Congenital form
In most cases, intrauterine infection of a child does not lead to the development of symptoms. If a pregnant woman encounters cytomegalovirus invasion for the first time, the risk of developing a congenital disease in the newborn increases.
Signs and complications of congenital infection:
- Liver damage, manifested by organ enlargement, jaundice and increased bleeding.
- Intrauterine growth retardation and prematurity.
- Microcephaly and retinitis.
- Enlarged spleen.
The probability of death from congenital infection reaches 30%. The negative consequences of cytomegalovirus infection subsequently become the cause of human intellectual disability.
What to do if CMV is detected in a pregnant woman?
If a pregnant woman does not have IgG antibodies, she should undergo frequent monitoring and follow doctors’ recommendations for prevention. As a rule, contraceptive methods are discussed with a specialist, limiting too close physical contact with older children, especially if they go to a preschool institution, separate linen and towels, and no need to eat from the same plate for children. Pregnant women who have not previously had CMV infection, working in preschool institutions, orphanages, etc., can temporarily change the conditions of their work.
Traces of the virus found in various biological fluids of the expectant mother indicate a different level of danger to the child. There is a correlation between the amount of viral DNA in the mother’s amniotic fluid and the likelihood of the unborn child developing manifest CMV infection. Pregnant women with symptoms of ARVI pharyngitis and elevated temperature should undergo DNA diagnostics of cytomegalovirus in order not to miss its activation or reactivation, in which case treatment may be prescribed. If the expectant mother has been diagnosed with a virus in one form or another, the child must be examined, since this infection significantly affects development, quality of life, and possible diseases that arise as a result of this infection. The goal of this careful approach to identifying the virus is timely treatment and prevention.
Goals of therapy and prevention
- prevention or termination of the phase of active reproduction of the virus;
- preventing the transmission of the virus from cell to cell;
- inactivation of free viruses in the extracellular space;
- transferring an actively reproducing virus into a state of latent persistence
At this stage of scientific development, there is no means by which cytomegalovirus can be completely eliminated, so chronic CMV infection is present in the body of those who have encountered it.
Features of the virus
Human cytomegalovirus is a DNA virus from the herpesvirus family.
Other members of this family are the causative agents of herpes, chickenpox, mononucleosis and other diseases. CMV develops in connective tissue cells and often spreads throughout the body. Replication of viral particles occurs in leukocytes: the pathogen enters the cell, introduces its own genetic information into the nucleus and triggers the assembly of the necessary protein components. After replication, virions leave the affected cell and attack other leukocytes, affecting external receptors. The mechanism of transmission of the virus has not been thoroughly studied, but experts know that CMV can be present in almost all biological fluids, including saliva, semen, urine and blood. It is believed that the infection is most often transmitted through kissing and sexual contact. Due to its moderate contagiousness, infection requires close contact with a carrier of the virus.
In the external environment, the virus quickly loses its virulent properties, so the household route of transmission is not so common. CMV is easily inactivated by ethanol and exposure to high temperature. After entering the body, the virus is not destroyed by the immune system, however, lymphocytes are able to secrete immunoglobulins that remain in a person throughout life.
The danger of cytomegalovirus during pregnancy
Infection with the virus in the first trimester of pregnancy is very dangerous. Cytomegalovirus can penetrate the placenta into the fetus. Infection can cause intrauterine death.
If infection occurs later, the following situation is possible: the pregnancy will continue, but the infection will affect the internal organs of the child. A baby may be born with congenital deformities, various diseases (edema of the brain, microcephaly, jaundice, inguinal hernia, heart disease, hepatitis).
Dire consequences can be avoided if the virus is detected in time, so it is very important to plan your pregnancy and get tested for any infections before conception, as well as visit your doctor regularly throughout your pregnancy. With proper treatment, the baby can be born healthy, being only a passive carrier of cytomegalovirus.
Analysis for cytomegalovirus during pregnancy
It is almost impossible to independently find out about the presence of cytomegalovirus in your body. Being in a latent form, the virus does not manifest itself in any way. When active, the infection can be confused with another disease. To detect the virus, it is necessary to be tested for cytomegalovirus during pregnancy, or more precisely for TORCH infection. It is used to detect the presence or absence of not only cytomegalovirus, but also toxoplasmosis, rubella, and herpes simplex virus (types 1–2).
Cytomegalovirus is diagnosed using the following methods:
• polymerase chain reaction; • cytological examination of urine and saliva sediments; • serological studies of blood serum.
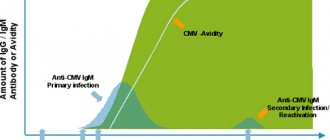
The polymerase chain reaction is based on the determination of deoxyribonucleic acid, which is the carrier of the hereditary information of the virus and is contained within it. Scrapings, blood, urine, sputum and saliva are used for research. Cytomegalovirus in a smear during pregnancy is diagnosed by the presence of giant cells. The purpose of serological studies of blood serum is to detect antibodies that are specific for cytomegalovirus. The most accurate method is enzyme-linked immunosorbent assay (ELISA), which provides the determination of different types of immunoglobulins (IgM, IgG).
The results of the analysis for cytomegalovirus may indicate several options:
1. IgM is not detected, IgG is within the normal range; 2. IgM is not detected, IgG is higher than normal (positive IgG cytomegalovirus during pregnancy); 3. IgM is higher than normal.
In the first case, the female body did not come into contact with cytomegalovirus, which means that preventive measures should be taken and situations in which one can become infected should be avoided.
The second analysis indicates that the female body has encountered the virus, but at the moment it is in an inactive form. There is no need to worry about primary infection during pregnancy, but there is a risk of reactivation of the virus.
The third analysis indicates that a primary infection has occurred or a reactivation of cytomegalovirus, which was in a latent form in the body, is developing.
It is worth noting that IgM is not always detected. Doctors focus on the IgG level. Normal IgG levels may vary from woman to woman. It is advisable to get tested before conception. This allows you to determine the norm of cytomegalovirus during pregnancy. Reactivation of the virus is indicated by the IgG number increasing fourfold or more.