Dental periodontitis is an inflammation of an infectious nature that occurs at the membrane of the tooth root and affects the tissues of the oral cavity located next to it. Periodontitis is difficult to confuse with other dental diseases, because it has a clear symptom – severe and constantly increasing pain, which cannot be relieved by taking tablets from the pharmacy.
Treatment of periodontitis must be carried out urgently, because you risk not only losing a tooth, but also acquiring complications that are dangerous to the overall health of the body! How periodontitis occurs, what signs will help to identify the disease in a timely manner, how periodontitis is treated in dentistry, at what prices the service is offered in Moscow - we will talk about this in detail in this article.
Symptoms of periodontitis
Despite the fact that experts distinguish several types and stages of periodontitis, there are a number of symptoms, the presence of which most likely indicates the development of this disease.
Clinical manifestations of periodontitis:
- pain due to periodontitis;
- weakness;
- enlarged lymph nodes;
- the temperature may increase by 1 - 2 degrees;
- tooth mobility;
- affected teeth often change color.
Almost all complaints with periodontitis are associated with the occurrence of pain, but patients often go to the doctor only with very severe pain, when the disease is in an advanced stage.
Exacerbation of periodontitis: how does it manifest?
The chronic form of the disease may not have any symptoms for a long time, but sometimes exacerbation phases may occur.
At such moments, the disease begins to resemble the acute stage of development: the gums swell, severe pain occurs, and pus appears. When there is no more pus left in the lesion, the pain goes away and the symptoms disappear, but this does not mean that periodontitis has been cured: it has simply entered the chronic stage again. After some time, an exacerbation will occur again, accompanied by the same symptoms.
Factors such as hypothermia, various diseases, or simply a weakened immune system can provoke an exacerbation of the disease.
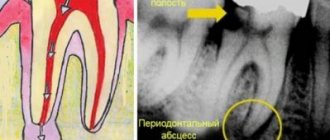
Diagnostics
Almost all methods for diagnosing periodontitis are associated with x-ray examination, since it is quite difficult to visually determine the disease. The most obvious signs:
- change in tooth color;
- the presence of carious cavities;
- fistula due to periodontitis;
- pus during periodontitis (purulent discharge from the gums in the place where the root tip is located).
Be that as it may, the stage of periodontitis can only be accurately diagnosed using x-rays: this is crucial, since the treatment plan is drawn up depending on the type of disease.
Causes
Complications of oral diseases
As a consequence of untreated gingivitis, periodontal disease, tooth root cysts and pulpitis.
Infection
Bacteria penetrate the gums through the bloodstream during inflammatory diseases of the nasopharynx and upper respiratory tract (sore throat, sinusitis, etc.).
Deep caries
As a rule, it leads to the occurrence of granulosa or fibrous forms of periodontitis due to decay products that accumulate daily in the dental canals of severely damaged teeth.
Dentist mistakes
Poorly performed treatment of tooth canals, when fragments of dental instruments, etc. accidentally remain there.
Injuries
The bad habit of constantly pressing on the tooth with a ballpoint pen, a smoking pipe, or a filling that is too high and injures the periodontium can also provoke non-infectious periodontitis.
Professional factor
In professions such as a brass musician or a tailor, pathological pressure on the tooth occurs on a regular basis: in the first case when playing an instrument, and in the second due to the habit of biting off the thread with teeth instead of cutting with scissors.
Attention!!
Patients with reduced immunity and chronic diseases of the endocrine system are also at risk.
Prevention
To reduce the risk of developing the disease, you should follow simple recommendations:
- Brush your teeth at least 2 times a day. It is advisable not to use hard brushes to avoid injury to the gums.
- After eating, rinse your mouth with warm, clean water or a special mouthwash.
- Use toothpicks less often.
- Visit your dentist regularly.
- Remove tartar twice a year and undergo professional cleaning.
- Get rid of bad habits. Alcohol and smoking greatly impair dental health.
Periodontitis is one of the most common dental diseases. If you take good care of your teeth and maintain oral hygiene, you can significantly reduce the likelihood of its occurrence.
Back
Classification of periodontitis
It is believed that the main cause of periodontitis is complications from caries (pulpitis), when the inflammatory process moves to the apex of the root and tooth root periodontitis occurs. This is indeed one of the most common reasons, but this does not always happen.
Classification of periodontitis by reason of occurrence
| Type of periodontitis | Price for installation of one implant |
| Infectious | The most common type of disease when a chain of caries occurs is pulpitis - periodontitis. Appears both after primary and secondary caries. It can be difficult to detect visually (especially periodontitis under a crown or filling). |
| Medication | Periodontitis after dental treatment. Occurs when potent or toxic drugs (arsenic, formaldehyde, phosphate cement, etc.) enter the periodontium. It can often be a consequence of an allergy to certain medications. |
| Traumatic | Its cause is mechanical damage, including due to an incorrectly installed seal. May become infectious. |
Acute periodontitis
Rapid development of the disease (literally in 48 - 72 hours). The tooth may change color and become mobile; swelling of the gums and unbearable pain are often observed. It is quite difficult to detect acute periodontitis on an x-ray, since the bone in the affected area has not yet begun to deteriorate. An enlarged periodontal gap can be seen on x-rays.
Stages of periodontitis (acute)
- Stage 1. Pain, increased sensitivity.
- Stage 2. Exacerbation of periodontitis. Severe inflammatory process, the occurrence of mobility, possible appearance of fistulas and purulent discharge.
Chronic form of the disease
Chronic forms of periodontitis occur much more slowly and are partly asymptomatic. It often occurs with caries, under a filling or crown, so visually detecting the disease can be quite difficult. Sometimes a fistula is observed on the surface of the mucosa in chronic periodontitis. However, the disease can be easily diagnosed using x-rays. In addition, chronic periodontitis in the acute stage causes pain, as well as a feeling as if the tooth is being torn from the inside.
Functions of periodontium –
- Retaining function - it consists in holding the tooth in the alveolus, and the dento-alveolar fibers of the periodontium are primarily responsible for this.
- Shock absorption and distribution function - intercellular substance and periodontal fibers allow you to evenly distribute the chewing load from the tooth to the alveolar tissue.
- Protective function - the connective tissue and cellular components of the periodontium represent the so-called “histohematic barrier”, which ensures the structural and antigenic homeostasis of both the periodontium itself and the surrounding tissues. The implementation of the protective function is mediated by both specific and nonspecific protective factors.
- Plastic function - ensures the preservation of the structure of the periodontium, as well as the reparation of both the periodontium itself and adjacent tissues (for example, the bone plate of the alveolus, as well as the cement of the tooth root). The periodontium is very rich in cellular elements, including osteoblasts, which are responsible for the formation of bone tissue on the surface of the alveoli, as well as cementoblasts, on which the production of replacement cement for the tooth root will depend.
- Trophic and sensory functions are provided by a well-developed vascular and nervous network (a large number of receptors). These functions are closely related to those listed above.
Types of chronic periodontitis
| Type of periodontitis | Description |
| Chronic fibrous periodontitis | Characterized by the proliferation of fibrous tissue. Such periodontitis can be detected on x-rays due to the widened periodontal gap. This form is easier to treat than others. |
| Chronic granulating periodontitis | Rapidly destroys the bone under the apical part of the root. This type of periodontitis in the acute stage is characterized by swelling of the mucous membrane, purulent discharge (periodontitis with fistula). The tooth is often mobile. On a radiograph, granulating periodontitis often resembles a candle flame. |
| Chronic granulomatous periodontitis | On an x-ray, the area under the root tip looks like a large, round spot. This is nothing more than a granuloma. Periodontitis of this type is characterized by the appearance of purulent formations - granulomas or cysts, and in especially severe cases the diameter of the cyst can exceed 3 centimeters. |
Treatment methods
Treatment algorithms for periodontitis vary depending on what form of the disease is acute or chronic.
Stages of treatment of acute periodontitis
- Expansion of the root canal.
- Removal of affected tissue.
- Antiseptic treatment.
- Application of a periodontal bandage.
- Antibiotic therapy.
- Inspection of the canals after 3 days and installation of a temporary filling.
- Control X-ray after 2 months and installation of a permanent filling.
Treatment of chronic periodontitis
- Emphasis on canal drainage.
- Endodontic treatment of root canals.
- Impregnation methods (treatment of canals with a solution of silver salts).
- Tooth extraction if therapy is ineffective.
Disease prevention – at the very end
- Maintaining a hygienic regime: brushing your teeth twice during the day, using mouthwash and floss.
- Balanced diet: minimum carbohydrates and maximum fresh vegetables and fruits.
- Regular self-massage of the gums using your finger.
- Scheduled consultation with a dentist once every 6 months.
Insidious periodontitis: crept up unnoticed, left without a tooth
Periodontitis is the next stage of inflammation after pulpitis. The infection is localized at the apex of the tooth root and surrounding tissues. The disease is often asymptomatic, but without timely help it leads to tooth loss.
Causes:
- Untreated pulpitis. If a tooth hurts and then stops, it means that the inflammation has entered a chronic stage. Chronic pulpitis will slowly spread throughout the tooth and turn into periodontitis.
- Pulpitis treated using outdated methods. Before the advent of the apex locator, there was nothing to measure the length of the root canal, and the doctor acted blindly. If the canal is not completely treated and particles of infected pulp remain in it, complications arise. To avoid this, the doctor may have overdone it and brought the dental material beyond the root apex. Over the years, a focus of infection sometimes develops around a lump of paste.
- Tooth injury. A common problem in active children. Due to injury (the incisors are often affected), the pulp dies, and periodontitis develops after this. In fact, the reason is the same pulpitis that was not noticed and not treated in time.
Types of periodontitis
| Form | View | How it hurts |
| Spicy | Serous | Mild aching pain in the tooth area. |
| Purulent | Throbbing pain. Tooth mobility may increase. Possible swelling of the cheek, weakness, fever, flux. | |
| Chronic | Fibrous | No symptoms or slight darkening, dull color of the crown of the tooth. |
| Granulating | Mild pain when biting eventually turns into pain from heat, chewing, or pressure. The gums become red and swollen. | |
| Granulomatous | No symptoms. A fistula appears to drain the discharge, but the patient cannot always see it. |
The most aggressive is granulating periodontitis, which very quickly spreads to neighboring tissues. With this diagnosis, most often the tooth cannot be saved.
In the granulomatous type of the disease, the inflammation site has a hard shell, and inside it is filled with pus. Depending on the size, these neoplasms are called granuloma (up to 5 mm), cystogranuloma or radicular cyst (more than 1 cm).
Thus, granuloma and tooth root cyst are manifestations of chronic periodontitis.
Diagnostics
Do not confuse fistula with stomatitis. The fistula looks like a pimple, is located on the gum near the roots of the tooth, and does not hurt when pressed. If a fistula appears, contact your dentist as soon as possible.
The doctor can suspect a problem before the formation of a fistula or gumboil based on complaints. It is very important that the patient describes all the symptoms and does not hesitate to complain about mild, unexpressed, occasional pain and discomfort.
X-rays help to accurately establish the diagnosis. Periodontitis is visible even on a small targeted photograph. Next, to plan treatment, the dentist will suggest taking a panoramic image (all teeth in one frame) or a computer tomogram (a three-dimensional image of the dental system).
CT - 3D computer tomogram
allows you to see the type of periodontitis, the location and size of cystogranuloma, and give a prognosis for treatment.
Positive dynamics
visible on a repeat tomogram 2 years later
From all sides
The advantage of CT is the ability to examine the tooth and the tissue around it from different angles
Treatment
Depending on the stage and form of the disease, the doctor will select the optimal method.
1. Therapeutic treatment. Typically, three visits to the dental office are required.
- Urgent Care. The dentist will remove the source of inflammation: clean and disinfect the canals using medications and laser sterilization. If necessary, the doctor will install a drainage to drain the pus.
- Treatment of tooth canals and installation of a temporary filling. If there are doubts that the immune system will cope with the remaining microorganisms, the dentist may prescribe antibiotics, physiotherapy, rinses and medicinal baths.
- Tooth restoration. At the last visit, the dentist will take an x-ray to make sure that the inflammation has been removed. After this, you can begin filling and restoring the aesthetics and chewing function of the tooth.
- Observation. We can talk about the positive dynamics of the tissues surrounding the tooth after 1-2 years based on the results of an x-ray examination.
2. Tooth-preserving operations. Sometimes conservative methods are not enough. A dental surgeon can perform a cystectomy (removal of the cyst) or apex resection (cutting off part of the tooth along with the cyst).
3. Tooth extraction. In advanced stages, it will not be possible to completely defeat foci of infection. Attempts to save a tooth will lead to large financial expenses and jeopardize neighboring teeth. The best solution would be to install an implant in place of the affected tooth.
If a tooth is left without treatment, it will be removed prematurely. The inflammation will grow and go into an acute stage, and at the most unfortunate moment.
Doctors call chronic periodontitis a ticking time bomb. Exacerbation is provoked by stress, exertion, hypothermia or climate change. That is, it will happen on a long-awaited trip to the sea, while working on an important project, before an exam, or during an infectious disease.
Periodontitis in children
In a child, periodontal inflammation can develop on both milk and permanent teeth. Features of childhood periodontitis:
- high flow rate,
- severe symptoms (temperature, pain, swelling, possible suppuration),
- increased risk of complications. If urgent measures are not taken, the rudiments of permanent teeth will suffer.
Treatment follows the same scheme as for adults. If there is less than a year left before a baby tooth falls out or the roots have already resolved, the pediatric dentist will suggest removing the tooth.
Prevention
Simple and inexpensive measures will reduce the risks of periodontitis and tooth loss.
- Maintain good oral hygiene.
- Eat right. Excess carbohydrate foods provoke the development of pathogenic microorganisms.
- Contact a specialist for dental treatment in a timely manner. Come for a routine examination every six months, even if nothing hurts. Voice all complaints.
- Treat with understanding the doctor’s suggestion to undergo a panoramic radiography or computed tomography. Complete information will allow you to notice and cure the disease.
For expert assistance in writing the article and providing examples of work, we thank dentist-therapist Olga Yuryevna Yuryeva.
Prognosis for periodontitis treatment
In dentistry, periodontitis is considered a very difficult disease to treat, especially its advanced chronic forms. If in mild forms it is enough to depulpate the tooth and remove the affected tissue, then to treat severe forms it is necessary to carry out a number of more complex manipulations. In the acute form, the doctor, as a rule, opens the body of the tooth, cleans the canals and leaves them open for the release of accumulated pus. The patient is then prescribed antibiotics for periodontitis, as well as mouth rinses.
Rehabilitation for the granulating and granulomatous type takes a longer time (up to 2 - 3 months). This is due to the fact that inflammation and bone lesions are neutralized with the help of special medications based on calcium hydroxide, the effectiveness of which appears only after long-term use.
Unfortunately, conservative treatment of periodontitis is impossible if there are cysts and granulomas. Here only invasive interventions will save you, in particular, removal of the apical part of the tooth root along with the formations. Remember that complications of periodontitis take much longer to treat (and are more expensive): do not let your problems get worse and consult a doctor on time.
What to do if you have periodontitis
If the diagnosis is confirmed, the disease must be treated. How dental periodontitis is treated depends on the form and stage of inflammation. The correction program may include therapeutic and surgical techniques.
Conservative therapy
Conservative methods are aimed at maximizing the preservation of the structure of the unit and restoring its functionality. The program includes elimination of the source of inflammation and endodontic treatment. All manipulations are performed under local anesthesia. Treatment regimen:
- Conducting anesthesia.
- Opening the crown, providing access to the root canals.
- Expansion of the cavity.
- Pulpectomy (if the segment has not been previously treated) or unfilling of the canals.
- Antiseptic, medicinal treatment of cavities.
- Temporary filling (for the period of anti-inflammatory treatment).
- Removal of temporary filling, filling of root canal.
- Restoration of the coronal part of the unit.
- Prescribing a course of antibiotic therapy.
Surgical intervention
Invasive methods are used when other methods are ineffective. The operation can be carried out using different protocols:
- Resection of the apex of the tooth root followed by filling the cavity with special bone-forming materials.
- Extraction of the diseased segment.
If periodontitis is not treated, complications are possible: odontogenic periostitis (inflammation of the periosteum), abscess, phlegmon, etc. The infectious process spreads to nearby lymph nodes, and lymphadenitis occurs. In severe cases, possible: tooth loss, osteomyelitis, sepsis.