Published: 04/16/2012 Updated: 05/20/2021
In the 70s of the last century, a group of infections was identified, the peculiarity of which is that, while relatively harmless for adults and children, they become extremely dangerous for pregnant women. This group of infections is usually called TORCH infections, after the first letters of the Latin names of the infections included in it. This abbreviation stands for: TO - toxoplasmosis; R - rubella (Rubella); C - cytomegalovirus infection (Cytomegalovirus); H - herpes infection (Herpes simplex virus).
The peculiarity of TORCH infections is that when a woman is infected with them during pregnancy, they can have a detrimental effect on all systems and organs of the fetus, especially on its central nervous system, increasing the risk of miscarriage, stillbirth and congenital deformities of the child. Perinatal infections account for approximately 2-3% of all congenital anomalies of the fetus. Most infections are dangerous if they are initially infected during pregnancy. Recurrences of herpes can be dangerous during childbirth and the postpartum period. Often, infection of a pregnant woman with TORCH complex infections is a direct indication for termination of pregnancy.
Let us dwell in more detail on each infection included in the complex.
What are ToRCH infections?
The abbreviation ToRCH comes from the first letters of the most dangerous infections for the fetus - Toxoplasma (toxoplasma infection) - Rubella (rubella) - Cytomegalovirus (cytomegalovirus) - Herpes (herpes). These are classic infections. In addition to them, they also talk about infections such as parvovirus (infection caused by parvovirus B19), listeriosis, hepatitis B and C and some others. All of them can affect people of any gender and age, but the term itself is used in relation to women who are preparing for pregnancy, pregnant women, as well as the fetus and newborn. Rubella, toxoplasmosis, cytomegalovirus and herpes infections are common infections. In most cases, the first encounter with them occurs in childhood and adolescence - this is called primary infection, after which immune protection remains. If the body encounters an infection again, it is called a secondary infection or reinfection.
References
- Order of the Ministry of Health of the Russian Federation dated November 1, 2012 No. 572n “On approval of the Procedure for providing medical care in the field of obstetrics and gynecology (except for the use of assisted reproductive technologies).”
- Infectious diseases: national guidance // Ed. N.D. Yushchuka, Yu.Ya. Vengerova. – M.: GEOTAR-Media, 2010. – 1056 p.
- Sadova N.V. et al. TORCH syndrome: clinical diagnosis and etiological verification // Russian Medical Journal 2014, No. 3 p. 194.
- Nahmias Andre J. The TORCH complex-perinatal infections associated with toxoplasma and rubella, cytomegalo- and herpes simplex viruses. Pediatric Research 5(8):405-406 August 1971.
Why is the examination carried out?
It is before pregnancy (or in the early stages) that we need to find out whether there was an infection or not. If there was, you don’t have to worry, this infection is not dangerous for a pregnant woman. If not, then the doctor will tell you about a set of preventive measures (for example, if we are talking about rubella, then you can get vaccinated, if we are talking about toxoplasma, you can follow certain rules to reduce the risk of infection, etc.). In addition, for those infections for which there are no protective antibodies, it is important to conduct regular monitoring so as not to miss an infection during pregnancy.
Facts about IUI
In less than 10 out of 100 pregnancies, the infection is transmitted to the unborn baby from his mother. And approximately 0.5% of newborns are born with corresponding symptoms. But, if one or another infection is present in the mother’s body, this is not a complete guarantee that the child will also have it.
Some infectious diseases that threaten the development of the embryo are asymptomatic for the mother, without causing much harm to her body. Basically, the fetus becomes infected with the same infection as the mother if she became infected with the disease for the first time.
If a pregnant woman’s disease is detected and treated in time, the risk to the unborn baby is minimal.
The essence of the analysis
Blood is taken from a vein of the pregnant woman, which contains antibodies to infections (immunoglobulins Ig). There are five classes of antibodies, but in this case only two should be determined - IgM and IgG. Many laboratories do only a comprehensive examination. But it is quite possible to find out whether the immunoglobulins you are interested in are available, which will cost less. The analysis can reveal not only the presence of antibodies, but also their quantity. The latter option is more preferable, as it gives the doctor maximum information. If necessary, it is possible to find out the time of infection by determining at what point immunoglobulin began to be produced.
Additional and confirmatory studies: immunoblot
Conventional ELISA tests for antibodies to infections are screening tests, that is, they allow one to suspect the presence of an acute infection or recent infection that requires certain actions. If an acute infection is suspected during pregnancy, more specific (confirmatory) tests are required before starting treatment.
Immunoblot is a highly specific and highly sensitive method:
- Sensitivity 97%
- Specificity 99%
- High resolution between negative and positive results!
- More accurate detection of infection time
The essence of the immunoblotting method (blotting - from English, blot, spot) is as follows. During the immune response, the body produces antibodies to different proteins of the infectious agent at different times. For example, when encountering Toxoplasma, IgG antibodies to ROP1 first appear, then to the MAG1 protein, and later to the SAG1 protein. If we detect antibodies to each of these proteins in the serum, we can know when the production of antibodies began, with an accuracy of 2-3 weeks if the infection was recent.
Immunoblot studies are more expensive and time-consuming than antibody screening tests. Therefore, the examination is usually carried out in two stages: first, a risk group is identified (serological testing for the presence of IgG and IgM antibodies). Next, if a previous infection is suspected, an immunoblot study is performed.
Important: Immediately after receiving the screening results of the antibody test, you should consult your doctor.
In the CIR laboratory: immunoblot study: cytomegalovirus (IgG, IgM), toxoplasma (IgG, IgM) and rubella (IgG)
Decoding the results
It is important to understand that primary infection with TORCH infections is dangerous during pregnancy. The possibility of getting sick is excluded if the woman has encountered the pathogen before. The results obtained are read as follows: the presence of class G antibodies indicates that the woman has long been ill with an infection, the body has formed immunity that will protect the child and mother from a dangerous disease; class M antibodies indicate an acute infection (primary infection or relapse); the absence of IgM and IgG means that there is a possibility of infection with rubella, toxoplasmosis, herpes and cytomegalovirus. To understand how long ago the infection occurred, it is necessary to analyze the amount of IgG. If these antibodies are not present, it means that the body has encountered the disease recently.
Complementary and confirmatory studies: IgG antibody avidity
When you need to figure out how long IgG antibodies have been present in the body (that is, how long ago the infection occurred), a special test is performed for the avidity of IgG antibodies (from the Latin Avidity - greedy). During the development of the immune response, IgG antibodies gradually increase their binding strength to the infectious agent. This binding strength is called avidity. At the very beginning, IgG binds the pathogen, but the connection is quite weak. Such IgGs are called low-avidity. After a few weeks, the antibody is able to bind its target much more strongly. Such antibodies are called high-avidity.
Thus, the appearance of low-avidity antibodies indicates that a dangerous encounter with a virus or Toxoplasma took place recently. If low-avidity antibodies are detected during pregnancy, confirmatory research methods are prescribed to make a decision (see immunoblot below). The result of the analysis is presented by the avidity index, expressed as a percentage.
Example result: In this example, high-avidity IgG antibodies were detected.
*reference values may vary in different laboratories.
| Result | 89% |
| Interpretation of results | |
| Result | Meaning |
| <50% | Low-avidity |
| 51-69% | transitional |
| >70% | Highly avid, protective antibodies |
In the CIR laboratory:
avidity of IgG antibodies to cytomegalovirus, toxoplasma and rubella.
General recommendations
If a woman does not have antibodies to rubella, it is advisable to get vaccinated. In this case, pregnancy is possible only three months after vaccination. It is not possible to protect yourself from other infections in this way. If an acute disease is detected, it is necessary to first be cured, and only then conceive a child. A pregnant woman without immunity to TORCH infections needs to be very attentive to her health and avoid visiting places of possible infection. Limiting contact with cats, being careful when working with raw meat, and planting flowers and beds in the ground will protect you from toxoplasmosis. Be sure to wash your hands thoroughly after such contact. The presence of high titers of class M immunoglobulin requires immediate consultation with a doctor to prescribe more in-depth studies and treatment to avoid problems with fetal development.
Dictionary
Antibodies (immunoglobulins) are protective proteins of the immune system that are formed in the body when foreign substances (antigens) enter. Antigens are substances that, when introduced into the human body, trigger the production of antibodies and an immune response. Perinatal (peri – around, natalis – birth) (perinatal) is a period that begins a few weeks before birth and ends a few weeks after the birth of the child. Prenatal - antenatal Vaccination (vaccination) is a method of preventing infectious diseases. The method involves introducing a substance into the body that can stimulate the formation of specific antibodies (the development of immunity to a given disease). Avidity is a characteristic of the strength of binding of antigen and antibodies. ELISA (enzyme-linked immunosorbent assay) - enzyme-linked immunosorbent assay - a laboratory method based on an antigen-antibody interaction reaction.
Anti-Rubella-IgM (IgM antibodies to the rubella virus)
Antibodies of the IgM class to the rubella virus.
Determination of IgM antibodies to the rubella virus is used to diagnose primary infection with the rubella virus (Rubella). They can be detected within 1 to 3 days after the onset of clinical symptoms, and in most cases their concentration decreases rapidly within 6 to 8 weeks from the onset of the disease. The presence of IgM antibodies to rubella virus indicates recent infection. Laboratory diagnosis of this infection in pregnant women is undertaken to assess the risk of infection to the fetus. Determination of IgM is also important for the diagnosis of congenital rubella in newborns.
Anti-Toxo-IgG (IgG class antibodies to Toxoplasma gondii)
Class G antibodies to Toxoplasma gondii (T. gondii).
Antibodies class G
are produced for the toxoplasma antigen in acute, subacute, chronic and latent forms of toxoplasmosis after 3 - 4 weeks from the moment of infection. Class G antibodies usually persist for life. They perform a protective function and prevent re-infection in the vast majority of cases.
Features of infection.
The causative agent, Toxoplasma gondii, is a protozoan. The life cycle of the pathogen takes place inside the cells of the host organism. The definitive host of the parasite, infected cats and other representatives of the feline family, excrete a special form of toxoplasma - oocysts - in their feces. Oocysts are stable in the external environment. Oocysts that enter the body of an intermediate host (rodents, birds, livestock, humans) continue their life cycle in the muscle and other tissues of the body, where pseudo- and true cysts are formed.
Risk groups for intrauterine infection
Women who:
- live in a family with children who go to kindergarten, school, or other institutions
- work in the medical field, having contact with carriers of diseases or sick people
- work in preschool and school children's institutions
- have 2 or more medical abortions
- patients with inflammatory pathologies that occur in a chronic form
- have untimely rupture of amniotic fluid
- have a history of embryonic malformations and antenatal fetal death
- have once given birth to an infected child (one or more)
Anti-Rubella-IgG (IgG antibodies to the rubella virus)
An indicator of the presence of immunity to the rubella virus.
IgG antibodies to the rubella virus begin to be produced 3-4 weeks after infection and are detected after the end of the acute illness for life, providing protection against re-infection. Detection of anti-Rubella-IgG in a concentration of less than 10 U/ml indicates their insufficient level to protect against clinical manifestations of the disease with or without exposure to the rubella virus.
An anti-Rubella-IgG level of more than 10 U/ml is recommended as an indicator of the presence of immunity to this virus. Determination of anti-Rubella-IgG titers over time (in paired studies with an interval of 2-3 weeks) is used, if necessary, to confirm a recent infection with the rubella virus (in addition to the determination of anti-Rubella-IgM). A significant increase in IgG titers indicates the severity of the process. Positive anti-Rubella IgG results when testing umbilical cord blood or newborn blood should be interpreted with caution, since specific IgG can be transmitted to the fetus from the mother through the placenta.
Pathogens of IUI
Most bacteria and viruses can be passed on to the unborn baby, causing serious consequences. Those viruses that provoke acute respiratory viral diseases do not reach the fetus. They can be dangerous for the baby only if the pregnant woman has a high temperature.
A mother can become infected with rubella through airborne droplets. It is not necessary to be close to a sick person; infection is also possible at a distance. In this case, the consequence for the fetus will be fetal rubella syndrome.
Cytomegalovirus is transmitted through body fluids. This is mostly saliva, but may include semen and urine, as well as blood. In a child, the infection may manifest itself with corresponding symptoms after birth, or it may occur in a latent form.
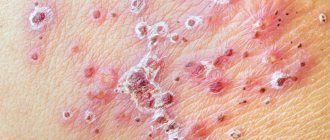
Herpes simplex virus 2 is transmitted mainly through unprotected sexual intercourse. If this happens to a pregnant woman, her child will be born with a congenital form of herpes. Parvovirus B19, like rubella, is transmitted by airborne droplets to a pregnant woman. As a result, the fetus develops dropsy and anemia.
Chickenpox is transmitted not only through the air, but also through household contact. A child receives developmental defects due to intrauterine infection (if the infection occurred in the first trimester). If the infection occurs before childbirth, then there will be a congenital form of this disease, and this is a very dangerous condition.
Listeriosis (a bacterial infection) can develop in a pregnant woman if she eats contaminated cheeses, meats or vegetables. The child eventually develops pneumonia and/or sepsis. Syphilis is transmitted to pregnant women through sexual contact if the partner has been infected. After birth, a child develops this disease with all the ensuing consequences. Tuberculosis, which is also a bacterial infection, is transmitted through the air. The embryo can die in the womb, be born prematurely, with a congenital form of tuberculosis.