Uterine bleeding is the discharge of blood from the vagina, characterized by abundance and duration. This pathological condition poses a danger to the life and health of a woman and is a sign of serious diseases of the reproductive system. To save the patient, it is important to immediately provide her with first aid and find out the cause of the bleeding. Natural bleeding from the vagina is called menstruation. Menstrual bleeding is characterized by cyclicity and repeats at regular intervals. The period between menstruation usually lasts 25–30 days. Blood from the vagina should not be released longer than 8 days, otherwise we can talk about pathology. Menstrual irregularities are a reason to immediately consult a gynecologist. The doctor will find out the cause of the pathological phenomenon and help get rid of the disease at an early stage, before complications arise.
What is dysfunctional uterine bleeding?
- dysfunctional uterine bleeding of the juvenile period - between the ages of 12 and 18 years;
- dysfunctional uterine bleeding of reproductive age - develops in women 18-45 years old;
- dysfunctional uterine bleeding of the premenopausal (menopausal) period - occurs during menopause (45-55 years).
According to the criterion of the presence or absence of ovulation, dysfunctional bleeding is:
- ovulatory;
- anovulatory (80% of cases).
According to statistics, uterine bleeding is the most common pathology of the female reproductive system.
Causes of dysfunctional uterine bleeding
Dysfunctional uterine bleeding is a consequence of a violation of the hormonal regulation of ovarian function by the hypothalamic-pituitary system. Due to impaired secretion of luteinizing and follicle-stimulating hormones of the pituitary gland, which are responsible for follicle maturation and ovulation, disruptions in folliculogenesis and menstrual function are observed. In this case, the ovary can either ripen, but without ovulation, or not ripen, that is, the corpus luteum does not form in any case.
As a result of these pathological processes, the female body is in a state of hyperestrogenism - progesterone is not synthesized in the absence of the corpus luteum, and the uterus is exposed to estrogen. A disruption of the uterine cycle occurs when the endometrium grows greatly (hyperplasia), and then is rejected. Because of this, uterine bleeding becomes severe and prolonged. Dysfunctional uterine bleeding may stop on its own, but usually reappears after some time. Therefore, it is very important to exclude recurrence of the disease.
Causes of juvenile dysfunctional uterine bleeding
During puberty, dysfunctional bleeding occurs more often than other gynecological pathologies (in 20% of cases). Their reasons are:
- mental/physical trauma;
- avitaminosis;
- overwork;
- dysfunction of the thyroid gland/adrenal cortex;
- childhood infections (measles, chicken pox, rubella, whooping cough);
- Acute respiratory infections, chronic tonsillitis.
Causes of dysfunctional uterine bleeding during reproductive age
In women of reproductive age, the disease occurs less frequently - in 5% of cases. Its development is led by:
- climate change;
- intoxication poisoning;
- infectious diseases;
- harmful working conditions;
- abortions;
- medications that cause disorders at the level of the hypothalamic-pituitary system.
Causes of dysfunctional uterine bleeding in the premenopausal period
During menopause, dysfunctional uterine bleeding occurs in 15% of cases from other gynecological pathologies. Gynecologists explain their occurrence by the fact that with age, the pituitary gland produces fewer gonadotropins and does so irregularly. This, in turn, causes disturbances in the egg cycle (formation of the corpus luteum, ovulation, folliculogenesis). Due to a lack of progesterone, the endometrium begins to grow. Its rejection leads to severe uterine bleeding.
First emergency aid before doctors arrive
Heavy bleeding from the vagina must be stopped or at least reduced before doctors arrive. This is a matter of life and death for a woman. In most cases, with proper first aid, bleeding stops, but in 15% of cases the pathological process ends in death.
Every woman should know how to help herself before the doctors arrive, what she can do and what she can’t do.
A sick woman, while waiting for doctors at home, should do the following:
- lie on your back, remove the pillow from under your head;
- place a high cushion made of towels or a blanket under your shins;
- Place a cold water bottle or an ice-filled heating pad on your stomach;
- drink cold still water.
It is strictly prohibited:
- be in a standing and sitting position;
- lie with your legs pressed to your stomach;
- take a hot bath;
- do douching;
- put a heating pad on your stomach;
- drink hot drinks;
- take any medications.
Symptoms of dysfunctional uterine bleeding
In young girls and women of childbearing age, dysfunctional uterine bleeding has the following symptoms:
- Bloody discharge from the genital tract appears outside of menstruation. Their color can range from red to dark burgundy. May be abundant and contain clots.
- Before bleeding, menstruation may be delayed for several weeks (up to one month).
- The duration of menstruation increases by 3-4 days, the discharge during the “extra period” is spotting.
- The menstrual cycle is not regular.
- A woman complains of increased fatigue, dizziness, and pale skin.
During premenopause, dysfunctional uterine bleeding manifests itself:
- irregular, prolonged bleeding that occurs after menstruation (menometrorrhagia);
- regular uterine bleeding with an interval of up to 21 days (polymenorrhea);
- frequent, long and heavy menstruation (hypermenorrhea);
- intermenstrual bleeding (metrorrhagia).
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Hygiene as a prerequisite for successful recovery
It is no secret that compliance with hygiene standards, especially in the intimate area, is the key to the health of not only the woman herself, but also her partner and offspring. The rules of personal hygiene are learned in early childhood and subsequently must be strictly observed throughout life.
Expert opinion
Today, modern methods of maintaining natural cleanliness may differ significantly from those used by our mothers and grandmothers. Refusal of soaps with a high alkali content, the use of hypoallergenic sanitary pads, special compositions for treating the intimate area based on mild ingredients - all this ensures comfort and health for many years.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
The Ginocomfort series of intimate hygiene products is not just detergent and soothing compositions - it is the result of long-term research, careful selection of components, strict compliance with the recipe and quality control. Using Gynocomfort intimate hygiene gels, you will forget about irritation, provide powerful antibacterial protection to the body and comfort for a long time. This is especially important for uterine bleeding caused by myomatous formations. The secreted blood is a breeding ground for a large number of bacteria. It quickly coagulates, an unpleasant odor appears, hyperemia appears on the skin and mucous membranes, a burning sensation occurs, and pustular lesions appear.
To eliminate discomfort from uterine bleeding and prevent bacterial infection, you should use the following products from the popular Gynocomfort series:
- Revitalizing intimate gel - suitable for eliminating vaginal discomfort. Restores the natural balance of the skin in the intimate area and the microflora of the mucous membrane after suffering from inflammatory diseases.
- Washing gel for intimate hygiene “Basic care” - provides comfort and safety, is suitable for daily use and does an excellent job of protecting against the development of pathogenic microflora on the vaginal mucosa.
All Gynocomfort products are great for women of any age and with any health condition, can be combined with any therapy and are indispensable during the recovery period.
Intimate gel for women's health
Diagnosis of dysfunctional uterine bleeding
In addition to listening to the patient’s complaints, gynecological examination and ultrasound diagnosis of the pelvic organs, recognizing dysfunctional uterine bleeding involves the use of additional research methods. So, if we are talking about examining girls of juvenile age, the following is carried out:
- taking a blood test for hormones and coagulation;
- hysteroscopy.
Diagnosis of dysfunctional uterine bleeding in reproductive age includes:
- exclusion of organic pathologies of the genitals (spontaneous abortion, endometriosis, tumor neoplasm, ectopic pregnancy, etc.);
- hysteroscopy;
- curettage of the endometrium for histological examination of the material.
When diagnosing dysfunctional bleeding in women of menopausal age, gynecologists determine whether bloody discharge from the genital tract is another menstruation (since menstruation can sometimes begin at this age). Additionally, hysteroscopy and diagnostic curettage are performed. If there is a suspicion of a tumor, the doctor prescribes a computer or nuclear magnetic tomography to the patient.
Bloody discharge during pregnancy
Light spotting is common in the early weeks of pregnancy, but heavy bleeding can occur in the third trimester of pregnancy and poses a serious risk to both mother and fetus.
The severity of bleeding is assessed by:
- volume - small drops or real bleeding;
- duration;
- blood characteristics;
- accompanying symptoms.
There are many reasons for bleeding during pregnancy, including:
- urinary tract infections or hemorrhoidal disease (bleeding in which is misunderstood as blood loss of genital origin);
- polyps in the cervix;
- cervical carcinoma;
- placenta previa (abnormality of the placenta);
- placental abruption before childbirth;
- abortion (miscarriage);
- ectopic pregnancy (the embryo, instead of implanting in the uterus, implants in other areas, especially often in the fallopian tubes);
- gestational trophoblastic disease.
Polyps in the cervix
Both in the presence of bloody discharge and in case of more significant blood loss, the patient is always recommended to consult a doctor. If spotting in the first trimester is physiological in nature, when the bleeding was especially heavy, hospitalization would become mandatory.
Almost always in the third trimester of pregnancy, therapeutic treatment includes:
- If the presentation is mild, close monitoring of symptoms is necessary until vaginal delivery eventually occurs;
- If the clinical picture is severe, emergency treatment with continuous cardiotocography (for fetal monitoring) and immediate cesarean section should be performed.
Intense bleeding in the first weeks after childbirth or after an abortion can occur when the uterus has not yet restored its physiological size, or in case of imperfect (insufficient) cleaning of the internal walls.
How to stop dysfunctional uterine bleeding - treatment of pathology
Treatment of dysfunctional uterine bleeding consists of hemostatic measures. In this case, both conservative and surgical methods can be used. The choice of method to stop uterine bleeding in women of juvenile and reproductive age depends on the amount of blood loss:
1. If the hemoglobin level is above 100 g/l (moderate anemia), symptomatic treatment is used. It includes the use of the following drugs:
- Dicynone;
- Vikasol;
- Ascorutin;
- Aminocaproic acid;
- Oxytocin.
If the tablets are ineffective, hormonal drugs containing progesterone are selected. It can be:
- Non-ovlon;
- Marvelon;
- Mercilon;
- Rigevidon.
As a result of their use, dysfunctional uterine bleeding stops after 5-6 days.
2. If the hemoglobin level is less than 70 g/l (severe anemia), hysteroscopy with separate diagnostic curettage and pathomorphological examination of the scraping are performed. Afterwards hormones are prescribed.
Iron supplements, vitamins B12, B6, C, P, and folic acid also help normalize the condition of a woman suffering from bleeding. In some cases, the question arises about transfusion of fresh frozen plasma and red blood cells.
To exclude the re-development of uterine bleeding, it is recommended to take low doses of Norkolut, Novinet, Silesta, Logest, Duphaston.
Treatment of the disease in menopausal women is aimed at suppressing menstrual and hormonal functions. In this case, a surgical method is used - hysteroscopy and therapeutic and diagnostic curettage. Conservative homeostasis in such a situation is not capable of normalizing a woman’s condition. In especially severe cases, gynecologists perform cryodestruction of the endometrium or supravaginal amputation of the uterus.
Treatment of dysfunctional uterine bleeding with folk remedies
Of the folk recipes to stop dysfunctional uterine bleeding, women can resort to:
- Nettle decoction. 1 tbsp. dry leaves pour a glass of boiling water. Cook for 10 minutes over low heat. Strain. Take 1 tbsp. 5 times a day
- Orange decoction. Pour the peels of 6 oranges into 1.5 liters of water. Cook over low heat until most of the water has evaporated. Take 2 tbsp. 3-4 times a day.
- Infusion of cucumber lashes. Cut off the vines remaining after harvesting, chop them finely, and wash them. Pour 100 grams of greens into 2 glasses of water and boil. Drink 1/2 glass 3 times a day.
Any traditional recipe must be previously agreed with your doctor.
Drug therapy
Treatment of diseases that cause bleeding from the uterus is carried out in a hospital setting. Additionally, the doctor prescribes medications to the patient to help stop bleeding. Hemostatic medications are taken only on the recommendation of a medical specialist; taking medications at your own discretion is strictly prohibited. Below is a list of medications most commonly used to stop bleeding.
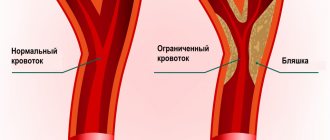
- Etamsylate - This drug stimulates the synthesis of thromboplastin and changes the permeability of blood vessels. Blood clotting increases, resulting in decreased bleeding. The medication is intended for intramuscular injection.
- Oxytocin is a hormonal drug often used during labor to improve uterine contractility. As a result of contraction of the uterine muscles, bleeding stops. The drug oxytocin is prescribed for intravenous administration with the addition of glucose and has a large list of contraindications.
- Aminocaproic acid - This medicinal substance prevents blood clots from dissolving under the influence of certain factors, thereby reducing bleeding. The medicine is either taken orally or administered intravenously. Treatment of uterine bleeding with aminocaproic acid is carried out under close medical supervision.
- Vikasol - The drug is based on vitamin K. With a deficiency of this vitamin in the body, blood clotting worsens. The medication is prescribed to patients who have a tendency to uterine bleeding. However, vitamin K begins to act only 10–12 hours after entering the body, so it is not advisable to use the drug to stop bleeding in emergency cases.
- Calcium gluconate - The drug is prescribed for calcium deficiency in the body. Deficiency increases the permeability of vascular walls and impairs blood clotting. This medicine is also not suitable for use in emergency cases, but is used to strengthen blood vessels in patients prone to bleeding.
Danger
Dysfunctional uterine bleeding is not a harmless disease. During the juvenile period it can lead to:
- anemia;
- hormonal disorders;
- infertility;
- endometriosis.
In women of reproductive age, the disease can be caused by:
- infertility;
- anemia;
- endometrial cancer, breast cancer;
- fibrocystic mastopathy;
- uterine fibroids.
In premenopausal and menopausal patients, dysfunctional uterine bleeding can cause anemia, cancer, and also cause the growth of existing tumors into neighboring organs. from a gynecology clinic at the first symptoms of the disease.
.
About the disease
Gastrointestinal bleeding is an extremely dangerous sign. We are talking about the leakage of blood that comes out of damaged vessels and enters the organs of the gastrointestinal tract. Bleeding is considered a complication of inflammatory and chronic diseases. It is often caused by alcohol and drug intoxication of the body.
The sources of hemorrhage are the stomach, intestines, and esophagus. The disease is as common as appendicitis. Often this phenomenon occurs as a complication of duodenal ulcers, chronic gastritis, and the appearance of neoplasms.
We recommend diagnosing gastrointestinal bleeding at the medical institution “KDS Clinic”. All examinations are carried out using modern technical equipment and innovative techniques. The disease will be diagnosed even at an early stage.
Prevention
Prevention of dysfunctional uterine bleeding consists of:
- regular visits to a gynecologist;
- submitting a smear once a year for oncocytology;
- competent treatment of gynecological diseases;
- exclusion of abortion;
- reduction of psycho-emotional and physical stress;
- maintaining a menstrual calendar;
- proper nutrition.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Let's sum it up
As we have already found out, there can be quite a few reasons for the occurrence of uterine bleeding due to fibroids. Obvious symptoms and a wide range of treatment options make it possible to effectively combat the painful condition, but only if you seek medical help from specialists in a timely manner. No self-medication should be allowed in this condition! Neither self-administration of drugs to improve blood clotting, nor herbal medicine, nor hormone therapy carried out without careful medical supervision will give positive results.
Any delay in diagnosing and treating uterine bleeding can lead to loss of health and even become life-threatening.
Do not hesitate to regularly contact the antenatal clinic for a routine examination. Timely detection of myomatous nodes and monitoring the condition will help to avoid problems and prevent heavy blood loss. Sources:
- Ailamazyan E.K. Emergency care for extreme conditions in obstetric practice. – St. Petersburg, 2003.
- Bodyazhina V.I., Zhmakin K.N., Kiryushchenkov A.P. Obstetrics. - M.: Medicine, 1986. – 496 p.
- Gynecology: Textbook / Ed. G.M. Savelyeva, V.G. Breusenko. - M.: GEOTAR-MED, 2004. - 480 p..
- Bokhman Y.V. Guide to gynecological oncology, L.: Foliant, 2002.
- Malevich K.I., Rusakevich P. Treatment and rehabilitation for gynecological diseases. – Minsk, 1994. – 367 p.