Tetanus is a serious disease caused by a bacterial toxin that attacks the nervous system and leads to painful muscle contractions, especially in the jaw and neck muscles. Tetanus can interfere with the ability to breathe and can be life-threatening. The main habitat of dangerous bacteria is soil, saliva and animal feces.
The daily life of children and adults is impossible without injuries that affect the integrity of the skin and mucous membranes. And if the wound is contaminated with soil elements in the absence of immunity to tetanus, this can cause an infection to develop. The tetanus vaccine is the only protection against this disease. In order for the human body to develop immunity to the disease, it is necessary to administer special vaccines containing neurotoxin and tetanus toxoid. When children receive a tetanus shot, these substances are released into the bloodstream, activating the immune system and producing protective antibodies.
Where can I get a tetanus shot? The RebenOK clinic in Moscow vaccinates the population in accordance with established standards and deadlines. You must first make an appointment with a pediatrician to rule out possible contraindications.
Why is tetanus dangerous?
Once tetanus toxin binds to nerve endings, it cannot be removed. To fully recover from a tetanus infection, new nerve endings must develop, which may take several months.
Consequences of tetanus infection:
· Fractures. The severity of muscle spasms can lead to fractures of the spine and other bones.
· Development of pulmonary embolism. A displaced clot may block the main artery of the lung or some of its branches.
· Death. Severe muscle spasms caused by tetanus can cause respiratory failure, which is the most common cause of death.
To prevent a sad outcome, it is recommended to vaccinate your child against tetanus on time.
Types of vaccines
The tetanus vaccine is an inactivated vaccine (not live) and contains a toxin produced by the bacterium but has no toxicity (toxoid). Once injected, it cannot cause disease, but retains its ability to stimulate the production of antibodies. The tetanus vaccine is always part of a combination vaccine that includes other components.
Where do you get the tetanus shot? It all depends on the drug. The vaccine is administered intramuscularly into the subscapular region, thigh or shoulder.
Types of tetanus vaccines at the RebenOK clinic:
· "Adasel". The vaccine is intended for patients 4-64 years of age. Efficacy and safety have been confirmed. Revaccination is carried out once in a dose of 0.5 ml. The vaccine is injected into the deltoid muscle of the shoulder intramuscularly.
· "ADS-M". Used for children aged 6 years and adults. Introduced every 10 years. It is prescribed mainly if other drugs need to be replaced due to complications. Forms strong immunity. Requires revaccination every 10 years. The graft is introduced under the shoulder blade or into the anterior outer part of the thigh.
· "DTP". Adsorbed drug for tetanus, diphtheria and whooping cough. It is carried out for children from 3 months of age to 4 years. Vaccination consists of three injections with an interval of 45 days, followed by revaccination one year after the third vaccination. Good protection is guaranteed if revaccination recommendations are followed.
· "Pentaxim". Vaccination against tetanus, diphtheria, whooping cough, polio and infection caused by Haemophilus influenzae. Forms stable immunity throughout life. The vaccine is given to children from 3 months of age.
· "Infanrix Hexa" (Belgium). A combined drug for tetanus, hepatitis B, diphtheria, Haemophilus influenzae, whooping cough and polio.
The choice of drug remains with the doctor. The pediatrician must first study the child’s medical history and select the most appropriate vaccine, taking into account individual characteristics.
Clinical manifestations
The incubation period of the disease varies from a day to a month, but more often it is 7–14 days. The initial symptoms of tetanus (prodromal period) are not observed in all patients and include headache, twitching and muscle tension in the wound (complete healing of the wound is often observed), sweating, malaise, and irritability. More often, the first manifestation of the disease is a dull, nagging pain at the site of infection. Later, specific signs of the disease appear:
- There is convulsive compression and tension of the masticatory muscles, which makes it difficult to open the mouth and is called trismus;
- A “sardonic smile” appears, which can be described as both malicious and mocking (the forehead wrinkles, the eyes narrow, the lips stretch into a smile, but the corners of the mouth droop);
- A swallowing disorder or dysphagia develops, as a convulsive spasm of the pharyngeal muscles occurs, making it difficult and painful for the sick person to swallow;
- There will be stiffness (tension) of the neck muscles, but there are no other meningeal symptoms.
The presence of the first three symptoms in a person confirms a tetanus infection.
- The height of the disease
It is characterized by the occurrence of tonic spasms that spread to the muscles of the trunk and limbs, excluding the hands and feet. Tonic muscle tension is very painful and constant, persisting during sleep. On the third or fourth day of the disease, the abdominal muscles become stiff, movements in the limbs become difficult, the intercostal and diaphragmatic muscles spasm, which is accompanied by rapid shallow breathing. Tonic spasms also spread to the muscles of the perineum, intestines and urethra, resulting in difficulty urinating and defecating.
- Convulsive syndrome
Later, convulsive syndrome occurs. In the case of a mild course of the disease, convulsions occur no more than 5 times a day and last several minutes; severe tetanus is characterized by constant and continuous convulsions. Any stimulus can provoke convulsive contractions: light, sound, tactile contact. Cramps are very painful and can involve arbitrary muscle groups, resulting in the patient taking bizarre positions. During convulsions, the patient's face turns blue, becomes puffy and covered in perspiration.
- Development of opisthotonus
Total muscle contraction, including severe tension of the back muscles, leads to opisthotonus: the patient arches, touching the surface of the bed only with the back of the head and heels, the elbows are bent, the hands are clenched into fists, and the legs are extended. The patient begins to experience severe fear and scream due to sharp pain, suffocates and clenches his hands into fists or grabs the edges of the bed. At the same time, the temperature rises, sweating and salivation increase.
Tetanus in adults can manifest itself as local symptoms or generalized ones. The duration of the incubation period depends on the proximity of the entry gate of infection to the brain and spinal cord. If the wound is located on the face or neck, the incubation period is reduced to 1 - 3 days. Tetanus in children (newborns) is characterized by a shortening of the incubation period to several hours (the infection penetrates through the umbilical cord, from where it quickly reaches the central nervous system through the bloodstream).
Contraindications
Tetanus vaccination for children has low reactogenicity, so there are practically no restrictions on the composition. The main contraindication is the occurrence of allergic reactions or neurological damage after the previous injection.
Temporary contraindications for tetanus vaccination:
· influenza and acute respiratory infections;
· diathesis, eczema and other skin manifestations;
allergic reactions and immunodeficiency;
· increase in body temperature.
In these cases, vaccination is carried out after complete recovery. A preliminary consultation with a pediatrician is mandatory.
Contraindications to the use of specific means of emergency prophylaxis of tetanus
The main contraindications to the use of specific tetanus prophylaxis are:
- pregnancy (in the first half, the administration of AS (ADS-M) and PSS is contraindicated, in the second half - PSS);
- increased sensitivity to the appropriate prophylactic agent;
- in persons who had contraindications to the administration of AS (ADS-M) and PSS, the possibility of emergency prophylaxis with the help of PSCI is determined by the attending physician.
Alcohol intoxication is not a contraindication to emergency prevention.
Advantages and disadvantages
The clinical effectiveness of tetanus toxoid is estimated at 100%. After the initial vaccination series, all vaccinated individuals have antibody titers above the level of protection. How long does the tetanus shot last? Protective antibodies in properly vaccinated people last for more than 20 years.
The decrease in the incidence of tetanus since the introduction of systematic vaccination confirms the effectiveness in preventing this disease. Tetanus toxoid is considered a safe drug.
Adverse reactions
All vaccines should be considered medicine and may have side effects. In the case of the tetanus vaccine, adverse reactions are moderate.
The most commonly reported symptoms are:
· pain, redness and inflammation at the injection site;
· headache and slight fatigue;
Nausea and vomiting (especially in adolescents).
Currently, there are fewer contraindications, as purified antigens are used. If adverse reactions occur, you should consult a doctor to prescribe symptomatic therapy.
Is there a fever after vaccination?
A slight increase in temperature after vaccination should not cause alarm. This is how the child’s body can react to the injected substance. The process of processing vaccination antigens and the formation of immunity to the disease occurs. Components are released that cause an increase in temperature.
It should be remembered that any manifestations are individual in nature. Adults and children may react differently.
If the temperature does not rise above 37.5 degrees and lasts no more than 3 days, there is no need to consult a doctor. This is considered a normal reaction of the body. Fever, as a reaction to vaccination, usually appears after 5-7 hours, in some babies the next day. If the temperature lasts longer and an increase is noted, you should seek help, as there may be other causes for this symptom.
Risk of post-vaccination complications
As with any other vaccine, in rare cases allergic reactions to vaccine components are possible. These complications are not related to the properties of the vaccine, but to the amount of excipients in specific preparations, whether the child is allergic to them and, in some cases, non-compliance with vaccination rules. It is significant that, according to statistics of post-vaccination complications in the United States, even severe allergic reactions to DTP vaccines have not led to serious consequences in any case since 1978, taking into account the fact that about 80 million vaccinations were given during this period. Possible specific complications of DTP vaccines include neurological complications, which are extremely rare. It is assumed that they may be caused by the fact that the toxins of pertussis bacillus (even inactivated) in combination vaccines tend to irritate the meninges of an extremely small proportion of susceptible children. Complications in the form of encephalopathy are less than 1 case per 300 thousand vaccinated people.
Currently, in the world, convulsions without fever are not considered a complication of vaccination. Research conducted in Great Britain in 1960-1970. indicate the same frequency of seizures in vaccinated and unvaccinated children. Moreover, the first manifestations of diseases such as epilepsy, organic damage, and are associated with vaccination only by a temporary factor.
The development of afebrile seizures indicates the presence of an organic lesion of the nervous system in the child, which was not taken into account and identified or could not be identified before vaccination for objective reasons. Therefore, in the event of afebrile seizures, a comprehensive neurological examination is necessary to make a diagnosis.
How many vaccinations are given against tetanus?
In the children's clinic, during preventive examinations, parents are informed when tetanus vaccinations are given. Full vaccination of children includes the administration of a total of 6 doses of the drug in accordance with the recommendations of the childhood vaccination schedule:
· 3 doses during the first year of life at 45-day intervals, starting at 3 months of age (3.4, 5 and 6 months), administered as a combination pentavalent or hexavalent vaccine;
· after a year, a booster (additional) dose is administered - in the form of a pentavalent combined vaccine;
· 6-7 years another dose that uses low antigen load vaccine in combination with diphtheria toxoid and low antigen load pertussis component (dpaT), standard combination (DPaT) can also be used.
· At 14 years of age, another dose is given using a low-load vaccine (diphtheria toxoid antigen plus tetanus pertussis toxoid (dpaT)).
How often do you get a tetanus shot? Revaccination is offered every 10 years to the entire population.
Active-passive prophylaxis of tetanus
AC should be administered in a volume of 1 ml, having previously read the instructions for the drug. At the same time, PSCH 250 IU must be injected into another part of the body; in the absence of PSCH, 3000 IU PSS must be injected. Before administering PSS, an intradermal test with horse serum diluted in a ratio of 1:100 is required to determine sensitivity to horse serum proteins (the ampoule is marked in red). An intradermal test cannot be performed if the victim was tested with 1:100 diluted anti-rabies gammaglobulin from horse serum for 1-3 days before the administration of PSS due to the need to administer anti-rabies gammaglobulin.
To perform the test, you need to use an individual ampoule, as well as sterile syringes with 0.1 ml graduations and a thin needle. The serum diluted 1:100 is injected under the skin into the flexor surface of the forearm in an amount of 0.1 ml. The reaction is monitored after 20 minutes. The test is considered negative if the diameter of the swelling or redness at the injection site is less than 1.0 centimeters.
The test is considered positive if the swelling or redness in diameter is 1.0 cm or more. If the skin test is negative, PSS (from an ampoule marked in blue) is injected subcutaneously in a volume of 0.1 ml. If there is no reaction after half an hour, you need to inject the remaining dose of serum with a sterile syringe. During this period, the opened ampoule with PSS should be covered with a sterile napkin.
Note : For people with allergic diseases and reactions to various allergens, as well as those who have previously received drugs containing horse serum (PSS and others) or heterologous gammaglobulins (anti-rabies, anti-encephalitis, etc.), it is best to resort to the administration of antihistamines before administering the main dose of PSS.
Persons with a positive reaction to intradermal injection of 0.1 ml of horse serum diluted 1:100 or who had a reaction to subcutaneous injection of 0.1 ml of PSS cannot undergo further administration of PSS.
Considering that after the administration of PSS and drugs that contain tetanus toxoid, particularly sensitive individuals may develop shock, each vaccinated person must be monitored medically for 60 minutes after vaccination. And the institution where people are vaccinated should be provided with anti-shock therapy in case of need.
Importance of vaccination
The causative agent of tetanus - clostridium (tetanus bacillus) is widespread everywhere and is resistant to environmental influences. When the rod enters a child’s body, it releases an exotoxin, which is highly damaging. The course of the disease is lightning fast and very fast. The increase in symptoms occurs instantly, and mortality rates are very high.
Treatment of tetanus is carried out inpatient conditions in intensive care wards. Muscle relaxants are prescribed to relieve seizures. Quite often, patients are transferred to artificial ventilation. The pH level of the blood is adjusted with medication, and support for the functioning of the cardiovascular, excretory and respiratory systems is also required. To prevent secondary infection, antibacterial therapy is carried out.
Parents must clearly understand that even modern medicine is not able to cope with the disease in all cases. Mortality rates remain quite high. The only correct solution is vaccination against tetanus.
The causative agent of the disease
The causative agent of tetanus is Clostridium tetani, a mobile, gram-positive rod that can only exist in anaerobic conditions (without access to oxygen). Clostridia form spores under unfavorable conditions for its life, which retain their viability for many years. Tetanus bacteria are killed by long-term (3–6 hours) treatment with antiseptics and disinfectants.
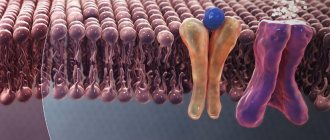
Clostridia themselves do not pose a danger to the body; the effect on the body, in particular on the nervous system, is exerted by the toxins they produce: tetanospasmin and tetanolysin. Tetanospasmin is introduced into the processes of neurons and enters the central nervous system, where it suppresses inhibitory signals, which provokes the development of tetanic convulsions. Tetanolysin destroys red blood cells, the membranes of the heart bag and its tissue, which leads to local necrosis.
The infectious agent normally lives in the intestines of humans, herbivores, birds and rodents. With feces, the tetanus bacillus enters the environment (soil, water bodies, rooms, where it penetrates with dust).
Transmission path
You can become infected with tetanus only through contact when injured skin and mucous membranes come into contact with dirt, dust, rust or water from open reservoirs. But the wound must be deep enough to allow anaerobic (oxygen-free) conditions to form. In this case, tetanus spores, while in the wound, are transformed into active bacteria. A sick person cannot transmit the infection to a healthy person. But susceptibility to the disease is very high. Those at risk for developing infection include:
- Children 9 years of age and younger (due to high levels of trauma);
- Newborns (violation of asepsis during the process of cutting the umbilical cord);
- Adults with deep wounds.
Warning for the unvaccinated
After all of the above, we can say with complete confidence that a tetanus vaccine is necessary. This is the only way to prevent the disease and all the complications it can bring.
In addition, depending on the dose, the drug will provide immunity against other diseases dangerous to children. The charts, developed by experts, are designed to cover the most prominent risks for each age group.
If in doubt, consult your general practitioner or pediatrician. Experts consider immunization for each case individually, and also warn whether there are any contraindications for delaying or not completing doses.