Hiatal or hiatal hernia is listed in the International Classification of Diseases under code K44.9. In the medical literature, the disease is often referred to as “HH”.
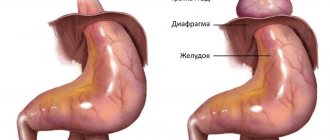
The essence of the pathology is the movement of underlying organs (stomach, omentum, subphrenic segment of the esophagus, intestinal loop) through the ring in the dome of the diaphragm without the obligatory accompanying layer of peritoneum.
Although diagnostic methods make it possible to reliably confirm the disease, in practice there are often cases of long-term treatment and observation of patients with various diseases of the stomach and esophagus caused by secondary changes.
Prevalence
Among all types of diaphragmatic hernias, esophageal hernias account for almost 90%. The older the age, the greater the risk of the disease and the frequency of detection. In people under 50 years of age they occur in 8% of cases, and in older ages - in 70%. It is estimated that up to 6% of the adult population suffers from diaphragmatic hernia.
It has been established that pathology develops more often in women. In early childhood, the formation of a hiatal hernia is usually associated with a congenital defect (short esophagus) with simultaneous weakness of the muscle and connective tissue of the diaphragm. The disease is considered one of the root causes of gastroesophageal reflux in children.
Classification
There are more than 50 classifications of hernias localized in the diaphragm. In practice, the most acceptable are those that take into account anatomical changes, the characteristics of the formed hernia, the size of the hernia opening and the role of the subphrenic part of the esophagus.
The most popular division of hernias according to mobility is sliding (axial, axial) and fixed paraesophageal (paraesophageal). Additionally, mixed hiatal hernias with a complicated course are distinguished.
The share of paraesophageal hernias accounts for no more than 5% (in children 0.3), non-fixed hernias occupy almost 95% (in children 99.4)
Sliding hernias have the possibility of fixation, most often against the background of shortening of the esophagus. Their main symptom is the free movement of the upper part of the stomach and the subdiaphragmatic portion of the esophagus into the chest cavity and back. Able to adjust independently when a person is in an upright position.
Types of axial hernias are distinguished depending on the portion of the stomach that passes into the chest cavity:
- cardiac - a small section of cardia emerges from the esophageal opening;
- cardiofundal - the hernia consists of the cardia and the body of the stomach;
- subtotal - the stomach is displaced into the chest cavity up to the pylorus;
- total - the hernia includes the entire organ with the pyloric section.
Usually, with a fixed cardiac section, the fundus of the stomach or the entire organ, a loop of intestine, the omentum, and rarely part of the spleen emerges into the distended esophageal opening. This species may be disadvantaged. Among fixed hernias, depending on the contents, the following types are considered:
- fundal - the body of the stomach moves into the chest cavity;
- antral - part of the antrum is displaced;
- intestinal - passes through a loop of the small or large intestine;
- gastrointestinal - the intestines and part of the stomach move at the same time;
- omental - the hernia contains an omentum.
There is a division according to the degree of expansion (size) of the hernial opening:
- 1st degree - only the abdominal segment of the esophageal tube lies in the supradiaphragmatic space, the stomach is pulled up to the diaphragm;
- 2nd degree - the vestibule and cardiac part move upward, gastric folds protrude into the diaphragmatic opening;
- 3rd degree - in addition to the abdominal part of the esophagus, the body and antrum of the stomach pass into the chest cavity.
It is possible to classify hiatal hernias in detail only with the help of additional studies.
Operation
The purpose of the operation is to restore the anatomical position and normal function of the cardia. The basic principle is to eliminate the hernial orifice and perform antireflux surgery. This is done by mobilizing and lowering the esophageal-gastric junction into the abdominal cavity, narrowing the esophageal opening of the diaphragm and performing one of the types of fundoplication, which allows you to restore the lower esophageal sphincter, the high pressure zone in it and the angle of His.
- The most common is the operation by Nissen, who proposed a 360° fundoplication for the treatment of a hiatal hernia complicated by esophagitis. It consists of forming a circular cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the mobilized abdominal section of the esophagus, in which a 30-32F1 probe is installed. The edges of the stomach are sutured together with the wall of the esophagus. The width of the cuff is at least 2.5-3 cm. If the hernial opening is wide (more than 3.5 cm), the legs of the diaphragm are sutured together behind or in front of the esophagus (posterior or anterior crurorrhaphy) to the normal size of the POD. When the POD diameter is more than 5 cm, to prevent recurrence of the hernia, it is advisable to strengthen the crurorrhaphy with a mesh prosthesis made of non-absorbable synthetic material.
- Fundoplication according to Nissen-Rossetti also involves a 360° fundoplication with the difference that the gastric cuff is not fixed to the diaphragm (prevention of hiccups and pain during breathing movements), but 1-2 sutures are placed between the esophagus and the gastric cuff on the side opposite from the sutures of the cuff itself (prevention of cuff expansion in the fundus of the stomach). The disadvantage of the Nissen and Nissen-Rosetti operations is the twisting of the esophagus along the axis when the fundus of the stomach is passed under it. This can be avoided by modifying the Nissen operation, in which the first short arteries of the stomach, the posterior (not covered by the peritoneum) wall of the cardia are mobilized, and the anterior and posterior walls of the fundus of the stomach are involved in creating the cuff.
- Toupet fundoplication involves the formation of a symmetrical cuff from the anterior and posterior walls of the fundus of the stomach, enveloping the esophagus at 240-270°, leaving its anterior-right surface free (localization of the left vagus nerve). Used for small stomach fundus. Many authors prefer this method of fundoplication due to the lower incidence of dysphagia in the early postoperative period (compared to the Nissen procedure). This advantage is offset in the future due to a greater number of relapses of reflux disease.
- Fundoplication according to Dor. It also involves partial fundoplication, in which the anterior wall of the fundus of the stomach is placed in front of the abdominal esophagus, fixing it to the right wall of the esophagus. This operation is ineffective; it is rarely used as a forced measure when it is impossible to fully mobilize the esophagogastric junction and perform other types of fundoplication.
- The Cuschieri operation (1991) is the creation of an acute angle of His using the round ligament of the liver, which, after partial mobilization from the navel, is carried out with the free end under the abdominal segment of the esophagus, pulling it to the right and anteriorly (an acute angle of His is formed). Rarely used due to low efficiency.
For hernias combined with pronounced shortening of the esophagus (congenital or due to esophagitis), the Collis-Nissen operation gives the best results. The operation consists of lengthening the abdominal esophagus due to the lesser curvature of the stomach, followed by gastrofundorraphy (enveloping the newly created esophageal tube from the lesser curvature with the walls of the fundus of the stomach according to the Nissen fundoplication type).
Why does a hernia form?
The causes of hiatal hernia consist of two mechanisms. Changes in the structure of the muscular-ligamentous apparatus of the diaphragm, loss of elasticity, atrophy with pronounced loss of tone and stretching.
This process is typical for old age, people who move little, do not exercise, have lost weight for various reasons, patients with chronic systemic diseases of connective tissue, blood circulation, metabolic disorders (Marfan syndrome, hemorrhoids, intestinal diverticulosis, flat feet, diabetes mellitus), if in children the basis of the disorders is genetic diseases or underdevelopment of muscle groups due to a complicated pregnancy of the mother, anomalies (achalasia, short esophagus).
Another important factor is the increase in intra-abdominal pressure. It grows in people:
Causes of pain in the esophagus
- with chronic diseases accompanied by flatulence and constipation;
- with prolonged uncontrollable vomiting;
- with ascites (abdominal enlargement caused by the penetration of plasma from the vessels into the abdominal cavity during congestion) with cardiac decompensation, liver cirrhosis;
- with a large tumor of a benign or malignant nature located in the peritoneal cavity;
- those who have suffered abdominal trauma;
- doing weightlifting;
- during heavy physical loads;
- with abdominal obesity;
- suffering from chronic diseases of the lungs, bronchi, and larynx with a severe cough.
Physiological pregnancy usually does not lead to a hernia, but if a woman is weakened by one of the listed diseases, then even normal enlargement of the uterus has a serious effect on muscle tone and puts pressure on the diaphragm from below. In case of multiple pregnancy or complicated childbirth, the prognosis worsens.
Impaired peristalsis of the esophagus, causing excessive tension and tightening of the cardial part of the stomach, accompanies inflammatory diseases of the esophagus; it supports peptic ulcer disease, calculous cholecystitis and pancreatitis, chronic gastroduodenitis by a reflex mechanism in 15–20% of patients (spasm of the longitudinal muscles occurs).
Of particular importance are burns of the esophagus (thermal or chemical) with the formation of cicatricial adhesions, narrowing of the lumen, and peptic ulcers.
General characteristics of the pathology
Sliding hiatal hernias got their name due to the fact that the posterior wall of the upper part of the cardiac part of the stomach, which is not covered by the peritoneum, participates in the formation of the hernial sac. Initially, the disease is asymptomatic and does not bother the patient at all. After some time, a person may notice symptoms similar to diseases of the gastrointestinal tract and heart. If not treated promptly, symptoms can be so severe that they limit normal life activities.
Nutritional adjustments play a significant role in stabilizing the patient’s condition. This is the use of a gentle diet, which includes:
- exclusion of fatty, fried and spicy foods from the diet;
- avoidance of consuming large amounts of salt;
- lack of smoked meats, marinades, hot seasonings in the diet;
- frequent and small meals.
Proper functioning of the digestive system will be the key to the effectiveness of treatment.
Symptoms and their origin
The disease develops gradually and is characterized by a chronic course. Half of the patients at the early stage do not have any characteristic symptoms of a hiatal hernia; they try to treat gastritis, biliary dyskinesia, and pancreatitis.
The components of the hernia rise above the area of the esophagogastric junction
These diseases cannot be considered “masks” of a diaphragmatic hernia, because the area of the gastroesophageal junction is equipped with powerful innervation and is involved in the regulation of digestive processes, especially in creating the necessary tone of the muscle layer. When the subphrenic segment of the esophagus and stomach slowly moves upward, the greater curvature, the fundus, is first pulled into the hernial opening.
The minor curvature takes on a horizontal position. Such localization creates conditions for the occurrence of reflux (reverse) reflux of contents, since it changes the angle of the connection and eliminates the fold-valve, which acts as a hermetically sealed closure of the lumen. The mechanism of the pathology explains the constant heartburn in patients and frequent belching.
The sliding of part of the organs up and down with an unfixed hernia produces constant irritation of the reflex zone, therefore, despite the rare infringement and asymptomatic conditions, the indication for surgical treatment is the transfer of up to 70% of the stomach volume into the chest cavity.
A fixed hiatal hernia is characterized by the duration and persistence of symptoms. This is a rarer but dangerous pathology. Much more often it leads to complications requiring emergency surgery.
The most common manifestations include:
- pain - the intensity can be different, localized in the epigastric region, radiating to the left scapula, shoulder, behind the sternum, sometimes of a girdling nature, cramping or dull pain in the right hypochondrium confirms the involvement of the motor activity of the bile ducts, pain is associated with the position of the body (intensifies when lying down , when bending forward);
- heartburn - accompanied by pain, does not go away for a long time after overeating;
- belching of recently eaten food, air - caused by the return of a bolus of food from the stomach into the esophagus due to damage to the lower sphincter, accompanied by temporary relief of the condition;
- difficulty swallowing - occurs in 1/3 of patients when the esophagus is narrowed in the lower segment, especially when eating hot or cold foods (rarely observed in children).
Belching affects 60% of patients
Unlike angina pectoris, patients' condition improves in an upright position after walking.
Patients are less likely to worry about:
- prolonged painful hiccups;
- nausea, vomiting (sometimes with blood);
- feeling of bitterness in the mouth;
- hoarse voice;
- burning at the root of the tongue;
- increased salivation;
- tendency to lower blood pressure.
These signs are caused by irritation of the branches of the vagus nerve, the entry of acidic contents and bile into the larynx (especially during sleep). Manifestations of a sliding hernia are distinguished by heartburn, since more conditions are created for the formation of gastroesophageal reflux. A fixed hernia causes pain, especially if it reaches a large size.
When the pleural cavity is compressed, shortness of breath and arrhythmias (extrasystole, paroxysmal tachycardia) associated with food intake may occur. A serious diagnostic error occurs when symptoms are confused with heart disease. A hiatal hernia may be mistaken for angina, and arrhythmias may not be treated successfully. Patients often end up in the cardiology department with pain.
Folk technique
Traditional methods of treatment will help relieve spasms, alleviate the patient’s general condition and relieve pain, but in order to completely recover from the disease, more qualified help will be required.
For heartburn
- Licorice. Take a few licorice roots and the peels of two oranges. Steam them with boiling water: place in a saucepan and keep on fire until all the water has boiled away. Then grind the pulp and add honey to it. Drink 15 minutes before meals.
- Linen. Brew flax seeds and leave in a thermos until they become soft. Strain the infusion. Drink half a glass twice a day.
From flatulence
Take cumin seeds and leave in boiling water for an hour. Can be used for a long time every hour. Chamomile tea, which has an anti-inflammatory effect and relieves spasms, will also help with bloating.
What complications does a hiatal hernia lead to?
The more severe the hernia and the longer targeted treatment is delayed, the more the risk of complications increases. The most commonly observed:
- pinching of organs that have moved from their anatomical location by the muscles of the diaphragm;
- reflux esophagitis - inflammation of the esophagus, as a result of constant reflux of the acidic contents of gastric juice, leading to ulcers on the surface of the mucosa, perforation;
- formation of adhesions, scars, narrowing of the lumen of the esophagus;
- stomach ulcer;
- acute or chronic bleeding from varicose vessels of the esophagus and stomach, anemia;
- attacks of angina pectoris, which are difficult to combat with nitro drugs;
- Barrett's esophagus is a precancerous disease.
The likelihood of malignant degeneration of mucosal cells increases
Features of treatment
If you had to face a problem such as a hiatal hernia, then there may be two ways out of the situation: surgical or conservative treatment. The main task of classical methods can be defined not as the elimination of the hernia itself, but as a reduction in the symptoms of reflux esophagitis and neutralization of gastroesophageal reflux. That is, doctors strive to relieve pain and prevent possible complications. These goals are achieved through a diet based on small and frequent meals.
| View | Description |
| Drug therapy | It is necessary to take medications that correct the motor process of the stomach and normalize secretory activity. In general, inhibitors, antacids, and prokinetics are used for such therapy. Drug treatment is used only in the early stages without complications. Thanks to the medications, the patient’s vitality increases and he feels relief. If treatment is applied in a timely manner, the likelihood of complications is significantly reduced |
| Surgical treatment | This method is used extremely rarely, only when drug therapy is ineffective or complications arise. |
During this treatment you will have to give up some foods. We are talking about chocolate, carbonated drinks, coffee, animal fats, fresh bread and other flour products. Also, doctors do not recommend resting in a lying position for the next 3 hours after eating during such treatment.
Axial hernia, regardless of the degree and severity, is mainly eliminated by conservative treatment methods.
| Treatment with diet | Drug treatment |
| The patient must switch to fractional meals. That is, food intake should occur in small portions, but much more often. In this case, all food should be crushed to a mushy state and consumed only warm. Some foods will need to be excluded from your usual diet, as they can be irritating to the mucous membrane of the digestive tract. These include all pickles and marinades, spicy foods, smoked meats | The use of antacids is indicated, which suppress the activity of gastric juice (Phosphalugel). Take enveloping medications (Vicalin). To eliminate painful sensations, you can use painkillers (Novocaine). Use of antispasmodics (No-spa) |
Bad habits can complicate the process of fighting the disease, so you will have to give them up. Exposure to pharmacological drugs is also possible. These can be proton pump inhibitors, prokinetics, antacids, etc. As for surgical intervention, it is relevant only if conservative treatment has not given the desired effect. The laparoscopic technique is most often used.
How do signs relate to the severity of the disease?
The abdominal part of the esophagus is covered with a parietal layer of peritoneum in front and on the sides, and the stomach lies completely inside a bed of visceral peritoneum. If the posterior wall of the esophagus is pulled into the diaphragmatic opening, then the classic signs of a hernial sac are violated - there will be no peritoneal wall.
The degree of hiatal hernia is determined during diagnosis by the severity of displacement of the stomach and esophagus into the chest cavity. Mild (first degree) - does not cause any disturbances, since only 2 lower segments of the esophagus (intra- and subdiaphragmatic) pass into the supradiaphragmatic space. The size of the distended esophageal opening does not allow the stomach to “stretch out.”
Inflammation (esophagitis, gastritis) may develop, but severe symptoms of digestive disorders do not occur. Second degree - in addition to the esophagus, the upper part of the stomach exits into the hernial opening, but remains at the level of the esophageal dome of the diaphragm. The patient exhibits all the typical signs of hiatal hernia; belching and heartburn are especially bothersome after eating.
Third degree - there is a movement of a large part of the stomach into the chest cavity, the subdiaphragmatic zone of the esophagus; in severe cases, the entire stomach is found in the chest cavity.
Possible complications
To the extent that axial hiatal hernia can develop asymptomatically for a long time, the likelihood of untimely diagnosis and treatment increases, resulting in complications:
- Bleeding may begin in the esophagus.
- The hernia is strangulated.
- Esophageal perforation is a common occurrence.
- A peptic ulcer of the esophagus develops.
- Cicatricial narrowing of the esophagus occurs.
But, complications are possible even after surgery during the rehabilitation period:
- Abnormal dilatation of the esophagus may occur.
- Recurrences of axial hernia occur.
- The stomach area becomes pathologically enlarged.
If an axial hiatal hernia is present, a lung problem in the form of aspiration pneumonia may occur. To eliminate this consequence, antibiotics are required, which are introduced into the body without affecting the digestive tract. It is very important to diagnose the complication in time and begin immediate treatment.
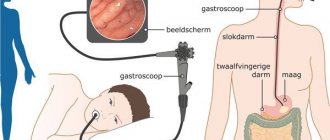
Diagnostics
The disease cannot be assumed with complete confidence only on the basis of patient complaints and examination. The main objective methods for diagnosing pathology must accurately determine which organs and to what extent they move from the abdominal cavity to the thoracic cavity through the esophageal opening in the diaphragm. For this purpose:
- plain chest x-ray;
- examination of the esophagus and stomach with a radiopaque substance;
- esophagoscopy - examination of the esophagus with a special apparatus (esophagoscope);
- fibrogastroscopy is a common way to identify internal problems in the mucous membrane of the esophagus and stomach using a flexible thin hose equipped with optics.
The main radiological signs of hiatal hernia: abnormally high location of the lower segments of the esophagus with a transition to the chest cavity, movement of the cardiac valve into the supradiaphragmatic space, a distended esophageal opening in the dome of the diaphragm, stagnation of contrast in the contents of the hernia.
Endoscopic studies reveal:
- inflammation of the stomach and esophagus;
- shortening of the esophagus due to spastic contraction;
- gaping of the cardiac sphincter or lack of tightness during closure;
- picture of reflux reflux;
- displacement of the line of connection of the esophagus with the stomach to the supradiaphragmatic position;
- narrowing of the lower end of the esophagus.
During fibrogastroscopy, material is taken for cytological examination of tissues to exclude the possibility of tumor growth. To determine the tendency of a hernia to internal bleeding, a stool test is performed for the Gregersen reaction, red blood cells and hemoglobin are checked if anemia is suspected.
Esophageal manometry method - allows you to study the ability to contract the longitudinal and circular muscles of the esophagus, coordination of sphincter contractions, peristaltic movements of the stomach
Impedancemetry is a method of identifying the functioning of the esophagus and stomach by measuring the electrical resistance between the inserted electrodes with a probe. Gastrocardiomonitoring is used to simultaneously monitor the activity of the heart and upper digestive tract. The method combines ECG recording and acidity measurements.
The acidity of gastric juice and its return into the esophagus are studied using the pH-metry method. It is possible to compare the effectiveness of combined conservative treatment of hiatal hernia without surgery.
How is the disease diagnosed?
Pathology is often identified when determining the causes of gastric contents reflux into the esophagus, pain in the chest and/or abdomen. To establish a diagnosis, the following is carried out:
- endoscopic examination - will exclude other diseases of the digestive tract, in which similar symptoms may be observed;
- stool test for occult blood - to exclude bleeding in the gastrointestinal tract;
- X-ray examination - may be required to exclude diseases of the respiratory system;
- ECG (electrocardiography) – for the purpose of differential diagnosis with diseases of the cardiovascular system.
Symptoms of strangulation
The infringement is explained by the jamming of organs passing through the hernial canal in an unusual place, the impossibility of returning. The main cause is a sudden contraction of the diaphragm muscles or torsion of the hernial sac. Significantly more painful symptoms appear than during the course of the disease.
They are caused by poor circulation in the displaced organs and tissue necrosis. The pain becomes cutting, intense, localized behind the sternum, constant, radiating to the back and abdomen. Heartburn is perceived as a burning sensation. Profuse belching appears, followed by vomiting. The abdomen is distended and weakness increases. Body temperature rises, sometimes the patient shudders.
During fibrogastroscopy, performed for emergency reasons, a change in the color of the strangulated section is detected, from gray-blue to black (gangrene). The patient should be operated on immediately. Timely removal of pinched parts of organs is the only way to save lives.
What do doctors recommend?
Ignoring or improperly treating a hernia can lead to dire consequences: terrible pain, dependence on painkillers, and limited movement. Not to mention the threat of complete paralysis, when there is no way out.
- rejection of bad habits;
- rational and balanced nutrition;
- healthy lifestyle;
- moderate physical activity;
- body weight control;
- timely and correct treatment of all concomitant diseases.
By following basic rules, you can not only reduce the risk of developing a hernia, but also other diseases of the gastrointestinal tract. In any case, self-medication should be excluded. The sooner a person seeks medical help, the greater the chance of a successful prognosis. Disregarding the fact of the occurrence of a hiatal hernia is a big mistake. If such a diagnosis has been made, then the treatment process must be taken as seriously as possible. Otherwise, the condition may worsen significantly.
Is it possible to get rid of a diaphragmatic hernia without surgery?
Treatment of a hiatal hernia depends on the degree of movement of organs into the hernial opening, the presence of complications, and concomitant diseases. In the first degree, the disease is detected by chance and does not bother the patient, but to prevent further development of the pathology, doctors advise:
- adjust the diet - all foods and dishes that cause increased fermentation, constipation, increased secretion of juice in the stomach, which contribute to weight gain, should be excluded from the menu;
- normalizing weight is a long process that requires proper nutrition and physical activity, since not all exercises can be performed, you should only do therapeutic exercises, the complex must be chosen with the participation of a specialist;
- in everyday life you will have to give up carrying heavy objects;
- To prevent gastric juice from flowing into the esophagus at night, it is recommended to sleep in a semi-sitting position and raise the head end of the bed.
The photo shows contraindicated work in a forced inclined position
After examination, individual characteristics of the course and the predominant mechanism of damage are revealed in each patient. Medications are prescribed according to this principle. To reduce acidity and prevent damage to the esophageal mucosa, the following are used:
- antacids (Almagel, Gastal, Maalox);
- proton pump inhibitors (Pantoprazole, Esomeprazole, Omeprazole);
- antihistamines (ranitidine).
Prokinetics (Motilium, Motilak, Trimebutin) help normalize muscle contractions. Vitamins of group B specifically influence the nervous regulation of sphincters, the cardia zone, and restore epithelial tissue.
To relieve pain, local enveloping agents (Almagel A) are recommended; non-steroidal anti-inflammatory drugs (Ibuprofen, Nurofen) are less commonly prescribed, since they themselves can cause an inflammatory process in the stomach.
Folk remedies can support and enhance drug therapy. Various herbal decoctions perform the same functions as medicines, but less productively: dill and flax seeds, chamomile flowers, licorice root, senna leaf. To realign organs that have moved upward, healing clinics recommend that patients jump from the top step to the bottom.
A sharp “landing” on the heels replaces jumping
How is a hernia treated at the CELT clinic?
At the initial stage, conservative methods of hernia treatment are used. The clinic of concomitant diseases of the gastrointestinal tract comes to the fore, so therapy is aimed at eliminating them. The clinic’s gastroenterologists will select an individual treatment regimen that includes a basic list of drug groups:
- antacids;
- proton pump inhibitors;
- H2-histamine receptor blockers;
- drugs that improve motor skills (prokinetics);
- B vitamins.
Indications for surgical removal of the hiatal hernia:
- Fixed large hiatal hernia.
- Long-term and ineffective conservative therapy.
- Development of complications of the disease.
- Precancerous condition of the mucous membranes (so-called dysplastic changes).
In our clinic, preference is given to low-traumatic surgical interventions - laparoscopic operations, which allow access to internal organs through small punctures in the skin measuring 0.5-1 cm. To avoid relapses, surgeons always install a mesh implant.
There are main groups of surgical interventions:
- Crurorrhaphy (suturing the hernial opening and strengthening the ligamentous apparatus).
- Gastropexy (attachment of the stomach to the abdominal wall).
- Fundoplication (surgery restores the normal relationship of the fundus of the stomach with the lower part of the esophagus).
- Partial removal of the esophagus (performed in the presence of a scar stricture).
Specialists will give all the necessary recommendations and describe in detail the principles of diet therapy and proper lifestyle. Thus, people suffering from hiatal hernia should eat no later than 3 hours before bedtime, sleep with the head elevated, normalize weight, and avoid overeating and heavy lifting. After surgery, patients must be observed by a gastroenterologist. Relapses of the disease are extremely rare.
The success of treatment for hiatal hernia depends on the level of qualifications and experience of doctors, as well as (to a large extent!) on the patient’s compliance with all the doctor’s recommendations. Rest assured that at the CELT clinic you will receive decent attention and high-quality medical services.