Chlamydia is a disease included in the list of the most dangerous sexually transmitted infections. It is classified as a “new” disease, since chlamydia began to be identified only a few decades ago. The disease occurs hidden, but despite its apparent harmlessness, it causes enormous damage to health and affects the course of pregnancy and the health of the newborn if chlamydia is detected during pregnancy.
Appointment with a gynecologist, urologist - 1000 rubles. Consultation with a doctor based on the results of tests or ultrasound - 500 rubles.
If untimely or absent treatment, chlamydia causes complications. In women this is infertility, in men it is epididymitis (inflammatory process in the testes). Complications of chlamydia also include Reiter's syndrome, prostatitis, salpingitis, endometritis and many others.
What is chlamydia: causes and characteristics of infection
The content of the article
The frequency of infection with chlamydia is lower than that of gonorrhea, but, nevertheless, chlamydia is practically the most common sexually transmitted disease. Every year there are about 200 million new infections with chlamydia. Chlamydia is caused by the chlamydia bacteria - Chlamydia trachomatis.
Invading the body, chlamydia primarily affects the human genitourinary system and urogenital tract. In this case, chlamydia can occur as a single infection or in combination with other infections of the genitourinary system: trichomoniasis, bacterial vaginosis.
Chlamydia is a bacterium that penetrates inside a cell and uses its substances for nutrition and other aspects of life. This is an energy parasite that is unable to synthesize ATP on its own. Chlamydia reproduces by division, the microorganism has its own DNA and RNA. As a result, human mucosal cells die.
When chlamydia enters the body, it can successfully resist the immune system and live there for many years, but not harm the carrier until a certain point. At the same time, “dormant chlamydia” is still dangerous - an infected person acts as a carrier capable of infecting other people.
Now almost 1 billion people are carriers of chlamydia. As soon as circumstances change—for example, the immune system weakens—chlamydia immediately becomes more active.
A disease without a history
Just some 30 years ago, no one had heard of chlamydia: data on incidence before the mid-80s simply did not exist. So where did it come from and does it have a story?
The history of chlamydia began back in 1907, when the Czech scientist Stanislav von Provacek went on an expedition to the island of Java to study syphilis. Provacek conducted an interesting experiment: he infected orangutans with scrapings from the conjunctiva of Indonesians suffering from trachoma. This is how a previously unknown microorganism was found, which was called “chlamydozoa,” which translated from Greek means “a cloak wrapped around the shoulder.” The association with ancient chlamys arose for the researcher when he saw inclusions of microbes “draping” the nucleus of an infected cell.
For a very long time, scientists could not understand who to classify chlamydia as - bacteria or viruses. In 1957, the microbe was isolated from a chicken embryo, and in 1963 - from a cell culture. Only then did it finally become clear that Chlamydia trachomatis is a bacterium. But only in the 80s of the last century was the connection between chlamydia infection and inflammatory diseases of the genitourinary tract proven.
The medical world has been moving towards this discovery since 1965, when the prevalence of non-gonococcal urethritis, not associated with either syphilis or gonorrhea, sharply increased. The alarming trend forced doctors to start searching for a new pathogen. The causative agent was found, but the answer to the question of whether cases of urethritis were caused by chlamydial infection or not remained a mystery. Apparently, no one will ever know where and when urogenital chlamydia came to us. But he came and is not going to leave.
How can you become infected with chlamydia: once is enough
The widespread distribution of the disease is explained by the fact that its symptoms are often not pronounced, and the patient may not be aware of the presence of chlamydia for a long time.
Sexual route: vaginal, anal and oral
! Chlamydia is a sexually transmitted disease and can therefore be contracted during unprotected vaginal or anal intercourse. There is a possibility of transmission of chlamydia through oral sex, which increases significantly in the presence of damage to the mucous membranes.
Is it possible to become infected with chlamydia if “it only happened once”? Clinical studies show that transmission of chlamydia occurs in 30-50% of cases of unprotected sexual contact, if sexual intercourse with an infected partner occurs no more than once. When chlamydia is detected in a person, it is imperative to check a regular sexual partner, since the risk of infection with regularly repeated sexual intercourse is almost 100%.
During childbirth
. There is a high risk of transmitting chlamydia from mother to child during childbirth, when the newborn passes through the birth canal. In this case, infection of the eyes and mouth occurs.
Household way
. In the external environment, the parasite can remain viable for 2 days, but it is sensitive to temperature conditions, surviving only at temperatures from 16 to 22 degrees. Therefore, there is a risk of household infection through dirty dishes, toilet seats, etc. is low, however, cases of infection through this route have also been observed. Including a small percentage of infections occurs due to the transmission of bacteria when visiting a bathhouse or sauna, since in the humid and cool environment of the dressing room, chlamydia feels “at home.”
First pharmaceutical aid
Pharmacists can easily “calculate” the treatment regimen for chlamydia in a prescription. Often, in addition to antibiotics, it includes local antiseptic drugs (vaginal suppositories, irrigation solutions), as well as probiotics. The pharmacist's task is to tactfully serve the patient without revealing that his secret has been exposed, and, if necessary, to offer a synonymous replacement. It would seem that the role of the leader is over. But it was not there.
There is a special category of patients among pharmacy clients who exhibit excessive zeal. They have a detrimental tendency to modify the course of treatment prescribed by the doctor. The ever-memorable compliance inexorably falls down and drags down the effectiveness of anti-chlamydial therapy. At this moment, a lot depends on the chief captain, who can warn the client in time against a rash step. And the small contribution of an ordinary pharmacist to the treatment of a stubborn disease may force the statistics to change vector.
Symptoms
The incubation period of infection ranges from – 1 week to – 2 months, during which time the infection spreads in the body. In 45% of men and 65% of women, the disease does not give any manifestations during this period and can only be detected through laboratory testing of biomaterials.
With acute chlamydia, men and women experience different symptoms. At the same time, the female body is more susceptible to infection - infection occurs faster and the consequences are more serious.
Immunomodulators
Treatment of chlamydia is complicated by the fact that during the period of illness the immune system is suppressed. Not all patients need to take immunomodulators, so it’s not worth injecting them on the basis of “it won’t get worse.”
For immunocorrection the following is prescribed:
- Immunomax – enhances protection against bacterial infections, injections in the first and last 3 days of the course;
- Erbisol – protects the liver from the toxic effects of antibiotics, 2 times for 20 days;
- Polyoxidonium – promotes comprehensive protection against infections, has detoxification properties, 10 injections every other day.
How does chlamydia manifest in women?
Manifestations of chlamydia in women at various stages of infection boil down to the following symptoms:
- Vaginal discharge. They have a mucous structure and may contain pus. May have an unpleasant, pungent odor.
- Pain appears during urination, a cutting or burning sensation.
- During menstruation, sharp pain in the genital area may occur.
- The appearance of bleeding between menstruation, the blood can be either pure or mixed with mucus.
- Low-grade fever, general weakness of the body, similar to the sensations during a cold.
Even one of the symptoms is an alarm bell, in which case you should definitely contact a gynecologist and get tested for chlamydia.
Which doctor will diagnose and treat chlamydia?
Patients often want to know which doctor should help them if symptoms appear that resemble chlamydia, caused by the trachomatis bacterium.
The question is also often asked about which institutions will conduct the examination and subsequent therapy.
In fact, chlamydia belongs to the STD group of infections.
This means that, first of all, a venereologist will deal with a person with this disease.
It is within his competence that the choice of diagnostic measures, methods of treatment and prevention of the disease lies.
You can find a venereologist either in a clinic or in a skin and venereology clinic.
There is also the option of seeking help at a private clinic, but there will be a fee for examination and treatment.
In addition to a venereologist, the patient can always seek help from a urologist or gynecologist.
Both doctors, working with diseases of the genital organs, to one degree or another encounter chlamydia during their practice.
This means they know how to diagnose and treat the disease, if necessary.
In rare cases, other specialists are additionally involved in therapy.
This could be an immunologist-allergist, an infectious disease specialist, a therapist and other doctors.
It all depends on what symptoms bother a particular patient.
How does chlamydia manifest in men?
In men, the manifestation of chlamydia is comparable to the symptoms of urethritis, and in the first stages, many do not pay attention to the problem, believing that everything is caused by inflammation after a cold or other “trifling” factors.
Chlamydia in men can cause the following symptoms:
- Transparent mucous discharge from the urethra.
- The presence of pus in the urine and its cloudiness.
- The color of the urine changes, and bloody discharge may appear, which may also be present in the seminal fluid during ejaculation.
- Urination is accompanied by a burning or stinging sensation.
- Spontaneous pain appears in the pelvic area, lower back, and scrotum.
- A low-grade fever is observed (the temperature rises from 37.1 to 38 degrees).
- General physical malaise.
It happens that chlamydia in men forms local colonies without general infection of the body. Focal accumulations without the development of an infectious disease are caused by strong immunity and antibody resistance to the effects of chlamydia. However, the man remains infectious.
What will happen if left untreated?
The consequences of chlamydia in men occur when the necessary therapy was not carried out, or if it was insufficient and ineffective, these are:
- Orchitis and orchiepididymitis. Chlamydia affects either the testicle or the testicle along with the epididymis.
- Reiter's syndrome. Simultaneous damage to the skin, joints and mucous membrane of the eyes.
- Funiculitis and vesiculitis. The spermatic cord and seminal vesicles are involved in the process of inflammation.
- Epididymitis. Inflammation of the epididymis. Characterized by high temperature and an increase in the volume of the appendage. The inflammatory process disrupts spermatogenesis and leads to infertility. Often occurs in parallel with orchitis (inflammation of the testicle).
- Urethritis with subsequent urethral strictures. The man will experience a frequent urge to urinate, and uncharacteristic discharge with pus and mucus will begin to appear from the urethra.
- Prostatitis. Against the background of chlamydia, the prostate gland becomes inflamed, urination is difficult, pain in the groin and lower back, and watery discharge appear. The prostate becomes sensitive to touch, painful, heterogeneous structure.
In addition to these numerous inflammations of the genitourinary system, chlamydia can affect other organs. With an ascending infection, the pathological process may involve the kidneys, peritoneum, and liver. Therefore, high-quality diagnosis of the disease and its timely treatment are so important.
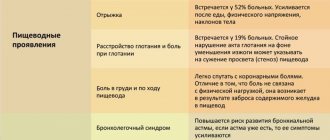
Oral chlamydia and its symptoms
When infected with chlamydia during oral sex or when transmitting bacteria through household means through dishes, etc. Oral chlamydia develops, affecting the oral cavity, throat, and nasopharynx. In this case, the following symptoms of the disease may be observed:
- Constant bad breath.
- The nasopharynx becomes covered with mucous deposits.
- Gradually, the mucus moves to the upper palate and tongue.
- There is nasal congestion and difficulty breathing.
- Enlarged tonsils, swelling of the back of the throat.
- Loss of taste due to mucus on the taste buds of the tongue.
- Pain when pressing on the mucous membrane of the throat, palate or tongue.
- Difficulty breathing due to a swollen throat.
- Attacks of suffocation most often occur in the evening or during hot periods.
Over time, the patient loses taste sensitivity, and eating is accompanied by pain that appears when food passes through the sore throat. A constant unpleasant sensation in the mouth develops. Spasmodic, involuntary twitching of the tongue is acceptable.
Since the symptoms of chlamydia are quite vague and often resemble manifestations of other diseases, it is necessary to consult a doctor in case of any abnormalities (discharge, itching, burning). For women it is a gynecologist, for men it is a urologist.
Preparation for testing for chlamydia trachomatis
Preparation for analysis largely depends on what material and where it will be taken from in order to perform the diagnosis.
If you plan to do an ELISA, a blood test will be taken from a vein from the patient.
The procedure is standard and does not present any difficulties.
The recommendations are simple:
- do not eat food before taking the test,
- visit the clinic to collect material in the morning,
- stop taking alcohol and antibiotics a few days before the test.
A smear from the urethra in both women and men usually requires more careful preparation.
It is necessary to refrain from sexual intercourse and the use of hygiene products for treating the genitals.
You will also have to avoid urinating for at least 3-4 hours.
Since a smear from the urethra is a painful procedure for men, they can replace this method of obtaining biological material with collecting sperm or urine.
It is also possible to detect chlamydia in both biological fluids.
Complications
Chlamydia often causes serious illnesses, which are a complication of the disease if treatment is improper or ineffective. In particular, the following consequences were identified:
- Reiter's syndrome
is the most serious complication, during which symptoms of urethritis, conjunctivitis and arthritis develop. In the final stages, joint deformation occurs - the cause of disability for life. - Orchiepididymitis
- a disease fraught with male infertility due to the destruction of Leydig cells, which contribute to the spermogenesis procedure. - Urethral stricture
- due to the appearance of scars on the tissue caused by the attack of chlamydia, the urethra narrows and is pinched, resulting in sharp pain when urinating. To correct the situation, surgical intervention is performed. - Chronic prostatitis
- chlamydia has a complex negative effect on the prostate, promotes narrowing of the ducts, reduces the production of prostate secretions, lowers the level of testosterone production, which leads to a decrease in potency.
The complications described above appear in the stages of advanced chlamydia if treatment is not started on time. In most cases, complications can be avoided.
Ways to get rid of chlamydia
The doctor prescribes treatment for patients only after the diagnosis has been accurately established.
This is due to the fact that the symptoms of STDs are very similar to each other.
Unfortunately, it is not possible to distinguish them without special diagnostics.
Patients are often interested in how to treat chlamydia trachomatis in women and men.
First of all, it is worth considering that you will have to use antibacterial drugs.
Because only they can destroy bacteria that have already entered the body.
Antibiotics of the fluoroquinolone, tetracycline, macrolide series, such as Azithromycin, Levofloxacin, etc., are suitable.
Doctors often prefer a course of two antibiotics, which can be supplemented with Metronidazole.
To increase the effectiveness of treatment, it is recommended to use drugs from the group of immunomodulators.
Their task is to strengthen the immune system and help it actively eliminate the infection.
For example, Polyoxidonium or Immunomax can be used as an immunomodulator.
After the acute process subsides, the doctor may add physical therapy to the treatment.
It will help the body recover faster and contribute to the normalization of functions lost due to illness, if they are not lost irretrievably.
Chlamydia during pregnancy
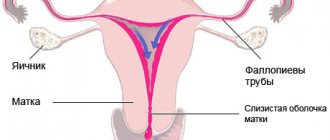
Chlamydia has a serious impact on the course of pregnancy and can cause a wide range of problems and malfunctions in the female body. Depending on at what stage of pregnancy chlamydia began, you may encounter the following consequences:
- Blastopathy – the death of the fertilized egg occurs, which ends in a frozen pregnancy or miscarriage.
- Embryopathy – abnormalities in the development of the fallopian tubes;
- Premature birth.
- Ectopic pregnancy.
If chlamydia was suffered before pregnancy, it can cause failure of nidation of the fertilized egg, which in the vast majority of cases leads to female infertility. Taking into account all the risks, testing for chlamydia is mandatory when planning pregnancy, as well as at various stages of bearing a child, if signs and symptoms of the presence of chlamydia in the body appear.
Even if chlamydia did not cause significant problems during pregnancy, chlamydia can be passed on to the baby during childbirth. The most serious complication in newborns resulting from maternal chlamydia is neonatal chlamydial pneumonia. This disease is difficult to treat, has many complications and high mortality statistics. Children born to a mother with chlamydia must be tested for infection between 1 and 3 months of age.
Treatment of uncomplicated infection
Treatment of urogenital chlamydia depends on the severity and extent of the process. If, against the background of infection with C. trachomatis, inflammatory diseases of the lower genital tract are detected - inflammation of the cervix (cervicitis), urethra (urethritis) or epididymis (epididymitis), then they speak of an uncomplicated chlamydial infection. Then the drugs of choice are azithromycin or doxycycline. By the way, studies have proven that azithromycin and doxycycline are equally effective. The effectiveness of first-line drugs in the treatment of uncomplicated urogenital chlamydia is 97–98%. Dual therapy with azithromycin and doxycycline is recommended for simultaneous infection with chlamydia and gonorrhea.
An alternative treatment regimen for chlamydial infection that is indicated when first-line drugs are intolerant or ineffective includes erythromycin or levofloxacin or ofloxacin. Sometimes preference is given to josamycin. The wide availability of generic azithromycin, moderate cost and high compliance (voluntary adherence by the patient to the prescribed treatment regimen) have become the basis for their mass use. Azithromycin is considered to be a more cost-effective treatment for chlamydia infection than alternative drugs. Erythromycin is less effective than azithromycin and doxycycline, mainly due to frequent gastrointestinal side effects, which may cause decreased compliance. Levofloxacin and ofloxacin have comparable efficacy to azithromycin, but are more expensive. Other fluoroquinolones have either been found to be ineffective in treating chlamydial infections or their use in such cases has not yet been fully studied.
How is chlamydia diagnosed: tests for chlamydia
To date, several effective methods for diagnosing chlamydia have been developed, which make it possible to determine the presence of an infectious pathogen even if it is present in the sample in minimal quantities. A smear, scraping from the surface of the genital organs, blood, seminal fluid, etc. can be used as the test material. Diana Medical Center does not use rapid tests to diagnose chlamydia, which provide false results.
Basic and most highly effective techniques.
- Immunofluorescence reaction (RIF);
- Enzyme-linked immunosorbent assay (ELISA);
- Polymerase chain reaction (PCR);
- Culture for chlamydia.
General smear (the probability of detecting the presence of chlamydia in this way is no more than 15%, so the use of this analysis is not effective, but it will help to identify concomitant infections that aggravate the problem). Read about tests for chlamydia here.
Striving for maximum accuracy and information content, preference is given to high-tech methods:
Enzyme-linked immunosorbent test (ELISA)
The technique makes it possible to fairly accurately determine the stage of the disease and chlamydial origin, as well as the presence of microorganisms in other organs not related to the genitourinary system. It has a relatively high research accuracy - up to 60%. It can be effectively carried out only after the development of specific antibodies to chlamydia has begun - 5-20 days from the moment of infection.
This is due to the fact that ELISA and RIF - enzyme-linked immunosorbent assay and immunofluorescence reaction research are not aimed at identifying the causative agent of chlamydia itself, but at detecting specific antibodies to this particular antigen. This is achieved through the controlled formation of antigen-antibody complexes, which in the case of the RIF method are labeled with a fluorescent substance, which makes the resulting complexes luminous. This makes them easier to detect during microscopic examination of the material.
During the research, the concentration of antibodies of the IgM, IgA, IgG groups produced by the body during protection against chlamydial infection at different stages of infection of the body is determined. The research takes quite a bit of time and is inexpensive.
Polymerase chain reaction (PCR)
The PCR method is highly effective and allows us to say with 100% probability whether there is chlamydia in the body or not. The study is based on the technology of detecting chlamydia DNA in a sample taken - scraping from the urethra, prostate secretion, ejaculate, urine sediment, saliva, blood and other biomaterials. Determining the results, depending on the equipment used, takes up to 3 days.
By triggering the reaction of duplicating DNA segments, a specialist can, in a short period of time, obtain the genetic chain of an infectious pathogen that is a million times longer in comparison with the primary segment. This allows chlamydia to be identified with 100% accuracy.
The technique is highly accurate; obtaining incorrect results is only possible if the sampling technology or transportation of the biomaterial is violated.
Chlamydia culture
Microbiological testing is 90% accurate in identifying chlamydia in the body.
By inoculating a sample of biological material on a special nutrient medium and creating favorable conditions for reproduction and growth, after some time it is possible to obtain a full-fledged colony of the pathogen. In this case, it is not difficult to identify the infection by simple microscopic examination. The advantage of this technique is the possibility of testing the sensitivity of the pathogen to various antibiotics. This allows you to choose the most effective drug for the treatment of chlamydia.
Diagnostics
Diagnosis of chlamydia is difficult because Chlamydia trachomatis is an intracellular parasite. To diagnose chlamydia, they do not take a smear (mucus and discharge), but a scraping (cells of the diseased organ). Diagnosis also includes observing the patient's clinical symptoms. Laboratory tests are carried out on smears from the cervix, scrapings from the urinary canal, and the first morning portion of urine. Most often, the study is carried out using the PCR (polymerase chain reaction) method. Additionally, a blood test is performed using ELISA (enzyme-linked immunosorbent assay) to determine the presence of immunity to chlamydia. ELISA is an auxiliary test that helps establish an accurate diagnosis, since antibodies to Chlamydia trachomatis can also be detected in healthy people. The presence of antibodies can be due to both a previous disease (“serological trace”) and cross-reactions with respiratory chlamydia.
Treatment of chlamydia
Since the causative agent of chlamydia is an intracellular bacterium, antibacterial drugs are used in the treatment of the disease (etiotropic therapy). Antibiotics are selected that destroy microorganisms of the identified group. Only a competent specialist can prescribe suitable medications based on the tests performed and after identifying the type of chlamydial bacteria, the affected area and the progress of the disease.
In addition, if there are concomitant infections, antibiotics, antifungals, and immunomodulators can be used. If there is a large amount of discharge, antimicrobial agents will be required.
As a rule, drugs are prescribed in the form of tablets, injections, and can be used locally in the form of vaginal suppositories for women. In most cases, several medications and auxiliary agents are combined, which also reduce the possibility of developing complications or intoxication of the body. Treatment is carried out at home. After completing the course of therapy, after 2-3 weeks a repeat test for chlamydia is done and if no bacteria are found, the treatment can be considered successful.
An important nuance is the need to notify the sexual partner about the presence of chlamydial infection, since with a high probability the partner may be infected with chlamydia, which will also require treatment using the same drugs and techniques. Doctors recommend that both partners be tested at the same time and treated together. This will avoid secondary infection.
Unique chlamydia
The song-sounding name Chlamydia trachomatis is a round, gram-negative intracellular bacterium with an unusual life cycle. It ensures the existence of the microorganism both inside and outside the cell. In the extracellular environment, chlamydia lives in the form of so-called elementary bodies, which resemble spores more than bacteria. Once inside the cell, C. trachomatis turns into an active pathogen, capable of producing its own DNA and RNA and carrying out large-scale destructive work. The intracellular form of chlamydia is called the “reticular body.” The ability of chlamydia to exist inside cells has confused scientists for many years. Because of it, researchers for decades could not decide which type of microbe to classify Chlamydia trachomatis. But even now, when this secret has long been revealed, chlamydia continues to surprise.
According to WHO data for 2011, 101 million new cases of chlamydial infection are detected annually.
Prevention of chlamydia
To reduce the risk of chlamydia and the development of chlamydia, it is recommended to adhere to simple rules of personal and intimate hygiene, as well as caution in choosing sexual relations. Protect against chlamydia:
- Using a condom during sexual intercourse.
- Refusal of casual relationships in favor of one permanent partner.
- Compliance with the rules of personal intimate hygiene, especially after visiting public baths and saunas.
It is recommended to be tested annually for chlamydia and other sexually transmitted infections (STIs, STDs) and non-sexually transmitted infections. It is also mandatory to take the test when planning a pregnancy and repeat it during pregnancy.
The use of contraception and compliance with moral standards when engaging in sexual activity will significantly reduce the risk of infection with chlamydia and the subsequent development of chlamydia in men and women.
Antibiotics
The main role in the treatment of chlamydia is given to antibiotics. Represented by 3 pharmacological groups: tetracyclines, macrolides, fluoroquinolones.
Tetracyclines
Contraindicated during pregnancy and lactation; not prescribed to children under 14 years of age. Doxycycline, Unidox Solutab and Vibramycin are indicated for uncomplicated forms of infection (urethritis, cervicitis). Doxycycline is taken only twice a day, but causes nausea and vomiting in many patients.
Macrolides
The group is represented by a wide range of drugs that are highly effective (97%) against mixed infections (mycoplasma, gonococcus, Treponema pallidum) and are safer than tetracyclines. These include:
- Erythromycin – has increased biological activity, but causes digestive upset (2 times a day for 10 days);
- Rovamycin – has low toxicity (3 times a day for 10 days);
- Sumamed - used for combined infections (chlamydia + syphilis or gonorrhea), a “loading” dose (1000 mg) is taken on the first day, in the next 5-7 days 500 mg;
- Rulid – inhibits chlamydia and ureaplasma, taken 2 times a day for 14 days;
- Klacid - used for long-term ureaplasmosis and chlamydia, it can be administered intravenously (2 days), then orally (10-12 days).
Fluoroquinolones
They are prescribed less frequently than those listed above, as they have increased toxicity. Ofloxacin, Tsiprolet, Abaktal are used for the treatment of combined, chronic infections: chlamydia, gonococcus, gardnerella, mycoplasma.
Difficulties in treating chlamydial urethritis
The content of the article
Due to the frequent coexistence of chlamydial urethritis with other sexually transmitted diseases, especially gonorrhea, and also due to the mild or even asymptomatic course of the infection, its treatment remains a big problem.
Additional difficulties in determining the appropriate dose and duration of treatment with an appropriately selected antibiotic are created by the cycle of intracellular development of chlamydia with the presence of infectious elementary and non-infectious reticular bodies and the possibility of their survival in the submucosal tissue.
Why you can’t use folk remedies for chlamydia
Today, there is a widespread fashion in the world for folk remedies.
People mistakenly believe that with the help of various herbal recipes, any disease can be cured with fewer side effects.
Unfortunately, this is not the case, and chlamydia is a great example of this.
Herbs, suppositories based on natural ingredients and other similar products cannot help in the fight against pathogenic microorganisms.
This must be remembered once and for all.
Folk remedies do not have sufficient pharmaceutical activity to destroy pathogenic microorganisms.
They will simply slow down their reproduction or transform the infection into a chronic latent form.
One of the most common reasons for treatment failure is precisely the fact that patients try to be treated using folk remedies.
Frankly disregarding the recommendations given to them by the attending physician.
As a result, the disease constantly recurs, each time causing more and more significant damage to the already weakened immunity.
The symptoms of the disease also become brighter with each relapse.
ethnoscience
There are so-called traditional methods of treating chlamydia:
- douching with garlic infusion;
- using garlic water tampons;
- drinking alcohol tincture with boron uterus;
- eliminating dairy products from the diet;
- starvation.
The effectiveness of these methods is controversial. For example, douching is considered harmful by many doctors, because it washes away all microflora and makes the mucous membrane defenseless against any pathogenic microorganisms. If you plan to try any of the above, be sure to consult your doctor.
Why local antiseptics are not effective against chlamydia
A number of patients are interested in the question of whether miramistin and chlorhexidine are effective in combating such an unpleasant infection as chlamydia trachomatis.
The doctors' answer is quite clear.
These drugs, which have a local antiseptic effect, do not have a full therapeutic effect.
And, contrary to popular belief, they cannot serve as a replacement for antibiotics.
It is a mistake to use only miramistin or chlorhexidine to treat an infection, refusing to use antibacterial agents.
After all, antiseptics, unlike antibiotics, cannot penetrate into the affected cells.
And they destroy only those pathogenic microorganisms that are on the surface of the epithelial layer.
As a result, there is no cure.
However, antiseptics can be used to speed up therapy and improve the effect of antibacterial agents.
Moreover, these drugs can act as protection against secondary infections.
They are often activated during the period of treatment of the underlying disease due to the fact that the body’s resistance decreases significantly.
Antiseptics can be used not only for external treatment of the genital organs, but also for instillation into the urethra for deeper cleansing.