short stature. HIDS is a very rare disease. The disease is more common in Western Europe, especially the Netherlands and France, but has been described in all ethnic groups. Boys and girls are equally affected. Symptoms of HIDS usually begin in early childhood, most often in the first year of life.
HIDS is a genetic disease. The gene defect is found in a protein called mevalonic kinase (MVK). MVK is a protein that facilitates a chemical reaction in the body (enzyme) involved in the process of cholesterol formation. In HIDS, the MVK enzyme is active in only 1-10% of normal enzyme activity. Episodes can be caused by infection, stress and vaccinations, or occur without any obvious trigger. Episodes of fever are the main symptom, lasting three to seven days and recurring every 2 to 12 weeks. The attacks begin suddenly, often with chills. Headache, stomach pain, loss of appetite and flu-like symptoms are common signs of this disease. Most patients complain of nausea, vomiting or diarrhea. Skin rashes, painful mouth sores, and joint pain are noted in HIDS, but the most striking feature of the disease is swelling of the lymph nodes in the neck or other parts of the body. Most (but not all) patients, especially very young ones, have elevated immunoglobulin D levels.
Treatment options for fever
Stabilization of body temperature and treatment of fever is carried out using the following methods:
- Taking antipyretic medications. This could be paracetamol, aspirin (contraindicated in children under 12 years of age), ibuprofen tablets or syrup. The advantages of the liquid composition are the possibility of its precise dosage and ease of swallowing, which is especially important for children. It is possible to take powders containing the listed antipyretic substances, which simultaneously have an analgesic and anti-inflammatory effect.
- Compliance with bed rest, due to which the patient’s condition improves somewhat.
- Reviewing your diet in favor of frequent small meals. Priority is given to dishes with a liquid or puree consistency, the digestion of which causes the body to spend less energy. You should completely exclude the use of hot and spicy dishes, seasonings and salty foods that draw water from the body.
- Drink plenty of fluids to prevent dehydration.
- Taking medications to treat the underlying cause of the fever. These could be antibiotics, non-steroidal anti-inflammatory drugs, etc.
If the temperature rises after heat stroke, measures should be taken to reduce it. For this, the patient is wiped with cool water, given plenty of clean water to drink, covered with ice packs and wrapped in wraps.
Fever of unknown origin: treatment
CELT hematologists develop treatment tactics based on the results of diagnostic studies and individual patient indications. Most often, when his condition is stable, treatment is abstained. At the same time, it is possible to discuss trial measures using pharmacological drugs for tuberculosis, thrombotic deep vein injuries or pulmonary embolism in cases where these diseases are suspected. According to indications (suspicion of thyroiditis, rheumatoid arthritis and polymyalgia), glucocorticoids are prescribed: their use is justified if the results help in diagnosing the underlying problem.
It is very important for the doctor to have data on the use of pharmacological drugs that the patient with fever has previously practiced, since the reaction to them in 5% of cases can manifest itself as an increase in temperature. Moreover, it is quite often a key sign of sensitivity to them. Most often, fever does not develop immediately after taking them, which makes it difficult to determine the cause. Experts identify different groups of medications that can cause fever of unknown origin:
- Antibiotics of the penicillin, nitrofuran, tetracycline group;
- Cytostatics;
- Medicines that affect the central nervous system;
- Anti-inflammatory drugs;
- Means for the treatment of pathologies of the gastrointestinal tract;
- Antihistamines;
- Medicines based on iodine.
At CELT, consultations are conducted by hematologists of the highest category, candidates and professors of medical sciences with many years of experience in practical and scientific work. You can schedule a consultation with them online or by phone. Since our clinic is multidisciplinary, we also offer the services of highly qualified urologists. They can undergo lithotripsy and remove kidney stones in a gentle way.
At CELT you can consult a hematologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
By making an appointment with a hematologist, you can get a comprehensive consultation. The doctor is competent to treat various blood diseases, most of which can be identified in the early stages and prescribe timely treatment to cope with the disease quickly and easily.
Diagnosis and treatment of fever at the clinic of JSC "Medicine" in Moscow
If signs of fever persist for several days without other visible symptoms, it is recommended to stop self-medicating and seek medical help. You can get it at the clinic of JSC "Medicine" in the Central Administrative District of Moscow, which has its own diagnostic center and outpatient clinic for undergoing prescribed procedures. Patients of the clinic invariably receive attentive attention, the opportunity to save time and money on undergoing research, as well as a guarantee of the security and confidentiality of personal information. Appointments can be made by phone or on the center's website.
Treatment
Treatment of fever should serve two purposes. Maintaining the functioning of internal organs, especially the respiratory, cardiac and excretory systems. And also to combat hyperthermia. For this purpose, not only medications can be used, but also physical effects on the body.
The patient is removed from his clothes and goes to bed with his head slightly raised. The head and wrists are covered with cold compresses from soaked bandages or ice packs. The body is wiped with a 3% solution of vinegar, alcohol or just cool water. Additionally, you can use a blower fan or air conditioner.
The patient may undergo gastric lavage and water enemas, just as the patient would. All intravenous infusion solutions are also stored in the refrigerator. At this stage, it is important that the body temperature reaches a maximum of 37.5 °C, as the body itself will continue to decline under the influence of the above measures.
Prescribed medications include antipyretics and antiallergic drugs in the form of intramuscular injections. These may be brufen and its analogues, solutions of acetylsalicylic acid and analgin with diphenhydramine or suprastin. Aminazine or lytic compounds are recommended for hyperactivity.
Resuscitation is performed in case of respiratory failure or cardiac arrest. If there is a threat of cerebral edema, magnesium sulfate is used. Prednisolone is used for hypotension and seduction to control attacks.