Stroke is a serious brain disease characterized by circulatory disorders, focal lesions of brain tissue, and death of neurons. A stroke can be hemorrhagic or ischemic. Hemorrhagic stroke is less common than ischemic stroke and is characterized by rupture of blood vessels and hemorrhage in brain tissue. Ischemic stroke is more often diagnosed in older people and is characterized by impaired blood flow in the cerebral arteries and the death of neurons in the area of blood supply to brain tissue by the affected artery. When a stroke develops, the patient requires emergency care: the sooner the patient is admitted to the hospital, the more effective the care provided by doctors will be.
In addition to drug treatment of stroke, great importance is attached to rehabilitation therapy, which begins to be carried out in the acute period of the disease. At the Yusupov Hospital, various methods of physiotherapy and exercise therapy are used to restore patients after a heart attack and stroke. With the help of a comprehensive rehabilitation program, the patient is rehabilitated - restoration of motor activity, coordination of movements, visual function, sensitivity. The neurorehabilitation department of the hospital is equipped with modern devices, verticalizers and various simulators, including robotic ones.
The influence of exercise therapy on the patient’s nervous system
Therapeutic exercise is the performance of certain physical exercises, which begin with the simplest movements of the patient after he regains consciousness, then the physical activity gradually increases, the exercises become more complex. Exercise therapy helps improve blood circulation in organs and tissues, accelerates the process of restoration of various body functions, and improves metabolism. Physical therapy exercises for each patient are selected individually depending on the severity of the patient’s condition and concomitant diseases. An individual physical therapy program at the Yusupov Hospital is drawn up by a rehabilitation doctor.
Make an appointment
Etiopathogenesis
The main mechanism for the development of paralysis is stroke - damage to the artery with blood escaping beyond the vascular bed. As a result, a hematoma is formed, which gradually grows and compresses the brain tissue. Vital neurons die, loss of function is noted, control of skeletal and smooth muscles decreases, and sensitivity disappears.
This condition is predisposed to:
- Eating disorders – the main role is played by a lack of calcium in the diet, which strengthens the walls of the arteries. In these cases, cardiologists repeat “where it’s thin, that’s where it breaks.” Weakened brain vessels that are prone to damage can cause a stroke;
- Hypertension – the situation is aggravated by increased blood pressure, which can damage weakened blood vessels. In older people, there is a lack of calcium, which can cause artery rupture;
- Compounded heredity - according to recent studies, there is a predisposition to vascular diseases, especially hypertension and strokes. The mechanism has not been fully studied; insufficiency of the neurohumoral mechanism and weakness of the vascular wall are assumed;
- Obesity - this condition is accompanied by a lack of minerals, an increase in blood pressure, which increases the likelihood of developing a stroke with subsequent paralysis;
- Cardiovascular diseases - valve malformations, heart failure, atherosclerosis and thrombosis predispose to cerebral hemorrhage;
- Endocrine diseases - diabetes comes first, leading to hypertension and hemorrhages. Sometimes the causes are hypothyroidism, pathologies of the adrenal cortex;
- Bad habits - nicotine weakens the walls of arteries and increases cholesterol levels in the blood. Natural alcohol in minimal dosages is useful, but an excess of surrogate or drunkenness often ends in stroke and paralysis.
The listed factors can provoke both left and right paralysis. According to statistics, the latter option is observed more often, which increases the patient’s chances of survival due to timely diagnosis.
Passive and active rehabilitation after stroke
The first classes with the patient are conducted by a physical therapy instructor in the ward. The patient performs simple movements with his arms and legs with the help of an instructor - this type of rehabilitation is called passive. Passive rehabilitation of the upper and lower extremities begins with the development of large joints with a gradual transition to small joints. Rehabilitation therapy begins with the shoulder and hip joints. After developing the hip joint, the instructor helps the patient flex and extend the lower limb, develops the knee, then the ankle joint, and lastly the doctor develops the joints of the foot.
The rehabilitation specialist performs massage from the foot to the thigh. During hand rehabilitation, exercises begin with the development of the shoulder joint, then flexion-extension and rotational movements of the hands are carried out in the area of the elbow and hand joints. Massage of the upper limbs is performed from the fingers to the shoulder. A set of exercises combined with massage stimulates brain function. With partial restoration of motor function, exercise therapy exercises become more complex, and the patient begins to perform the exercises independently. The time for gymnastics increases from 10 minutes to half an hour, and active rehabilitation of the patient begins.
If the brain damage is significant, the patient is paralyzed, sensitivity is lost, rehabilitation is carried out with the help of medication, massage, electromagnetic stimulation of nerve cells, acupuncture, and reflexology. After partial restoration of motor function, the rehabilitation doctor introduces therapeutic exercises into the program.
Rehabilitation exercises on simulators
The Yusupov Hospital uses two types of simulators for the rehabilitation of patients after a stroke - mechanical and robotic. Mechanical exercise machines include exercise bikes, treadmills, and exercise machines for restoring balance and gait. Robotic simulators are equipped with electronic biosensors that stimulate activity by influencing the affected limbs. Robotic simulators have wide functionality; they are programmed taking into account the patient’s needs, promote the transmission of nerve impulses from the brain to the injured limb, and stimulate motor activity.
Rehabilitation exercises after a stroke are performed using multifunctional exercise equipment and sports equipment. There are different types of simulators:
- To restore motor activity, use a flexion/extension simulator, a simulator for developing the joints of the limbs, exercise tracks, and exercise bikes.
- For bedridden patients, exercise equipment in the form of a bed or bicycle is used.
- To restore balance, gait, and motor activity, a horizontal simulator is used.
- For patients who cannot yet stand, a seated exercise machine has been created to develop and strengthen the back muscles.
Hand exercises for stroke rehabilitation
Hand exercises improve motor activity and help restore lost functions. In severe cases and in the absence of early rehabilitation, hand functions are often not restored or partially restored. In some cases, rehabilitation does not help; doctors carry out bipolar stimulation - an effect on immobile joints and muscles of the body using artificially created impulses from the brain to the body. This helps restore reflexes and sensitivity, improve blood circulation in the tissues. Then the patient undergoes rehabilitation using exercise therapy and other methods.
The motor activity of the hands and the motor skills of the fingers are most difficult to restore. You can often see trembling hands in a patient after a stroke; he cannot hold a ballpoint pen in his hand, cannot write, and does not grasp objects well. Especially for such patients, they conduct classes in modeling from plasticine, with a Rubik's cube, teach them to write again, and work on a silicone simulator. Doctors use reflexology if a patient has suffered a severe stroke. This helps restore fine motor skills, improve grasping movements, flexion and extension of fingers, and joints of the hand. At the Yusupov Hospital, patients undergo rehabilitation on computerized simulators using a comprehensive recovery program, which includes massage and physical therapy exercises.
Hand exercises are not complicated and do not require special exercise equipment or devices; the patient can perform them at home:
- Lie on the bed, move your arms back and grab the headboard. Tighten the muscles of your arms and body, imitating a pull-up. Raise your legs up or stretch them straight.
- Using rotational movements of bent arms, knead the shoulder joint.
- Sit upright on the bed, place your hands behind your back as close to each other as possible, tilt your head back, then return to your previous position.
Signs of memory impairment
A patient who has suffered a stroke usually faces difficulties in self-identification and other difficulties:
- Memories from childhood, adolescence or any other period of life disappear. He may not remember people he has ever encountered, certain significant situations and events.
- Loss of motor skills and loss of coordination. It’s as if the body is returning to childhood: it doesn’t remember how to eat, take care of itself in terms of hygiene, and learns everything all over again.
At the same time, there are situations when the victim remembers everything related to his profession down to the smallest detail. For example, he knows how to drive a car, knows musical notation, remembers how he wrote his dissertation, etc. - but does not have the skills of banal household self-service.
Sometimes amnesia is not immediately noticeable and appears much later in the process of secondary complications after a stroke.
When the disease occurs, the patient’s psyche also suffers: the person does not remember the people who communicate with him. Does not understand the purpose of certain items. Can’t remember professional skills – feels extremely uncomfortable. The victim may become depressed or be in a state of increased anxiety, which negatively affects the rehabilitation process and sometimes leads to psycho-emotional breakdowns.
For the shoulder joint
Restoration of the forearm and shoulder joint takes place with the help of flexion and extension exercises, rotation, push-ups, muscle tension and relaxation, clapping, and massage. To do this, use exercise machines, dumbbells, and various devices. First, the arm is kneaded, then a set of exercises is performed; therapeutic exercises are always combined with a massage of the limbs. A set of exercises for the shoulder joint:
- The patient lies on his back, arms extended along the body. The instructor holds his hand at the elbow to avoid bending, takes the patient's palm with his other hand and moves the patient's arm up and down.
- The instructor performs circular movements with the patient's arm fixed in a straightened state.
- The patient lies on his back, with his arm slightly to the side. The instructor turns the straightened arm over, palm down, then up.
For lower limbs
Exercises for the lower extremities begin to be performed as soon as the patient regains consciousness. At the initial stage, the instructor helps to bend and straighten the lower limbs; over time, the patient will be able to imitate walking in a prone position, then get out of bed, learn to maintain balance, and walk without support. Exercises for patients in the supine position:
- The patient is in a supine position, the leg is straightened. The instructor turns the leg with the foot inward, then outward.
- The patient is in a supine position, the leg is bent at the knee. Holding one hand under the knee, the instructor performs circular movements with the limb, holding and pressing with the other hand in the hip joint area.
- The patient is in a supine position, the affected leg is bent at the knee. The instructor fixes the leg at a right angle, holding it with the other hand under the knee, bends and straightens the lower limb.
- The patient is in the same position on his back, with the leg fixed at a right angle. The instructor, holding the patient's leg under the knee, moves it away from the body and returns it back.
These exercises are performed by the patient after he is allowed to sit:
- In a half-sitting position, holding the edges of the bed with both hands, stretch both legs forward as evenly as possible, bend over, throwing your head back. While stretching your limbs, take a deep breath, return to your previous position and exhale.
- Remain in the same body position, keep your breathing calm and deep, slowly lift your right leg up and lower it back, then your left leg.
- In a half-sitting position, bend your leg, pull your bent leg at the knee as close to your chest as possible (you can help with your hands), and tilt your head forward during the exercise. Bending the leg, inhale, straightening the limb, exhale, return to the previous position.
Exercise therapy to restore visual function after stroke
At the Yusupov Hospital, patients with visual impairments will be able to undergo examination, treatment, rehabilitation, and, if necessary, surgical treatment in a network of partner clinics. Rehabilitation after a stroke includes exercises that you can then do at home. Depending on the type of visual impairment, rehabilitation therapy is carried out:
- If lateral vision is impaired, intensive medical and restorative treatment is carried out, undamaged areas of the cerebral cortex take over the lost function, and vision is restored. In this case, the doctor marks with a red line a passage of text on the page of the book on the side of which lateral vision is weakened. Before starting to read, the patient must look for the red line - this will be the beginning of the text.
- With oculomotor nerve palsy, the patient cannot look straight and his eyes look in different directions. Such a disorder can resolve over time with proper and timely treatment and rehabilitation. With paresis of the oculomotor nerve, accommodation may be impaired. Over time, the patient gets used to using only central vision. To determine the impairment of perception of objects at far and near distances, the following test is performed: the doctor takes a pencil in each hand and brings one of the pencils closer to the patient’s face, then moves his hand back.
- If atrophy of the oculomotor nerve develops, the patient's function of the upper eyelid muscle is impaired. Nystagmus or trembling of the eyeballs may occur. Often this condition leads to visual impairment.
To restore vision, the doctor asks the patient to draw the other half of an object in a drawing or take part in a certain type of computer game. The patient is asked to follow with his gaze the pencil in the doctor’s hand, which moves in front of the patient’s face to the right, then to the left, up or down. The patient should follow the pencil without turning his head. To improve blood circulation, eye massage is necessary and beneficial. The eyes are closed, with gentle movements in a circle the patient massages the eyeballs, lightly pressing on them. The exercise should be performed for 10-20 seconds.
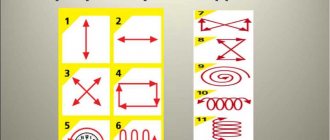
To restore visual function, a number of eye exercises are performed:
- Rotate the eye to the right, then to the left - repeat several times.
- Look up, then down - repeat the movement several times.
- Movement of the eyes in a circle - to the right, then to the left.
- Take a short break with your eyes closed, open your eyes and blink frequently for a few seconds.
- Close your eyes tightly and relax - repeat several times.
- Fix your eye on the object, then turn your head to the right and left without taking your eyes off the object - do this several times.
Recommendations from physiotherapists
After a stroke, life changes not only for the victim, but also for those close to him. You need to understand that there is a long rehabilitation ahead, which can last for several years. This is why rehabilitation exercises after a stroke are so important. Many people use methods recommended by their doctor. Recommendations from specialists in this direction will not hurt, among whom Bubnovsky’s technique receives special attention.
The main direction of rehabilitation therapy of this doctor is kinesitherapy - restoration through movement. He, like other doctors, argues that it is important to begin the method he developed immediately after severe symptoms have been relieved. Initially, this is passive therapy with the help of assistants. Later, patients begin to perform exercises themselves using exercise machines.
Restoring fine motor skills after stroke
Fine motor skills are restored with the help of simple exercises that allow you to restore fine hand movements and finger flexibility. The most effective activities for restoring fine motor skills are putting together puzzles, various objects from small parts of a construction set, drawing, fastening buttons on clothes, and lacing shoes. To restore the function of the hand and fingers, the patient is asked to take two nuts in his hand and roll them with the movement of the palm and fingers. Recommended for patients after a stroke to develop fine motor skills:
- Sort through the beans and peas, separating the peas from the beans.
- Use special silicone hand trainers with spikes to massage your palms and fingers.
- Tighten and unscrew nuts, close and open the lock with a key, turn on and off the lights in the room, write texts.
Restoring speech after a stroke
Speech function after a stroke is restored much worse than motor function. Its recovery can take a long time, over several years. Speech therapists at the Yusupov Hospital are developing a program and working with the patient to restore speech throughout the entire period of his stay in the hospital; after discharge from the hospital, his relatives are involved in the patient’s rehabilitation. To restore speech, the following techniques are used:
- Pronunciation of an incomplete word - the patient must complete the word independently.
- If speech function is completely lost, rehabilitation begins with the pronunciation of individual sounds.
- When the patient learns to pronounce words, he is forced to repeat short poems and sayings.
- Singing is considered one of the best methods of speech restoration.
- In order for the patient to learn to speak faster, the facial muscles and tongue muscles should be trained. For this purpose, the patient is taught to curl his lips into a tube, stick his tongue out of his mouth as far as possible, and lick his lips with his tongue, first in one direction, then in the other. Lightly bite your lower lip, then your upper lip, and bare your teeth.
Make an appointment
How to help yourself
Contrary to popular belief, it is strictly forbidden to independently engage in exercise therapy after a stroke at home, even if the illness experienced is characterized by the absence of negative symptoms. At the first stage, the patient in any case requires outside help - from medical workers or relatives.
At this time, close people should make sure that the patient does not dwell on negative thoughts and focuses on the correct implementation of exercise therapy after a stroke. In addition to physical therapy, one must remember to take prescribed medications, physiotherapy and massage in a timely manner.
For help, you can always contact our boarding house for the elderly and we will help you
Rehabilitation of the patient at home
Before the patient is discharged from the hospital, relatives receive recommendations on caring for the patient after a stroke. Recommendations for rehabilitation will be provided by the attending physician. The rehabilitation exercise program is performed every day without breaks, 2-3 times a day. Performing physical exercises should not tire the patient or cause him pain. Exercises in a sitting position help prepare the patient for walking.
When the condition improves, exercises are performed in a standing position; they help eliminate neurological disorders as much as possible by restoring fine movements. The patient performs exercises with an expander. From a standing position, he bends down and picks up a matchbox from the floor. Performs breathing exercises with raising your arms up while inhaling, standing on your toes, then lowering yourself onto your entire foot, lowering your arms, exhaling, leaning forward. A comprehensive recovery program is aimed at reducing muscle tone, improving blood circulation, preventing joint contracture, restoring and maintaining fine motor skills, speech, preventing the formation of bedsores and the development of inflammatory processes.
The Yusupov Hospital uses modern rehabilitation methods, uses various types of exercise equipment, and physical therapy exercises. Rehabilitation doctors develop an individual rehabilitation program for each patient.
Contraindications
Limitations in rehabilitation depend on the patient's condition. Physical activity is not indicated in the following cases:
- the patient did not recover from the coma;
- mental changes in behavior and aggressiveness are observed;
- repeated stroke in an elderly person;
- there are symptoms of epileptiform seizures, cramps in the limbs;
- Stroke is accompanied by severe diabetes mellitus, tuberculosis, and cancer.
An important point in physical therapy is the patient’s comfortable state of health. The appearance of headaches and weakness requires control of blood pressure, rest, and a slower rate of increase in load.
After gaining the opportunity to walk, it is necessary to use walks in the air with a gradual lengthening of the route. Confidence in one’s abilities and the support of loved ones allows the patient to take stroke therapy as beneficially as possible and strive for a full recovery.