Our license
Our doctors
Prices
Omphalitis of a newborn is a bacterial inflammatory process that occurs in the umbilical wound and ring, as well as in the surrounding subcutaneous fat and umbilical vessels.
The disease occurs due to lack of care for the newborn, infectious pathology in the mother, and violations of sanitary and epidemiological regulations in maternity hospitals. The causative agent is staphylococci, which penetrate through the placenta or during surgical treatment of the umbilical cord after its circumcision, and occasionally due to catheterization of the umbilical vein. Consider catarrhal, phlegmonous and necrotizing omphalitis.
General overview
An organ as insignificant as the navel is essentially a useless part of the human body. Only during the period of gestation does it play a vital role in the life and development of the child. After birth it becomes unnecessary. The navel is a natural scar that appears after excision of the umbilical cord in a baby on the anterior abdominal wall.
The obstetrician cuts and compresses the cord, and ten days later its remains fall off, forming a wound. After it heals, a neat navel appears on the stomach. However, things don't always go so smoothly. Sometimes mothers notice that the navel begins to get wet. This occurs due to infection of the umbilical wound, manifested in the form of redness, swelling, purulent discharge, fever, and abdominal pain. This phenomenon cannot be ignored.
Inflammation of the navel can also occur in adults. The disease is called “omphalitis”. It is characterized by the development of an inflammatory reaction of the skin and subcutaneous tissue in the navel area. In advanced stages, there is a risk of developing umbilical sepsis. The pathology is accompanied by a change in the shape of the navel. It becomes convex and hot, especially near the inflammatory focus.
Omphalitis in adults can be complicated by the appearance of an umbilical fistula. In this case, surgical intervention is required. The causes of omphalitis can be different, which determines further treatment tactics. Therefore, if you have a problem like this, you should immediately contact a specialist. Most often, the development of the disease is provoked by bacterial and fungal infections.
Omphalitis in adults can occur after piercing or improper care of the wound after the procedure. Depending on the root cause, there are two main forms of the disease:
- primary – the infection penetrates directly into the umbilical wound;
- secondary - the infection joins the fistula.
Depending on the form, omphalitis can be acute or chronic. And there is also a classification that divides pathology into categories depending on the nature of the inflammation:
- catarrhal. This is the most common type of disease. Serous fluid is released. Crusts appear;
- phlegmonous;
- gangrenous – difficult to treat;
- purulent. The navel protrudes above the abdominal wall. Ulcers and purulent discharge form. The gangrenous and purulent form is classified as a necrotic type of omphalitis.
Classification
Inflammation of the navel does not have a generally accepted classification, however, based on clinical data, the following forms are distinguished:
- catarrhal (wetting navel);
- purulent;
- phlegmonous;
- necrotic.
If the umbilical vessels are affected, phlebitis and arteritis occur.
Most often this pathology occurs in children. However, inflammation of the navel in adults also occurs and the reasons for this are:
- Infection due to poor hygiene and skin trauma.
- Navel fistulas.
- Thrombophlebitis of the umbilical vein.
- Endometriosis of the navel.
- Inflammation of the urachal cyst. The urachus is the urinary duct in the embryo that connects the top of the bladder and the umbilicus. A uruchus cyst is a non-occlusion of the middle part of the urinary duct. In adults, the urachus is represented by a fibrous cord that connects the bladder and the umbilicus.
If a woman's navel gets wet, this is not the norm. The scar at the site of the fallen umbilical cord should always be dry and not cause any discomfort in the woman. If there is pain, an unpleasant odor and redness, these are signs of inflammation. If the navel is red and wet, first of all you need to suspect omphalitis in adults and consult a surgeon.
Catarrhal omphalitis occurs with serous discharge from the navel, slight redness of the skin inside the navel and the umbilical ring itself occurs. Usually, thorough treatment of the cavity with antiseptics ( hydrogen peroxide , Chlorhexidine , Miramistin ) and antibiotic ointments ( Levomekol , Levosin ) give a quick positive result.
In the absence of treatment and a decrease in the protective properties of the body, the inflammatory process progresses and purulent omphalitis develops.
At the same time, the swelling and redness of the navel ring increases, inflammation of the fatty tissue becomes pronounced and pus appears in the navel. Phlegmonous omphalitis is manifested by severe inflammation around the umbilical ring, swelling and protrusion of the navel area. The resulting abscess leads to phlegmon of the abdominal wall. With this form, veins and arteries are involved - the umbilical vessels are thickened, painful and easily palpable. The vessels of the anterior abdominal wall dilate, the umbilical region bulges, and the skin around the navel is significantly hyperemic.
The necrotic form of omphalitis is a fairly rare complication of the phlegmonous form in severely weakened and premature children. The skin in this form becomes purple-bluish, skin necrosis and detachment from the underlying tissues occur. In a large wound, the muscles of the abdominal wall and fascia are exposed, which undergo purulent melting. Intestinal prolapse may also occur through the resulting muscle defect. This form is the most severe and ends with the development of sepsis .
One of the causes of navel inflammation is pathology of the urachus (urinary duct), which is more often diagnosed in newborns and occurs in 30-50% of children. The urinary duct must close at certain times during the embryonic period. Malformations of the urachus, depending on the degree of nonfusion, are divided into: umbilical fistula, urachus cyst, vesico-umbilical fistula and bladder diverticulum. Of all the possible anomalies of the urachus, the most common are urachus cyst and umbilical fistula.
Umbilical fistula is most often a congenital pathology and is detected immediately after birth. The urinary duct connecting the navel with the upper part of the bladder should normally close by 5-6 months of fetal development. Sometimes the lumen of the urachus remains throughout life and in this case a vesico-umbilical fistula (ICD-10 code Q64.4. Anomaly of the urinary duct) or a cyst is formed. With a fistula, urine acts as the discharge. The skin around it becomes inflamed and irritated by the discharge. When examining with a probe, a pocket is identified in the direction of the bladder. A fistula develops not only when the urinary duct is not closed, but also the vitelline-intestinal duct. When the vitelline-intestinal duct is not closed, an intestinal-umbilical fistula is formed and then the discharge can be intestinal or mucous. In rare cases, the intestinal mucosa or, much less frequently, the omentum emerges through this fistulous tract.
An acquired umbilical fistula is formed after a long inflammatory process, localized on the anterior wall of the abdomen, if an abscess . Urachal pathology in adults often does not manifest itself and is an incidental finding during cystoscopy and cystography .
Only a suppurating urachal cyst can manifest itself. In the case of congenital and acquired fistula, treatment is surgical - excision of the fistula and suturing of existing defects in the wall of the intestine or bladder. In the presence of an umbilical fistula, conservative therapy is possible at first in the hope of complete fusion of the duct.
Urachal cysts manifest themselves during inflammation and suppuration. A suppurating cyst can form a fistulous tract and pus will come out, and its amount increases with palpation below the navel. If a suppurating urachal cyst communicates with the bladder, cystitis . peritonitis occurs , and suppuration is complicated by phlegmon of the anterior abdominal wall . Both conditions are extremely severe.
Causes
The disease develops as a result of infection. Provoking factors that can contribute to the introduction of pathogenic microflora include the following:
- failure to properly observe personal hygiene rules;
- improper treatment of the umbilical wound;
- use of dirty bedding or underwear, towels;
- contamination with urine or feces;
- improper treatment of resulting skin lesions;
- touching the umbilical wound with dirty hands.
Infectious diseases, to which women are more susceptible during pregnancy, play an important role. Pathogenic microflora can easily infect the umbilical cord. The following microorganisms most often act as causative agents of omphalitis:
- staphylococci,
- streptococci,
- coli,
- Pseudomonas aeruginosa.
Features of the anatomical structure are also associated with the likelihood of the disease occurring. If the umbilical canal is narrow and deeply retracted, dying skin cells and sebaceous gland secretions can accumulate in it. Omphalitis in children mainly occurs as a result of improper or insufficient care.
The photo shows one of the most common causes of omphalitis - piercing
Inflammation can occur if the baby is bathed under unboiled tap water or the baby's undershirt is not washed well enough. This can easily cause the umbilical cord to become infected. As a result, liquid begins to accumulate in it, on the surface of which a crust appears.
After it dries and falls off, small sores remain in its place. This type of omphalitis is called simple or catarrhal. If a purulent secretion is released from the wound, the skin turns red and swells, and the baby’s temperature rises, then we are talking about a purulent form. Treatment is carried out in a hospital setting.
Omphalitis in adolescents and adults is much less common. And this is understandable, because the umbilical wound has healed a long time ago, and the likelihood of a pathological focus appearing is negligible. However, the disease can still occur if a person does not thoroughly wash the navel area and does not remove the contaminants accumulated in it.
Various factors can contribute to the progression of the disease:
- weakened immune system;
- hypothermia;
- overwork;
- prematurity, low weight (infantile omphalitis);
- infectious skin diseases;
- scratches, cuts, scratching in the navel area;
- presence of scars or tattoos;
- rubbing the navel with tight clothing or a belt buckle;
- inflammation after surgery;
- excess weight;
- presence of diabetes mellitus.
Important! Young women who like to decorate their bellies with piercings are at risk.
Another cause of infection may be a fistula. It is a channel through which different cavities are connected. Fistulas can be congenital or acquired. They may produce yellow liquid, feces, and urine.
For incomplete fistula, conservative treatment is prescribed. Baths with potassium permanganate and bandages with a chlorophyllipt solution will be effective. You can dry the wound with iodine or brilliant green. If the fistula does not heal, surgery is performed.
Prevention
Measures to prevent omphalitis in adults are:
- avoiding injuries to the umbilical area;
- maintaining personal hygiene and caring for the umbilical area, especially in case of obesity and excessive sweating ;
- performing piercings in beauty salons, which carefully monitor the disinfection of instruments;
- treatment with antiseptic compounds after piercing;
- rational nutrition to maintain a high level of immunity;
- If signs of inflammation appear, start antiseptic treatment and consult a doctor promptly.
Measures to prevent this disease in children include:
- Treatment of urogenital infections in pregnant women, as they cause omphalitis in the newborn.
- Compliance with the technique of cutting the umbilical cord and processing the remainder after childbirth.
- Compliance with the rules of asepsis and antisepsis in the delivery room and when working with newborns.
- Application of the “dry method” of managing the umbilical remnant. It is intended to keep the umbilical cord dry and clean. It should be left outdoors (or covered with a cloth) and allowed to dry naturally. In the area of the stump there is no need for regular application of antiseptic agents that irritate the skin and disrupt its integrity. The passage of the umbilical cord occurs faster if natural drying is used.
- Teaching mothers to care for the umbilical cord of a newborn. It is important to prevent its contamination, and it is also not advisable to apply antiseptic solutions unless necessary. Their application changes the microbiocenosis of the skin .
Symptoms
In newborns, the umbilical wound usually heals within two weeks. When handled correctly, it tightens. However, if an infection occurs, the wound does not heal for a long time, and serous-purulent fluid is released from it. First a crust appears, then it peels off, opening the wound again. The main symptoms of omphalitis include redness, swelling, and discharge.
In adults, a mild form of omphalitis most often develops. It manifests itself in the form of swelling, redness and discharge. In more severe cases, the secretion is bloody and purulent. The navel doesn’t just get wet, it emits an unpleasant odor. It becomes bulging and hot to the touch. Omphalitis is characterized by the appearance of not only local signs, but also general ones.
A person’s body temperature rises, he becomes lethargic and apathetic. At the necrotic stage of the disease, all layers of the abdominal wall are affected. Inflammation even spreads to internal organs. The skin turns dark blue. The danger of this condition is the development of peritonitis and sepsis - complications that can lead to death.
Kinds
Experts distinguish three forms of omphalitis. Each of them is a consequence of the previous one and occurs in the absence of treatment. So, omphalitis has three stages of development:
- weeping navel, or simple form;
- phlegmonous variety;
- necrotic or gangrenous inflammation.
Simple
The general condition of the patient is not impaired. In the navel area there is weeping with serous or purulent discharge. The pathological secretion dries out, becoming covered with a thin crust. At the bottom of the wound, during a long-term pathological process, mushroom-shaped tumors can form.
The child is calm. He has normal body temperature, restful sleep and a healthy appetite. The edges of the wound usually do not change or may be slightly swollen. The umbilical vessels cannot be palpated.
Important! Catarrhal omphalitis causes exclusively local changes.
The causative agents of the inflammatory process are most often staphylococci. The occurrence of catarrhal form in infants is facilitated by intrauterine hypoxia, a thick umbilical cord, and violation of aseptic rules when treating the navel. And also apply tetracycline ointment or synthomycin emulsion.
Despite the fact that this is a mild form of omphalitis, treatment must be started immediately, otherwise the disease will cause serious complications. Therapy can be carried out on an outpatient basis. Several times a day you need to treat the wound with an antiseptic solution. During processing, do not forget to remove any crusts that have formed. Among physiotherapeutic procedures, ultraviolet irradiation is used locally.
The simple form manifests itself only with local signs
Phlegmonous
This is a dangerous stage of ophthalitis, in which the inflammatory process affects surrounding tissues. There is a gradual deterioration in the general condition. With the development of phlegmon of the anterior abdominal wall, the temperature rises above 39 degrees. In this case, the umbilical fossa is an ulcer. When pressed, a purulent secretion is released from it.
Why does my stomach hurt just above my navel?
The discharge has an unpleasant odor. The area around the navel is inflamed and swollen. When pressed, severe pain occurs. Local manifestations are accompanied by symptoms of intoxication.
The patient becomes lethargic and apathetic. He has no appetite. Children are capricious and have frequent regurgitation. Phlegmonous omphalitis is an indication for hospitalization.
The child’s body, due to physiological characteristics, is not able to fully combat damaging factors. That is why from the first days of life the baby must be carefully cared for. Specific treatment is carried out by a surgeon. The specialist uses drainage to drain purulent contents. To do this, an incision is made into the umbilical ring and a drain is inserted.
Necrotic
It is extremely rare in weakened patients with impaired immune system function. Inflammation spreads deeper, affecting internal organs. The skin becomes dark. It resembles a bruise after a blow.
There is a high probability of developing peritonitis - inflammation of the peritoneum, which can be fatal. The spread of infection to the umbilical vessels can lead to sepsis - blood poisoning. Doctors prescribe broad-spectrum antibiotics as treatment. Often the patient requires surgical intervention.
Pathogenesis
The pathogen penetrates the tissues surrounding the navel in different ways (through the placenta or umbilical cord stump) and causes catarrhal, purulent or even necrotic inflammation. The infection spreads to the umbilical vessels, causing an inflammatory process in them ( phlebitis , arteritis ). The incidence of phlebitis in newborns increases with catheterization of the umbilical vein for infusion therapy.
The spread of inflammation leads to the development of phlegmon in the umbilical area. The infectious process in thrombophlebitis of the umbilical vein spreads along the portal vein to the intrahepatic branches of the portal vein - purulent foci are formed along the veins, despite the fact that the umbilical wound may have healed by this time.
Treatment
It is simply impossible to independently determine the cause of navel inflammation. A surgeon's consultation is necessary. And a bacteriological culture of the discharge from the umbilical wound will also be required. Treatment of omphalitis directly depends on the cause of the disease. Most often it is treated conservatively, but if fistulas form, surgery cannot be avoided.
Important! Maintaining navel hygiene while it is healing is the best prevention of omphalitis.
Antibacterial agents in the form of ointments and tablets are used as treatment. If the causative agent of inflammation is a fungal infection, antifungal drugs are prescribed. Anti-staphylococcal immunoglobulin is also administered in the injections. The main emphasis is on strengthening the immune system. For this purpose, vitamin therapy is carried out.
Piercing
Navel piercing should be performed in a specialized salon by a professional piercer. The use of exclusively sterile materials, as well as high-quality products, will minimize the risk of unpleasant consequences. After the procedure, there is usually pain and swelling. In this case, a cold compress will help. To prepare it, just apply a towel moistened with water. You can also wrap a piece of ice in a cloth.
If bleeding occurs, it is best to use a bandage tampon. The patch should not be used. The navel area should be protected from damage and infection. Before touching jewelry, you should wash your hands with antibacterial soap. And you should also remove dust and dirt from under your nails. Bed linen and personal towels should be changed at least once a week.
The navel area must be treated with disposable wet wipes. You should also temporarily limit contact with pets. It is better to use antibacterial soap for cleansing. Alcohol and hydrogen peroxide will not work. To process, take a cotton swab. The procedure must be performed carefully. Don't pull the decoration.
Saline solution has good disinfecting properties. To prepare it, you need to dissolve a quarter teaspoon of sea salt in a glass of warm boiled water. The finished product is used to prepare compresses. After disinfection, lightly soap the piercing and then gently pat it dry with a disposable napkin.
Until complete healing, you should not change the original decoration. There is no need to touch it, tug or rotate it. Avoid wearing tight clothes and underwear. It is better to replace a hot bath with a shower with water of moderate temperature. A stream of water will thoroughly clean the wound of dirt and detergent residues, preventing them from entering the wound.
Until complete healing, it is forbidden to swim in the pool or open water. In extreme cases, it is better to use a waterproof plaster
Tests and diagnostics
The diagnosis is established upon examination of the patient: the presence of serous or purulent inflammation of the umbilical wound, swelling and hyperemia of the umbilical ring, tenderness of the umbilical vessels, delayed epithelization of the wound.
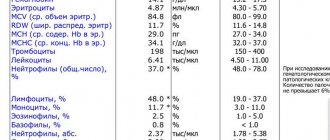
Laboratory tests include:
- Blood test - leukocytosis is determined with a shift in the leukocyte formula to the left and an increase in ESR.
- Sowing the discharge from the wound to determine the pathogens.
- Blood culture to determine the sensitivity of microflora to antibiotics.
- In case of phlegmonous or necrotic form - ultrasound of internal organs.
Instrumental research. The wound is probed to exclude umbilical fistulas. A test is also performed with a solution of methylene blue , which is injected into the fistula and the appearance of the drug in the urine or feces is observed (they become blue).
The most important
Omphalitis is inflammation of the navel. In adults, the disease most often occurs after piercing if hygiene rules are not followed. Diabetes and excess weight can contribute to the onset of the disease. In infants, omphalitis is the result of improper care. The catarrhal stage is the mildest form of the disease, but if left untreated it can progress to a purulent phase.
If the cause of inflammation is a bacterial infection, it must be treated with antibiotics. But first, a bacterial culture of the discharge is carried out. Treatment includes treating the wound with antiseptic solutions. In severe cases, surgery will be required.