pharmachologic effect
Fast-acting diuretic. The active component is a sulfonamide . The principle of action is based on the ability of furosemide to block the transport system of potassium, sodium and chlorine ions in the thick segment in the ascending limb of the loop of Henle. The severity of the saluretic effect directly depends on the entry of the active substance into the renal tubules (anion transport). The diuretic effect is achieved by inhibiting the process of NaCl reabsorption in the loop of Henle.
Secondary effects of the drug
- increased potassium production in the distal renal tubule;
- an increase in the volume of urine excreted (due to osmotically bound water);
- increased excretion of Mg and Ca ions.
Repeated use of the medication does not lead to a decrease in the severity of its effect, because furosemide is able to interrupt the tubular-glomerular feedback in the tubular structure, which is tightly connected to the juxtaglomerular apparatus (Macula densa). The drug is characterized by dose-dependent stimulation of the renin-angiotensin-aldosterone system.
In patients with heart failure, furosemide is able to quickly reduce filling pressure in the left ventricle and pulmonary artery and reduce preload , which is achieved by expanding the venous lumen. This rapidly developing effect is mediated by the action of prostaglandins , so its severity depends on the preservation of the functional state of the renal system and the synthesis of prostaglandins.
The hypotensive effect is due to a decrease in circulating blood volume, an increase in Na excretion, and a decrease in the response of vascular smooth muscle tissue to vasoconstrictor effects. The natriuretic effect makes it possible to reduce the reaction of vessel walls to catecholamines, the level of which is increased in patients with hypertension .
Dose-dependent natriuresis and diuresis are recorded when taking the drug at a dose of 10-100 mg. The diuretic effect develops within 50 minutes after intravenous administration of 20 mg of furosemide and can last up to 3 hours. The relationship between the intratubular concentration of free (unbound) furosemide and the severity of the natriuretic effect is expressed by a sigmoidal curve with a minimum effective rate of elimination of the active substance of approximately 10 mcg/min. That is why long-term infusion of the drug is considered more effective than bolus re-infusion. No significant increase in effect was observed with increasing bolus dosage. The effect of the active substance is reduced when Lasix binds to albumin in the tubular lumen (with nephrotic syndrome) and when the rate of tubular secretion decreases.
Pharmacological properties of the drug Lasix
Furosemide (4-chloro-N-(2-furylmethyl)-5-sulfamoylanthranilic acid) is a fast-acting diuretic, a sulfonamide derivative. The mechanism of action of Lasix is due to the blockade of reabsorption of chlorine and sodium ions in the ascending limb of the loop of Henle. To a lesser extent, the drug also affects the convoluted tubules, and this effect is not associated with inhibition of carbonic anhydrase or antialdosterone activity. Lasix has a pronounced diuretic, natriuretic, chloruretic effect. Increases the excretion of potassium, calcium, magnesium. When administered intravenously, it quickly reduces preload on the heart, left ventricular filling pressure and pulmonary artery pressure. Reduces systemic blood pressure. When taking the drug orally, the diuretic effect is noted within 1 hour, and the maximum effect is achieved within 1–2 hours after administration; the duration of the diuretic effect is 6–8 hours. With intravenous administration, the onset and maximum diuretic effect are observed respectively 5 and 30 minutes after administration, and its duration is about 2 hours. When taken orally, the bioavailability of Lasix is 64%. The maximum concentration of the drug in the blood plasma increases with increasing dose, but the time to reach the maximum does not depend on the dose and varies widely depending on the patient's condition. The half-life is about 2 hours. After intravenous administration, the amount of Lasix excreted in the urine is significantly greater than after oral administration. In blood plasma, the drug is mainly bound to protein, mainly albumin: in the concentration range from 1 to 400 ng/ml, protein binding in healthy individuals is 91–99%. The free fraction is 2.5–4.1% of the therapeutic concentration. During the biotransformation process, the drug in the body is converted mainly into glucuronide.
Pharmacodynamics and pharmacokinetics
The distribution index of furosemide is 0.1-0.2 l/kg body weight and may vary depending on concomitant pathology and the underlying disease. The active substance binds quite strongly to plasma proteins (the figure reaches 98%), mainly to albumin. The active component is excreted through the renal system (proximal tubules) mainly unchanged. When given intravenously, 60-70% of Lasix is excreted through the kidneys. Glucuronidated metabolites account for about 10-20% (the route of elimination is through the renal system). The remaining metabolites are excreted by biliary secretion through the intestines. After intravenous infusion, the terminal half-life is 1-1.5 hours.
The active component is able to penetrate into breast milk and pass through the placental barrier. The concentration of the active substance in the blood of a newborn baby (fetus) is the same as that of the mother.
Pharmacokinetics of certain patient groups
In patients with renal failure, the excretion of the active substance slows down, while the half-life increases (up to 24 hours with severe pathology).
In patients with nephrotic syndrome, a decrease in plasma protein concentrations leads to an increase in the level of unbound furosemide (free fraction), which can lead to ototoxic manifestations . Moreover, in this group of patients, the diuretic effect may be weakly expressed due to the ability of the active substance to bind to albumin, which is located in the tubules.
With continuous outpatient peritoneal dialysis and hemodialysis , the active substance is excreted in small quantities.
If the hepatic system is insufficient, the half-life increases by 30-90% due to an increase in the volume of distribution. In this group of patients, pharmacokinetic parameters vary quite significantly.
A slowdown in the excretion of the active substance is recorded (due to deterioration of the functional state of the kidneys) in severe arterial hypertension , heart failure and in the elderly.
In premature babies, the process of excretion of the active substance may slow down (the rate of excretion depends on the maturity of the renal system). A similar effect is observed in infants, because The glucurinating function of the kidneys is not fully developed.
Special instructions for the use of Lasix
When using the drug, concentration of attention may decrease, which is important for people driving vehicles and working with potentially dangerous mechanisms, especially at the beginning of treatment and while consuming alcohol. During the period of use of the drug, it may be necessary to replenish potassium loss. Since the drug can penetrate the placental barrier, Lasix can be used during pregnancy only under strict indications and for a short period of time. Since the drug can pass into breast milk and also suppress lactation, use should be discontinued during breastfeeding.
Indications for use of Lasix
The medication is used mainly for edema syndrome .
What are the tablets, solution and main indications for using Lasix:
- cerebral edema;
- edema syndrome in chronic pathology of the renal system ;
- edema syndrome in heart failure (acute form);
- edema syndrome in chronic heart failure ;
- hypertensive crisis;
- edema syndrome due to pathology of the hepatic system (in combination with aldosterone antagonists);
- acute renal failure during burns (maintaining fluid excretion), during pregnancy ;
- edema syndrome in nephrotic syndrome (together with therapy of the underlying disease);
- support for forced diuresis during intoxication with a chemical compound that is excreted unchanged through the renal system.
Contraindications
- severe hyponatremia ;
- hepatic precoma , coma ;
- renal failure with anuria , which does not respond to the administration of Lasix;
- severe hypokalemia ;
- allergic responses;
- breast-feeding;
- pronounced impairment of urinary outflow in any pathology (including unilateral damage to the urinary tract);
- pregnancy.
Relative contraindications:
- gout;
- arterial hypotension;
- myocardial infarction , acute stage (increased risk of developing cardiogenic shock);
- stenosing damage to the cerebral, coronary arteries and other conditions in which excessively reduced blood pressure is extremely dangerous;
- hepatorenal syndrome;
- diabetes mellitus (latent, manifested);
- hearing loss;
- hypoproteinemia;
- diarrhea syndrome;
- pancreatitis;
- disturbance of urinary outflow ( hydronephrosis , narrowing of the urethra, prostatic hyperplasia);
- systemic lupus erythematosus;
- ventricular arrhythmia.
The medicine is not prescribed to premature infants due to the risk of deposition of Ca salts in the renal parenchyma ( nephrocalcinosis ), due to the possibility of the formation of calcium-containing stones in the renal system ( nephrolithiasis ).
Side effects
Peripheral blood:
- aplastic anemia;
- eosinophilia;
- thrombocytopenia;
- hemolytic anemia;
- leukopenia;
- agranulocytosis.
Allergic responses, skin reactions:
- anaphylactoid reactions;
- exfoliative dermatitis;
- erythema multiforme;
- vasculitis;
- hives;
- purpura;
- photosensitivity;
- fever;
- bullous lesions of the skin;
- anaphylactic shock.
Hearing organs, central nervous system:
- headache;
- hearing impairment, tinnitus (in patients with hypoproteinemia , nephrotic syndrome );
- drowsiness;
- severe weakness;
- blurred visual perception;
- dizziness;
- paresthesia.
Digestive tract:
- acute pancreatitis;
- intrahepatic cholestasis;
- diarrhea syndrome;
- vomit;
- increased levels of AST, ALT;
- nausea.
Urinary tract:
- interstitial nephritis;
- deterioration of health with partial narrowing of the urinary tract (for example, with prostate hyperplasia);
- nephrolithiasis/nephrocalcinosis in premature infants.
Metabolism:
- decreased glucose tolerance (manifestation of latent diabetes mellitus is rarely recorded);
- increased triglycerides and serum cholesterol;
- increase in urea, creatinine (temporary, reversible changes);
- an increase in uric acid levels, and as a result, an increase in the manifestations of gout.
The cardiovascular system:
- a sharp drop in blood pressure ;
- arrhythmias;
- tachycardia;
- decrease in circulating blood volume;
- collapse;
- violation of orthostatic regulation of blood circulation.
Acid-base, water-electrolyte balance:
- metabolic alkalosis;
- hypokalemia;
- hypochloremia;
- hypovolemia;
- hyponatremia;
- dehydration;
- hypercalcemia.
Other reactions:
- pain at the injection site;
- muscle weakness, cramps;
- high risk of preservation of the Botallian duct in premature infants.
Side effects of Lasix
With long-term use or administration of the drug in high doses - hypovolemia, dehydration, hemoconcentration with a tendency to thrombosis (especially in the elderly), hypokalemia, hyponatremia, hypochloremia, alkalosis, in some cases - hypocalcemia; arterial hypotension, systemic circulatory disorders (especially in children and the elderly); deterioration of the condition due to obstructive uropathy (prostatic hyperplasia, narrowing of the ureter, hydronephrosis); increased levels of cholesterol and TG in the blood plasma; transient hyperuricemia (with exacerbation of gout), increased creatinine levels; hyperglycemia, especially in patients with diabetes; increased severity of metabolic alkalosis; nausea, vomiting, diarrhea; allergic skin reactions (itching, polymorphic erythema, exfoliative dermatitis, purpura), fever, extremely rarely - anaphylactic shock; extremely rarely - vasculitis, interstitial nephritis; changes in the composition of peripheral blood - eosinophilia, aplastic or hemolytic anemia, leukopenia or agranulocytosis, thrombocytopenia with a tendency to bleeding; In premature newborns with respiratory distress syndrome, the use of furosemide during the first weeks of life increases the risk of patent ductus arteriosus.
Instructions for use of Lasix (Method and dosage)
Lasix tablets, instructions for use
It is recommended to start treatment with the lowest dosages that can give the necessary therapeutic effect. The dosage is calculated individually, taking into account concomitant pathology, the patient’s weight, and the severity of the edema syndrome.
The manufacturer's recommended route of administration is intravenous. Intramuscular administration is possible when it is not possible to take the medicine orally (including when the absorption of the active substance from the lumen of the small intestine is impaired) or to carry out intravenous infusions. When administered intravenously, it is recommended to transfer the patient to the tablet form of Lasix as soon as possible.
Lasix ampoules, instructions for use
Intravenous infusions are carried out slowly (the rate of administration is no more than 4 mg per minute). In cases of severe pathology of the renal system (creatinine level more than 5 mg/dL), intravenous infusion can be administered at a rate of no more than 2.5 mg per minute. Long-term intravenous infusion of the drug allows you to achieve optimal effectiveness and suppress the process of counter-regulation (activation of neurohumoral antinatriuretic regulation links and the renin-angiotensin system). If, in acute conditions, after intravenous bolus injections it is not possible to carry out a stable continuous intravenous infusion, then preference is given to frequent injections of small doses in comparison with bolus intravenous infusions of high doses over long time intervals.
The solution does not have buffering properties and its pH is 9. Precipitation of the active component is observed at a pH value less than 7. Saline solution can be used for dilution. Freshly prepared solution is not intended for long-term storage. The maximum daily dosage for adults when administered intravenously is 1500 mg. For children, the dose is calculated according to the scheme - 1 mg per 1 kg of weight, but not more than 20 mg per day. The duration of therapy is determined individually.
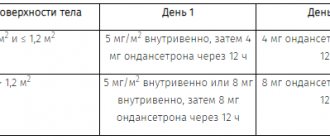
Treatment of edema syndrome arising from chronic heart failure
The recommended dosage varies in the range of 20-80 mg. Depending on the severity of the diuretic effect, an individual dose is selected. It is recommended to split the daily dosage into 2-3 doses.
Treatment of edema syndrome in acute heart failure
20-40 mg of furosemide is administered intravenously as a bolus. Depending on the therapeutic effect, the dosage regimen is adjusted.
Treatment of swelling in chronic renal failure
The severity of the natriuretic effect depends on the Na content in the blood and the functioning of the renal system. Careful selection of dosage with a gradual increase is required to achieve a stable effect on fluid loss, because at the beginning of therapy, due to the diuretic effect, up to 2 kg of weight per day can be lost. The maintenance dose of furosemide for patients on hemodialysis is 250-1500 mg per day.
Dose selection scheme for intravenous infusion: initially the solution is administered dropwise at a rate of 0.1 mg/min, then the rate is increased every half hour, assessing the severity of the therapeutic effect.
Removal of fluid from the body in acute renal failure
It is imperative to eliminate hypovolemia, acid-base and electrolyte imbalance, and arterial hypotension before starting therapy. The manufacturer recommends switching from the injection form of the drug to the tablet form as early as possible. The initial dosage for intravenous administration is 40 mg. In the absence of the expected effect, intravenous continuous infusion therapy is carried out at a rate of 50-100 mg/hour.
Swelling in nephrotic syndrome
The initial dosage recommended by the manufacturer is 20-40 mg per day. Assessing the diuretic effect, select the required dose of the medication.
Swelling due to pathology of the hepatic system
If aldosterone antagonists are insufficiently effective, Lasix is prescribed. If the dose is selected incorrectly, complications such as:
- electrolyte imbalance ;
- violation of orthostatic regulation of blood circulation;
- violation of the acid-base state .
If it is necessary to administer Lasix intravenously, then treatment begins with small doses - 20-40 mg.
Swelling of the brain, hypertensive crisis
Therapy begins with a bolus injection of Lasix intravenously at a dose of 20-40 mg. The correction is carried out taking into account the observed and expected effect.
Support of forced diuresis during intoxication, poisoning
After an intravenous infusion of electrolyte solutions, the diuretic Lasix can be gradually introduced, starting with 20-40 mg. Monitoring of electrolytes and the level of lost fluid is mandatory.
Lasix 20 mg/2 ml No. 10 solution for intramuscular and intravenous administration
Instructions for medical use of the drug Lasix® Trade name Lasix® International nonproprietary name Furosemide Dosage form Solution for intravenous and intramuscular administration 10 mg/ml Composition 1 ml of solution contains the active substance - furosemide 10 mg, excipients: sodium chloride, sodium hydroxide, water for injection. Description Transparent, colorless solution. Pharmacotherapeutic group “Loop” diuretics. Sulfonamide diuretics. ATC code C03CA01 Pharmacological properties Pharmacokinetics The volume of distribution of furosemide is 0.1 - 0.2 liters per 1 kg of body weight. The volume of distribution may be higher depending on the patient's disease. Communication with blood plasma proteins is 98%, mainly with albumin. Furosemide is excreted from the body mainly unchanged, mainly through the proximal tubules of the kidneys. After intravenous administration, 60%-70% of furosemide is eliminated in this way. Glucuronide - a metabolite of furosemide from 10% to 20% is found in the urine in a reduced form. The remaining dose is excreted in the feces, probably due to the secretion of bile. The half-life of furosemide after intravenous administration is 1 to 1.5 hours. Furosemide is excreted into breast milk. Furosemide passes the placental barrier and slowly enters the fetus. It is found in the fetus or in the body of newborns in the same concentrations as in the mother's body. Pharmacodynamics Lasix is a highly effective, rapidly and short-acting “loop” diuretic. Blocks the Na+K+2Cl–transport system located in the luminal cell membrane of the ascending loop of Henle. Therefore, the effectiveness of the diuretic action of Lasix depends on the drug reaching the level of the renal tubules through the anion transport mechanism. The diuretic effect is caused by suppression of the reabsorption of chloride and sodium ions in this segment of the loop of Henle. As a result, partial sodium excretion can reach 35% of glomerular sodium filtration. The consequence of increased sodium secretion is increased urine output (as a result of osmotically bound water) and increased secretion of potassium ions in the distal part of the renal tubules. The release of calcium and magnesium also increases. Lasix interrupts the tubular-glomerular feedback mechanism in the macula densa, as a result of which the diuretic effect is not weakened. Lasix leads to dose-dependent stimulation of the renin-angiotensin-aldosterone system. In heart failure, Lasix causes a rapid reduction in afterload (by dilating the venous vessels). This early vascular effect is mediated through stimulation of prostaglandins, resulting in increased renal blood flow with activation of the renin-angiotensin system. Moreover, due to its natriuretic effect, Lasix reduces the sensitivity of the vascular wall to catecholamines, which is increased in patients with arterial hypertension. The antihypertensive effect of Lasix is based on an increase in sodium excretion, a decrease in blood volume, and a decrease in the response of vascular smooth muscle to vasoconstrictor stimuli. When administered intravenously at a dose of 20 mg, the onset of the diuretic effect is observed after 15 minutes and lasts about 3 hours. A continuous infusion of Lasix is more effective than repeated injections of a loading dose of the drug. The important thing is that doses above a certain loading dose of the drug do not have a significant effect. The effect of Lasix is reduced in patients with reduced tubular secretion or when the drug is intratubularly bound to proteins. Indications for use: edema syndrome in chronic congestive heart failure (if treatment with diuretics is required) - edema syndrome in acute congestive heart failure - edema syndrome in chronic renal failure - maintaining fluid secretion in acute renal failure, including during pregnancy and childbirth - edema caused by nephrotic syndrome (if treatment with diuretics is required) - edema syndrome in liver diseases (if additional treatment with aldosterone antagonists is necessary) - arterial hypertension - hypertensive crisis (as maintenance therapy) - maintenance of forced diuresis Method of administration and dosage It is recommended to use the most effective lowest dose drug. For intravenous and intramuscular administration. The intravenous route of administration of Lasix is used only when the oral route is not possible or ineffective (for example, impaired intestinal absorption), or if a rapid effect is required. The transition from parenteral to oral form should be made as early as possible. To achieve optimal effectiveness and suppression of counterregulation, continued Lasix injections in the form of repeated bolus injections are recommended. If continuation of Lasix injections is not possible, for further treatment after one or more acute doses administered as a bolus, the subsequent regimen should be continued with low doses at short intervals (approximately 4 hours). This is preferable to treatment with large bolus doses at long intervals. For adults, the recommended maximum daily dose is 1500 mg. For children, the recommended dose is 2 mg/kg body weight, the maximum daily dose is 40 mg. For children, the recommended dose for parenteral administration is 1 mg/kg body weight, the maximum daily dose is 20 mg. The dose for children may be reduced depending on body weight. The duration of treatment depends on the indication and is determined individually by the doctor. Route of administration Intravenous injections/infusions: When administered intravenously, Lasix should be administered slowly and the rate of administration should not exceed 4 mg per minute. In patients with severe renal impairment (serum creatinine >5 mg/dL), it is recommended not to exceed an infusion rate of 2.5 mg per minute. Intramuscular injections are prescribed in exceptional cases when oral or intravenous administration of the drug is not possible. The intramuscular route of administration is not applicable for the treatment of acute conditions, such as pulmonary edema. The following dosages are recommended for adults (doses are indicated for parenteral and oral administration, since in most cases, treatment with Lasix requires a transition from parenteral to oral administration): Edema syndrome in chronic congestive heart failure The recommended initial oral dose is from 20 mg to 80 mg per day. This dose should be divided into 2 or 3 divided doses and adjusted as needed according to clinical response. Edema syndrome in acute congestive heart failure The recommended initial intravenous dose is 20 mg to 40 mg as a bolus injection. The dose should be adjusted as needed according to clinical response. Edema syndrome in chronic renal failure The natriuretic response of Lasix depends on a number of factors, including the severity of renal failure and sodium balance, so the effect of dosage cannot be accurately calculated. For patients with chronic renal failure, the dose of Lasix should be carefully titrated so that the initial loss of fluid is gradual. The dose that leads to fluid loss is approximately equal to 2 kg of body weight (approximately 280 mmol sodium) per day. The recommended initial oral dose is 40 mg to 80 mg per day. The dose should be adjusted as needed according to clinical response. The daily dose should be taken in 1 or 2 doses. For patients on dialysis, the usual maintenance oral dose is 250 mg to 1500 mg per day. For intravenous administration, Lasix is initiated by continuous intravenous infusion at a dose of 0.1 mg per minute, then gradually increasing the rate of administration every half hour based on clinical response. Maintaining fluid excretion in acute renal failure Hypovolemia, hypotension, severe electrolyte and acid-base imbalances should be corrected before starting treatment with Lasix. The recommended switch from intravenous to oral administration of Lasix should be made as soon as possible. The recommended starting dose for intravenous administration is 40 mg. If this dosage does not produce the desired fluid output, intravenous Lasix can be continued, starting from 50 mg to 100 mg every hour. Edema due to nephrotic syndrome The recommended initial oral dose is 40 mg to 80 mg per day. The dose should be adjusted as needed according to clinical response. The daily dose should be taken in one or more doses. Edema syndrome in liver diseases Lasix is used as an additional therapy with aldosterone antagonists in cases where antagonists alone are not enough. To avoid complications such as orthostatic reaction or electrolyte and acid-base imbalances, the dose should be carefully titrated so that the initial loss of fluid is gradual. The dose that leads to fluid loss is approximately 0.5 kg of body weight per day. The recommended initial oral dose is 20 mg to 80 mg per day. The dose should be adjusted as needed according to clinical response. The daily dose should be taken in one or more doses. If intravenous administration is necessary, the initial single dose is from 20 mg to 40 mg. Hypertension Lasix can be used alone or in combination with other antihypertensive drugs. The usual maintenance oral dose is 20 mg to 40 mg per day. In case of arterial hypertension associated with chronic renal failure, an increase in dose may be required. Hypertensive crisis The recommended starting dose for intravenous administration is 20 mg to 40 mg. The dose should be adjusted as needed according to clinical response. Maintaining forced diuresis during poisoning Intravenous administration of Lasix is recommended as an addition to infusion electrolyte solutions. The dose depends on the response to Lasix. Fluid and electrolyte losses should be corrected before or during therapy. In case of poisoning with acidic or alkaline substances, further removal can be increased by alkalization or oxidation of urine. The recommended intravenous starting dose is 20 to 40 mg. Side effects - electrolyte imbalance: hyponatremia, hypochloremia, hypokalemia, hypomagnesemia and metabolic alkalosis - dehydration and hypovolemia, especially in elderly patients - increased blood creatinine and urea, temporary and reversible - increased serum levels of cholesterol and triglycerides - increased uric acid levels in blood, which can lead to gout attacks - decreased glucose tolerance. In patients suffering from diabetes mellitus, a manifestation of latent diabetes mellitus may occur - a decrease in blood pressure, including orthostatic hypotension - a tendency to develop thrombosis - vasculitis - acute urinary retention in patients with partial obstruction of the urinary tract - interstitial nephritis - possible in premature infants formation of calcium-containing kidney stones (nephrolithiasis) and deposition of calcium salts in the kidney parenchyma (nephrocalcinosis) - nausea, vomiting, diarrhea - acute pancreatitis - intrahepatic cholestasis, increased levels of liver transaminases - hearing impairment and tinnitus, usually reversible especially in patients with renal failure and signs of hypoproteinemia (nephrotic syndrome) and/or after too rapid intravenous administration of Lasix - itching, urticaria, bullous rashes, erythema multimorpha, bullous pemphigoid, exfoliative dermatitis, purpura, photosensitivity - severe anaphylactoid and anaphylactic reactions (shock) - paresthesia - hepatic encephalopathy in patients with hepatocellular insufficiency - thrombocytopenia, leukopenia, eosinophilia, agranulocytosis, aplastic or hemolytic anemia, hemoconcentration - in premature infants during the first weeks of life, furosemide may increase the risk of patent Botallian duct - increased body temperature - pain at the injection site after intramuscular injection Contraindications - hypersensitivity to furosemide or to any of the components of the drug; with hypersensitivity to sulfonamides, antibiotics or sulfonylureas, cross-sensitivity to furosemide may occur - hypovolemia or dehydration - renal failure with anuria not responding to furosemide - severe hypokalemia - severe hyponatremia - hepatic coma and precoma caused by hepatic encephalopathy - breastfeeding period Drugs interactions Not recommended combinations In some cases, intravenous administration of Lasix within 24 hours after taking chloral hydrate can lead to flushing, excessive sweating, anxiety, nausea, increased blood pressure, and tachycardia. Therefore, co-administration of Lasix and chloral hydrate is not recommended. The ototoxicity of aminoglycosides and other ototoxic drugs may be increased by concomitant use of Lasix. Since the resulting hearing impairment may be irreversible, such simultaneous use should be avoided, except in cases where it is necessary for health reasons. Combinations requiring special precautions When using Lasix and cisplatin simultaneously, there may be a risk of ototoxicity. If, during treatment with cisplatin, it is necessary to achieve forced diuresis with the help of Lasix, then the latter can be prescribed only in a low dosage (for example, 40 mg with normal renal function) and in the absence of fluid deficiency. Otherwise, the nephrotoxic effect of cisplatin may be enhanced. Lasix reduces the excretion of lithium, thereby increasing the damaging effects of lithium on the heart and nervous system. Lithium levels should be carefully monitored in patients receiving this combination. Treatment with Lasix can lead to severe hypotension and deterioration of renal function, and in some cases to the development of acute renal failure, especially when prescribing angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor antagonists for the first time or when taking the first dose at an increased dose. It is recommended to discontinue furosemide or reduce the dose of furosemide 3 days before starting treatment with ACE inhibitors or angiotensin II receptor antagonists. Lasix should be used with caution in combination with risperidone. In elderly patients with dementia, mortality is increased when Lasix and risperidone are used together. The need for co-administration must be justified based on the risks and benefits of the combination. In the presence of dehydration in elderly patients with dementia, the risk of mortality is increased with the combination, and the combination of Lasix with risperidone should be avoided in these patients. Combinations to consider Co-administration of non-steroidal anti-inflammatory drugs (NSAIDs), including acetylsalicylic acid, may reduce the effect of Lasix. In patients with dehydration or hypovolemia, NSAIDs may cause acute renal failure. At the same time, the toxic effect of salicylates may increase. A decrease in the effectiveness of Lasix has also been described with simultaneous administration of phenytoin. With simultaneous treatment with glucocorticosteroids, carbenoxolone, licorice in large quantities, and long-term use of laxatives, hypokalemia may increase. Possible hypokalemia or hypomagnesemia may increase the sensitivity of the myocardium to cardiac glycosides and drugs leading to prolongation of the QT interval. The effect of other drugs that lower blood pressure (antihypertensives, diuretics and other drugs) may be enhanced when used simultaneously with Lasix. The simultaneous use of probenecid, methotrexate and other drugs that are eliminated by tubular secretion (like Lasix) may reduce the effectiveness of Lasix. On the other hand, Lasix may result in decreased renal elimination of these drugs. When treated with large doses (Lasix and other drugs), their levels in the blood serum may increase and the risk of side effects may increase. The effectiveness of hypoglycemic agents and pressor amines (for example, epinephrine (adrenaline), norepinephrine (norepinephrine) may be weakened, and theophylline and curare-like drugs may be enhanced. Lasix may enhance the damaging effect on the kidneys of nephrotoxic drugs. In patients simultaneously receiving treatment with Lasix and certain Cephalosporins in high doses are possible to deteriorate renal function. With the simultaneous use of cyclosporine A and Lazix, it is possible to increase the risk of secondary gouty arthritis due to lasix-induced hyperuricemia and the deterioration of the urates with kidneys caused by cyclosporine. Patients with a high risk of radio contract nephropathy, treated with a more lasix, in a larger The degree is subject to impaired renal function after receiving a radio contrast compared to high -risk patients who received only intravenous hydration before obtaining a radio contrast. Special instructions for precautions during Lazix therapy need to control the amount of urine allocated. Particularly carefully monitor patients with impaired urinary outflow (disorder of the bladder, prostatic hypertrophy, urethra narrowing), increased urine formation can cause or strengthen the patient's complaints. Such patients need to conduct careful monitoring of the condition, especially during the start of treatment. When treating with a lasix, it is necessary to conduct a regular medical examination, it is necessary careful observation: - with hypotension - at the risk of a significant decrease in blood pressure, for example, in patients with stenosis of the coronary arteries or arteries of the brain - with latent or manifesting diabetes - with gout - renal. deficiency in combination with a serious liver disease (hepatiental syndrome) - with a decrease in blood protein (hypoproteinemia), for example, with nephrotic syndrome (the effect of lasix therapy can be reduced and an ototoxic effect). A thorough selection of dose is required. - in premature babies (nephrolytiasis/nephrocalcinosis), regular monitoring of the function of the kidneys and ultrasound examination of the kidneys are recommended. During lasix therapy, it is necessary to periodically control the levels of sodium, potassium and creatinine in blood serum. Patients with a high risk of developing disorders of electrolyte metabolism, as well as in cases with additional fluid loss (vomiting, diarrhea, increased sweating) must be carefully observed. Hypovolemia or dehydration, as well as violations in the balance of electrolytes and in an acid-base state, must be adjusted. It is possible a temporary cessation of lasix therapy. Pregnancy and lasix breastfeeding period penetrates through the placental barrier. During pregnancy, Lazix should not be used, with the exception of the necessary cases for medical reasons. Lazix treatment during pregnancy requires careful observation of the fetus. Lazix penetrates breast milk and suppresses lactation. Women should stop breastfeeding during lasix treatment. Features of the effect of the drug on the ability to drive a vehicle or potentially dangerous mechanisms, some side effects, in particular, falling blood pressure, can reduce the ability to concentrate and rapid reaction, which represents a risk to persons driving vehicles and working with potentially dangerous mechanisms. An overdose of the clinical picture of the acute or chronic overdose of the drug depends mainly on the lost volume of fluid and electrolytes: hypovolemia, dehydration, hemoconcentration, heart rhythm (including atrioventricular blockade and ventricular fibrillation). Symptoms of these disorders include a pronounced decrease in blood pressure (up to the development of shock), acute renal failure, thrombosis, delirious states, sluggish paralysis, apathy and confusion of consciousness. Treatment is symptomatic, aimed at limiting and reducing further absorption of the drug, gastric lavage, and the use of activated coal. There is no specific antidote. Clinically important violations of electrolyte and water metabolism must be adjusted. Along with the prevention and treatment of serious violations, as a result of such violations of the correction, the general and specific measures of intensive medical supervision and therapeutic measures should include. The form of release and packaging solution for intravenous and intramuscular administration of 10 mg/ml. 2 ml of the drug into ampoules made of amber -colored glass Type I with a white point (fault line) above the neck. 10 ampoules, along with instructions for medical use in the state and Russian languages, are invested in a cardboard pack. Storage conditions Store in a place protected from light at a temperature not exceeding 25C. Keep out of the reach of children! The shelf life of 3 years after the expiration of the shelf life cannot be used. Conditions of vacation from pharmacies according to the recipe manufacturer Aventis Pharma LTD, India address address: 54/A, Sir Mathuraadas Vasanji Road, Andheri (E), Mumbai 400 093, India address of the organization receiving in the territory of the Republic of Kazakhstan claims from consumers on product quality (goods ) 050016 Almaty, st. Kunaeva 21b Phone: 8-727-244-50-96 Fax: 8-727-258-25-96 E-mail
Overdose
Clinically, acute and chronic overdoses may present differently depending on the level of electrolyte and fluid loss. The most commonly recorded manifestations are:
- dehydration;
- acute renal failure;
- hypovolemia;
- delirium;
- hemoconcentration;
- thrombosis;
- cardiac rhythm and conduction disturbances (ventricular fibrillation, atrioventricular block );
- apathy;
- flaccid paralysis;
- confusion;
- drop in blood pressure.
Therapy is aimed at correcting disturbances in the acid-base balance, water and electrolyte status under the mandatory control of hematocrit and electrolytes.
Interaction
Carbenoxolone , glucocorticosteroids , drugs with licorice root , laxatives in combination with Lasix increase the risk of developing hypokalemia.
It has been noted that furosemide is able to enhance the nephrotoxic and ototoxic effects of aminoglycosides due to delayed excretion through the renal system. The nephrotoxic effects of medications are enhanced by parallel treatment with furosemide. Kidney damage is also recorded with the use of high doses of cephalosporins , the predominant route of elimination of which is through the renal system.
Cisplatin with furosemide has a pronounced ototoxic effect. The administration of high doses of furosemide (more than 40 mg) increases the nephrotoxic effect of Cisplatin.
The severity of the diuretic effect of Lasix is reduced when taking drugs from the NSAID . With severe dehydration and hypovolemia, NSAIDs can provoke the development of acute renal failure. Lasix enhances the toxic effects of salicylates . During treatment with Phenytoin, the severity of the diuretic effect of furosemide decreases.
Blood pressure-lowering medications, diuretics , and antihypertensive drugs in combination with Lasix can cause a sharp drop in blood pressure.
ACE inhibitors can lead to a deterioration in the functional state of the renal system and provoke hypotension. In severe cases, acute renal failure develops.
A decrease in the effectiveness of Lasix is observed when taking medications that, like furosemide, are secreted in the tubules of the renal system ( Methotrexate , Probenecid ). At the same time, a slowdown in the elimination of these drugs is recorded. There is a weakening of the effect of curare-like muscle relaxants, Diazoxide and Theophylline . The opposite effect is observed with pressor amines ( Norepinephrine , Epinephrine ) and hypoglycemic agents.
A weakening of the effect of furosemide and a slowdown in its absorption are recorded when taking Sucralfate (recommended time interval - 2 hours). Furosemide slows down the excretion of lithium, increasing its concentration in the blood serum, and accordingly increasing the severity of the toxic effect of lithium on the functioning of the nervous system and heart.
The risk of developing gouty arthritis increases with simultaneous therapy with Cyclosporine A , which causes hyperuricemia and impairs the excretion of urate by the renal system.
Intravenous administration of Furosemide within 24 hours after the use of Chloral hydrate causes increased sweating, redness of the skin, tachycardia, increased blood pressure, anxiety, and nausea. The solution for intravenous infusion has an alkaline reaction, which does not allow mixing it with medications whose pH is less than 5.5.
Lasix drug interactions
If the use of the drug is accompanied by the development of hypokalemia and hypomagnesemia, the sensitivity of the myocardium to cardiac glycosides may increase. When combining the drug with GCS, laxatives and carbenoxolone, the risk of developing hypokalemia increases. When Lasix is co-administered with aminoglycosides (kanamycin, gentamicin, tobramycin), cephalosporins or cisplatin, their concentrations in the blood plasma may increase, which can lead to the development of nephro- and ototoxic effects. If forced diuresis is required during treatment with cisplatin, furosemide is prescribed in a low dose (40 mg with normal renal function) and when the body is sufficiently hydrated. NSAIDs, as well as phenytoin and probenecid, may reduce the diuretic effect of Lasix. When used simultaneously with ACE inhibitors, a significant decrease in blood pressure may occur, even to the point of collapse, and in some cases lead to a decrease in renal function and the development of acute renal failure. Caution should be exercised when prescribing Lasix and hypoglycemic drugs simultaneously, as this may require dose adjustment of the latter. If it is necessary to prescribe Lasix and pressor amines (epinephrine, norepinephrine) simultaneously, the increased risk of side effects and reduced effectiveness of the drugs must be taken into account. The drug potentiates the effect of theophylline and curare-like drugs. The simultaneous use of Lasix with lithium preparations can lead to increased reabsorption of lithium ions in the renal tubules and the development of toxic effects.
special instructions
Before prescribing furosemide, the treating doctor must exclude pronounced forms of urinary outflow disorders (including unilateral ones). If urinary outflow is partially impaired, more careful monitoring of patients is required, especially in the first stages of treatment.
In case of diarrhea syndrome, vomiting, increased sweating and other conditions with a high risk of developing electrolyte imbalance, it is necessary to monitor the level of potassium, sodium and creatinine in the blood serum. If necessary, measures are taken to eliminate dehydration or hypovolemia, acid-base and electrolyte imbalances if they occur. In some cases, short-term discontinuation of Lasix may be necessary.
The use of a diuretic drug requires a mandatory intake of food rich in potassium (cauliflower, spinach, lean meat, tomatoes, bananas, potatoes, etc.). If the diet is ineffective, the prescription of special potassium-sparing medications and potassium supplements is required.
Premature infants undergo regular renal ultrasound examinations due to the risk of nephrocalcinosis and nephrolithiasis. During treatment, certain side effects and reactions may be recorded (for example, a pronounced drop in blood pressure), which negatively affect the performance of certain types of activities (driving vehicles, working with complex mechanisms).
In case of cirrhotic damage to the hepatic system and ascites, dosage selection is carried out in a hospital setting (water-electrolyte imbalance can provoke the development of hepatic coma ).
Compatibility Guidelines
It is unacceptable to mix furosemide with other medications in the same syringe.
Emergency measures for the development of anaphylactic shock
In case of cyanosis , nausea, severe weakness, cold sweat and other signs of anaphylactic reactions, the injection is stopped immediately, leaving the needle from the syringe in the vein. The head and torso are lowered down, while simultaneously carrying out the necessary measures to maintain the patency of the respiratory tract.
Urgent measures
Emergency intravenous infusion of Adrenaline ( epinephrine ): a standard solution of 1 ml adrenaline is diluted to 10 ml. Slowly, under the control of blood pressure and heart rate, 1 ml of the resulting solution is administered (corresponding to 0.1 mg of adrenaline). If necessary, further intravenous infusion is carried out. Simultaneously with adrenaline, glucocorticosteroids ( Prednisolone or Methylprednisolone at a dose of 250-1000 mg). Electrolyte solutions and plasma substitutes allow you to replenish the volume of circulating blood. Prescription of antihistamines, oxygen inhalations and artificial respiration are carried out if necessary.
Analogs
Level 4 ATC code matches:
Furosemide
Britomar
Trigrim
Torasemide
Trifas
Diuver
- Furosemide;
- Furosemide-Vial.
Reviews of Lasix
Lasix has established itself as an excellent diuretic and provides immediate relief from edema. However, due to its rapid action, negative effects also appear: the drug washes away microelements even with short-term therapy. One of the advantages is the relatively low cost of both the tablet form and the solution.
Reviews of Lasix for weight loss
The medication really allows you to lose weight without much effort, but the kilograms are reduced due to lost fluid, which is also restored immediately after stopping the medication. In addition, the drug negatively affects water and electrolyte balance, which can negatively affect overall health.
Using Lasix
The dosage regimen is set individually, taking into account the severity of water-electrolyte imbalances, the magnitude of glomerular filtration, and the severity of the patient’s condition. During treatment, the water-electrolyte balance is adjusted taking into account daily diuresis and the dynamics of the general condition. Oral Lasix is usually prescribed on an empty stomach. The drug is prescribed parenterally to patients who cannot take the drug orally, or in urgent cases. The rate of intravenous administration of the drug is at least 1–2 minutes. For moderate edema, the initial dose for adults and adolescents over 15 years of age is usually 20–80 mg orally and 20–40 mg IM or IV. For treatment-resistant edema, the same dose or increased by 20–40 mg (20 mg for parenteral administration) can be re-administered no earlier than after 6–8 hours (2 hours for parenteral administration) until a diuretic effect is obtained. This individually selected dose can be used 1 or 2 times a day. The highest effectiveness is achieved when taking the drug for 2-4 days a week. For children, the initial dose is 2 mg/kg (1 mg/kg for parenteral administration). If the effect is insufficient, it can be increased by another 1-2 mg/kg (by 1 mg/kg - with parenteral administration), but not earlier than 6-8 hours after the previous dose (with parenteral administration - at least 2 hours). For hypertension (arterial hypertension), the initial dose for adults is 80 mg/day (usually divided into 2 doses). If the effect is insufficient, other antihypertensive drugs should be added. For patients with pulmonary edema, Lasix is administered intravenously at a dose of 40 mg. If the patient’s condition requires it, then after 20 minutes an additional 20 to 40 mg of Lasix should be administered. To carry out forced diuresis, 20–40 mg of the drug is added to the infusion electrolyte solution. Further dosing depends on the detoxification program and should be carried out taking into account indicators of water and electrolyte balance.
Lasix price, where to buy
The price of Lasix tablets varies in the range of 50-60 rubles. The solution costs a little more. The price of Lasix in ampoules is approximately 100 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
LuxPharma* special offer
- Lasix tab.
40 mg No. 45 RUR 1,370 order - Lasix solution for injection 2ml 10mg/ml No. 10
RUB 1,480 order
show more
Pharmacy24
- Lasix 40 mg No. 45 tablets Sanofi India Limited, India
42 UAH order - Lasix Neo 10 mg/ml 2 ml No. 10 solution S.S. Zentiva S.A., Rumunia
70 UAH order
PaniPharmacy
- Lasix tablets Lasix tablets. 40 mg No. 45 India, Sanofi India
47 UAH order
- Lasix neo ampoule Lasix NEO solution d/in. 10mg/ml amp. 2ml No. 10 Romania, Zentiva
77 UAH order
show more