general characteristics
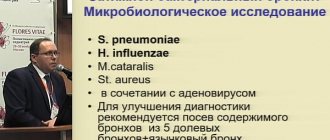
The study is indicated for suspected bacterial origin of pharyngitis and tonsillitis in order to select adequate etiological therapy. Cultivation of material from the throat is used primarily to identify hemolytic group A streptococci, S.aureus, Str.pneumoniae. The distinction between infection and patient colonization cannot be determined by culture alone. It is necessary to take into account the degree of growth and the clinical picture. Isolated microorganisms: Streptococcus pneumoniae, Streptococcus pyogenes, Streptococcus spp., Coagulase-negative staphylococci, Staphylococcus aureus, Enterobacteriaceae, Pseudomonas aeruginosa, Haemophilus influenzae, Moraxella catarrhalis, Candida spp., Corynebacterium spp., Neisseria spp.
4. Results of throat culture for microflora
Culture results will be ready within 1-2 days, in some cases testing is carried out within a week.
There is also a rapid test for streptococci.
The results of such a test for streptococcus will be ready in 10-15 minutes. This test is only for bacterial infections caused by streptococcal bacteria.
A rapid test for streptococcus can show two results:
- Negative test results for streptococcus.
Streptococcal bacteria were not detected. Microflora culture may be recommended. - Positive test results for streptococcus.
Streptococcal bacteria were detected. This means you have strep throat (strep throat). You must start taking antibiotics immediately.
Throat culture for microflora can also be negative or positive:
- Negative culture results for microflora. There are no bacterial or fungal infections and their growth is not observed. Negative results may mean that your infection is caused by a virus rather than bacteria or fungus. Throat infections can be caused by different viruses - enteroviruses, Epstein-Barr virus, herpes simplex virus, respiratory syncytial virus (RSV).
- Positive results of throat culture for microflora. Bacterial growth is observed. Examples of bacterial throat infections are strep throat, diphtheria (diphtheria corynebacterium), and whooping cough (whooping cough). Fungal growth is observed. The most common fungal infection in the throat is oral candidiasis, which is caused by yeast-like fungi of the genus Candida.
Patient preparation rules
tonsil smear
Standard preparation conditions (unless otherwise determined by the doctor):
2 weeks in advance Stop taking antibacterial and antimycotic drugs. 24 hours in advance Stop taking any local medications and procedures in the area of biomaterial collection. 2 hours before Do not use on an empty stomach or 2 hours after meals.
You can add this study to your cart on this page
Diagnostic value of mouth swab
At its core, it is completely, 100% analogous to a urogenital smear.
The only difference is where the diagnostic material is taken from.
A mouth smear helps determine the spectrum of oral microflora in the person being examined, regardless of gender.
This method refers to laboratory-instrumental techniques and performs one task: obtaining diagnostic material for a detailed study of microflora.
Samples obtained using a mouth swab are examined in different ways:
- microscopy of native material and fixed, stained smear
- bacteriological examination (culture)
- immunological studies
- molecular genetic
The main thing is to correctly and accurately collect diagnostic samples.
But before you collect them, you need to determine who needs it.
Interpretation:
- Of key importance is the quantitative assessment of grown colonies of microorganisms. I degree of growth (very meager growth) - no growth on solid nutrient media, only in liquid nutrient medium (105 CFU/tampon/ml). I and II degrees of growth indicate contamination or carriage , aIII and IV - in favor of the etiological significance of this microorganism. Isolation of Streptococcus pyogenes, Streptococcus pneumonieae, Haemophilus spp., Staphylococcus aureus in the absence of a clinical picture of the disease does not indicate the presence of the disease; In some patients, these microorganisms can colonize the normal upper respiratory tract.
Sample result (PDF)
What is it and why?
The oral cavity of every person is very densely populated with microorganisms.
Most of them are harmless saprophytes, among which there are cocci and bacilli.
There are even non-pathogenic spirochetes.
Our body has learned to coexist safely with them, and we simply do not notice them.
But such prosperity does not always happen.
Problems arise when foreign microorganisms enter the oral cavity.
For example, pathogens of sexually transmitted infections that thrive on the mucous membranes of the mouth and genitals.
The list of microbes that are capable of such a change in habitat is quite wide:
- Trichomonas
- treponema pallidum
- human papillomaviruses (HPV)
- herpetic group viruses
- gonococci
- chlamydia
In principle, this list can include almost all STD pathogens.
A smear helps to identify them in the mouth.
Carrying out manipulation
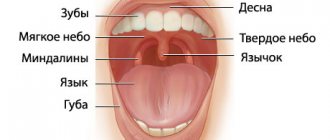
The patient enters the office and sits on the couch. The doctor asks the patient to throw his head back on a special headrest and open his mouth wide.
The specialist presses the patient’s tongue with a wooden or metal oblong spatula, then takes a swab with a cotton tip and collects biomaterial from the mucous membrane of the pharynx. During the manipulation, the person does not feel pain or severe discomfort; only a gag reflex may occur due to the touch of the stick to the back wall of the throat.
The doctor places the resulting sample in a special container or test tube. In laboratory conditions, the material taken will be exposed to different environments in order to determine the presence of microbes, fungi and bacteria.
Depending on the reaction to a certain environment and the behavior of microorganisms during exposure to drugs and antibiotics, the laboratory assistant issues the appropriate research result.
Typical signs of oral STDs
It often happens that people come to dermatovenerologists from dentists or laryngologists.
After the treatment from these doctors turned out to be ineffective.
Or after the patient has had a mouth smear examined for microflora.
And they found sexually transmitted infections in the material.
How they get there is sometimes quite difficult to figure out.
The most common method is oral sex.
It is also necessary to remember that more than 200 thousand germs are transmitted with a deep kiss.
And, if your partner had herpetic rashes in the mouth, infection cannot be avoided.
The same applies to atypical forms of primary syphilis, gonorrhea and other STDs.
Gonorrhea is transmitted through oral sex.
It manifests itself as a sore throat, hoarseness and other symptoms of a prolonged cold.
Syphilis is the same.
Characteristic signs are painless lumps and reddish ulcers on the tongue and red border of the lips.
May occur as chronic flaccid tonsillitis.
Trichomonas, chlamydia and mycoplasma when localized in the mouth do not cause specific symptoms.
They can be suspected only by a lingering cough or tonsillitis.
The patient's general well-being does not deteriorate.
Herpes is easy to detect: pain and burning, rashes on the mucous membranes, transforming into erosions.
Relapses up to 5-6 times a year.
Against the background of immunodeficiency, constant persistence of rashes in the mouth is possible.
Human papillomavirus lesions are painless and usually have the appearance of genital warts.
Having reached large sizes, they can make swallowing and speech difficult.
Infection through domestic means cannot be ruled out.
All infections can be transmitted through a toothbrush.
Because of this, children whose parents suffer from the oral form of one or another sexually transmitted infection often suffer.
Another reason for taking a swab from the mouth is the need to assess the prevalence of STDs when examining a patient with established damage to the reproductive organs.
Indications for performing an oral smear
The reasons for conducting such a study differ for doctors of different specialties.
As for venereology, here are the main symptoms for which dermatovenerologists take a swab from the mouth:
- burning and pain in the mouth
- painful rash on the mucous membranes of the mouth and cheeks
- enlarged tonsils without pronounced clinical signs
- complaints of a sore throat for a long time
- the appearance of painless lumps and wounds in the mouth, on and under the tongue
- unpleasant odor with the exception of dental caries
- sour taste, foamy saliva
In principle, everything is decided individually each time.
We have listed only a few signs that indicate the main STDs characteristic of lesions in the oral cavity.
Necessary equipment
Individual protection means
The material collected is infectious and the procedure may generate an aerosol (if sneezing or coughing), so the person performing the swab must wear personal protective equipment: a long-sleeved waterproof gown, gloves, a mask and safety glasses or a face shield (if swabbing the face with suspected SARS-CoV-2 infection, it is best to use an FFP2/FFP3 filter mask [if not available, a surgical mask is acceptable, especially if work is not performed with continuous exposure], a face shield, an additional gown, e.g. non-woven, and double gloves - internal, worn under the cuff, and external ones on the cuff of the robe). The procedure should be carried out in a separate and well-ventilated room. The patient must wear a mask, which he removes immediately before performing the procedure.
Smear collection kit
Before performing the procedure, you should prepare a smear collection kit. The type of microorganism and the planned test determine the type of swab probe and substrate. To collect material for PCR testing, you should use only swab probes with synthetic fiber wound on a plastic rod (others may cause PCR inhibition). Do not use swab probes made from organic materials (eg cotton, wood) or calcium alginate, as they may inhibit PCR. In addition, when taking a smear in the direction of whooping cough, you should not use cotton swabs or rayon (rayon) swabs. Polyester, Dacron or nylon swabs on a plastic shaft are probably universal. On the shaft of the swab probe there is a factory mark on the depth to which it should be inserted, and a narrowing at which it should be broken after lowering it into the test tube.
In case of diagnosis for the presence of SARS-CoV-2, you can use:
1) commercial kits - contain a flexible flocked plastic probe and a tube with virological medium
2) home made kits (for swabs from the throat and nose), containing:
a) sterile flocked or standard plastic swab probes with dacron, viscose or rayon swabs
b) test tubes with a sterile buffered 0.9% NaCl solution in a volume that allows the end of the swab probe to be immersed (Fig. 1).
Picture 1. A - equipment needed to prepare a home made kit: 1 - a needle for drawing up a 0.9% NaCl solution, 2 - a syringe, 3 - a small package with a 0.9% NaCl solution (small packages should be used to avoid contamination of the solution when used) repeated use), 4 - probe-tampon, 5 - test tube. B - 0.9% NaCl solution should be drawn into a syringe under aseptic conditions. B - approximately 1 ml of solution should be poured into a test tube into which, after taking a smear, a swab probe will be placed
Before taking a smear, you should describe the tube in which the swab probe will be placed and stick a code on it (if required; Fig. 2).
Figure -2. Description and sticking of the code on the test tube. The following information must be indicated on the tube: patient’s first and last name, date of birth, date and time of swab collection.