Cardiac arrest is a complete cessation of ventricular contractions or severe loss of pumping function. At the same time, electrical potentials disappear in myocardial cells, impulse pathways are blocked, and all types of metabolism are quickly disrupted. The affected heart is unable to push blood into the vessels. Stopping blood circulation poses a threat to human life.
According to WHO statistical studies, 200 thousand people in the world have cardiac arrest in a week. Of these, about 90% die at home or at work before receiving medical attention. This indicates a lack of public awareness of the importance of emergency response training.
The total number of deaths from sudden cardiac arrest is greater than from cancer, fires, road accidents, and AIDS. The problem concerns not only older people, but also people of working age and children. Some of these cases are preventable. Sudden cardiac arrest does not necessarily occur as a consequence of a serious illness. Such a defeat is possible against the background of complete health, in a dream.
General information
Sudden cardiac arrest is a non-violent, sudden death due to various causes, manifested by sudden loss of consciousness and cessation of circulation.
It is extremely important to distinguish between the concept of “sudden cardiac death” and the concept of “sudden death”. The main diagnostic criterion for the latter is the causative factor: sudden death develops as a result of non-cardiac causes (rupture of an aneurysm of large vessels, drowning , thromboembolism of the pulmonary artery or cerebral vessels, airway obstruction, electric shock, shock of various etiologies, embolism, drug overdose , exogenous poisoning, etc.), while sudden cardiac death (SCD) is caused by heart diseases that develop immediately or within an hour from the moment of acute changes due to cardiac dysfunction. However, information about heart disease may or may not be available.
Cardiac arrest means the cessation of its mechanical activity, leading to the cessation of blood circulation, which, in turn, leads to oxygen starvation of vital organs and, in the absence/ineffectiveness of urgent resuscitation measures, leads to death. Sudden cardiac death is a group concept that includes a wide range of pathologies that cause it (various nosological units from the groups of ischemic heart disease, myocarditis , cardiomyopathies , prolongation of the Q-t interval , malformations of the heart / blood vessels, Brugada syndrome , Wolff-Parkinson-White syndrome , etc.) .
That is, this is a concept that is characterized by a single mechanism of death, namely, ventricular disturbances in heart rhythm, leading to chaotic and scattered (asynchronous) contractions of individual muscle fibers of the heart, as a result of which the heart ceases to perform a pumping function - to supply blood to organs and tissues . The most common type of sudden cardiac death is sudden coronary death (ICD 10 code: I24.8 Other forms of acute coronary heart disease). That is, coronary death is an independent nosological form of IHD; accordingly, cases of sudden death in patients with IHD are formulated as “sudden coronary death”, and in other cases of sudden death of a cardiac nature - as “sudden cardiac death” (I46.1).
Despite a significant decrease in mortality from cardiovascular diseases in developed countries over the past 15-20 years, it continues to remain high and causes the death of about 15 million people annually. SCD accounts for about 15% of cases in the overall mortality structure in the world, and about 40% from diseases of the heart and circulatory system (38 cases/100,000 population).
In Russia, the share of cardiovascular diseases in overall mortality is 57%, which is 200-250 thousand people per year. At the same time, IHD accounts for 50.1%. In almost 15% of cases, the cause of cardiac arrest is cardiomyopathies , 5% of patients had inflammatory heart diseases, and only 2-3% of patients had genetic abnormalities.
About 40% of people die from VVS during working age. The incidence of SCD in people of working age (25-65 years) is 25.4 cases/100 thousand population. This figure is significantly higher among males (46.1 cases/100 thousand population per year), while for women it is 7.5/100 thousand population, i.e. the ratio of SCD cases in men/women is 6.1:1.0. In 80% of cases, SCD occurs at home, including cardiac arrest during sleep, and about 15% - in a public place/on the street.
The proportion of cardiac arrest during sleep is higher than during wakefulness. The sudden and unpredictable nature of cardiac arrest, and the high incidence of deaths, along with the extremely low level of effective and successfully performed resuscitation measures, make the problem of SCD in clinical cardiology an extremely complex and difficult to resolve problem not only in emergency medicine in Russia, but in all countries in general.
The complexity of resuscitation measures is due to the fact that only a short-term cardiac arrest (no more than 5-6 minutes) provides the opportunity to restore physiologically normal activity of the higher parts of the brain under hypoxic . How long does the brain live after the heart stops working? It is generally accepted that under conditions of oxygen starvation (clinical death), a disruption of the barrier function of brain cell membranes occurs, which consists of an increase in permeability to electrolytes and water.
Already in the first 1-2 minutes, mono-divalent ions (H+, Na+, Cl–) and high-molecular protein compounds enter the cells of the cortex and brain structures. A decrease in ATP and cessation of energy metabolism disrupts the processes of protein synthesis and their physicochemical properties, fat metabolism and electrolyte composition, which causes complex intracellular changes. The rapid movement of potassium and sodium ions leads to a sharp increase in osmotic pressure and the development of “osmotic shock” and swelling of the tissues of brain structures. That is, the brain dies (biological death) 5 minutes after blood circulation stops.
Given the relatively high prevalence of SCD in the general human population and the fact that cardiac arrest in the presence of medical personnel with a relatively high chance of successful resuscitation is rare, early identification of individuals at increased risk of developing cardiac arrest is of particular importance.
How many people survive clinical death safely?
It may seem that most people who find themselves in a state of clinical death come out of it safely. However, this is not the case; only three to four percent of patients can be resuscitated, after which they return to normal life and do not suffer from any mental disorders or loss of body functions.
Another six to seven percent of patients, being resuscitated, nevertheless do not fully recover and suffer from various brain lesions. The vast majority of patients die.
These sad statistics are largely due to two reasons. The first of them is that clinical death can occur not under the supervision of doctors, but, for example, at the dacha, from where the nearest hospital is at least half an hour’s drive. In this case, doctors will arrive when it is no longer possible to save the person. Sometimes it is impossible to defibrillate in a timely manner when ventricular fibrillation occurs.
"Special Report": Beyond
The second reason remains the nature of the damage to the body during clinical death. If we are talking about massive blood loss, resuscitation measures are almost always unsuccessful. The same applies to critical myocardial damage during a heart attack.
For example, if a person has more than 40 percent of the myocardium affected as a result of blockage of one of the coronary arteries, death is inevitable, because the body cannot live without heart muscles, no matter what resuscitation measures are taken.
Thus, it is possible to increase survival rate in case of clinical death mainly by equipping crowded places with defibrillators, as well as by organizing flying ambulance teams in hard-to-reach areas.
Pathogenesis
Cardiac arrest is based on shifts in the gas composition of the blood and acid-base balance towards oxidation, which leads to disruption of metabolic processes, inhibition of conductivity, changes in excitability in the heart muscle and, as a result, disruption of the contractile function of the myocardium. A wide range of pathologies, different causes and types of contributing factors form different mechanisms of cardiac arrest. The cessation of cardiac activity may be based on different types of cardiac arrest, the main of which are: cardiac asystole and ventricular fibrillation .
What is cardiac asystole? Asystole means the complete cessation of contractions of the muscles of the atria and ventricles in the genesis of which is the complete cessation of the process of transfer of excitation from the sinus node in the absence of impulses in secondary foci of automaticity. This includes:
- asystole of the entire heart with impaired/complete blockade of conduction between the sinus node and the atria;
- ventricular asystole in the presence of complete transverse block;
- pronounced ventricular bradycardia against the background of incomplete blockade of conduction between the ventricles and atria.
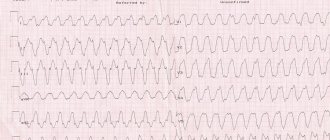
Asystole can occur reflexively (suddenly) with still preserved myocardial tone or gradually (with preserved myocardial tone or with its atony). Cardiac arrest most often occurs in diastole and is much less common in systole. In Fig. The ECG below shows an agonal rhythm turning into asystole .
Ventricular fibrillation is understood as an asynchronous (chaotic and scattered) contraction of the muscle fibers of the heart, leading to disruption of the function of blood supply to organs and tissues. In this case, vigorous fibrillary contractions are observed (with normal myocardial tone) or sluggish (with its atony).
The main mechanism of cessation of blood circulation in most cases (85%) is ventricular fibrillation, the development of which is facilitated by factors that reduce the electrical stability of the myocardium: decreased cardiac output, increased heart size ( aneurysm , hypertrophy , dilatation ), increased sympathetic activity.
The cause of ventricular fibrillation is disturbances in the conduction of excitation in the conduction system of the ventricles. The preliminary stages of cardiac fibrillation are:
- ventricular fibrillation and flutter;
- paroxysmal tachycardia , which is caused by impaired intraventricular/intraatrial conduction.
In Fig. Below is an ECG for large-wave and small-wave ventricular fibrillation.
There are several theories to explain the mechanisms of heart rhythm disturbances during fibrillation, the most significant of which are:
- The theory of heterotopic automatism, which is based on the appearance of numerous foci of automatism that arise as a result of “overexcitation” of the heart.
- The theory of "ring" rhythm. According to its provisions, excitation continuously circulates throughout the myocardium, which leads to contraction of individual fibers instead of simultaneous contraction of the entire muscle.
An important mechanism for the occurrence of ventricular fibrillation is the acceleration of the excitation wave. In this case, only muscle fibers contract, which by that time had left the refractory phase, which causes chaotic contraction of the myocardium.
Also, disturbances in electrolyte balance (potassium and calcium) are of great importance in the development of pathology. Under conditions of a hypoxic state, intracellular hypokalemia , which in itself increases the excitability of the heart muscle, which is fraught with the development of paroxysms of disruption of sinus rhythm. Also, against the background of intracellular hypokalemia, myocardial tone decreases. However, cardiac activity is disrupted not only with the development of intracellular hypokalemia, but also with a change in the ratio/concentration of K+ and Ca++ cations. Such disorders lead to changes in the cell-extracellular gradient with a disorder in the processes of excitation/contraction of the myocardium. In addition, a rapid increase in plasma potassium concentration against the background of its reduced level in cells can cause fibrillation. Intracellular hypocalcemia can also contribute to the loss of the myocardium's ability to fully contract.
In general, regardless of the genesis of SCD, cardiac arrest must be based on a factor leading to the occurrence of SCD and disability of the heart muscle. The BCC formula can be presented as: BCC = substrate + trigger factor.
Where the substrate refers to anatomical/electrical abnormalities caused by heart disease, and the trigger factor refers to metabolic, mechanical and ischemic influences.
What types of stops exist and how do they differ from each other?
What we see in films as a straight line is not the only option for stopping the myocardium. Often electrical activity is observed, but there is no normal blood circulation.
The types of cardiac arrest are as follows:
- Ventricular fibrillation is the name given to chaotic, disorderly contractions of individual myocytes. As a result, the heart seems to flutter, but the pumping function is lost. In this case, electrical defibrillation is effective.
- asystole - this type is characterized by a complete absence of contractions and electrical activity. A straight isoline is observed on the cardiogram.
- electromechanical dissociation - in this case, individual QRS complexes are observed on the ECG, but contractions do not occur, and there is no blood pressure.
Classification
Cardiac arrest is distinguished by:
- cause of heart disease (sudden cardiac death), among which, depending on the time interval between the onset of a heart attack and the onset of death, instantaneous (almost instantly) and rapid cardiac death (within 1 hour) are distinguished.
- non-cardiac causes (rupture of an aneurysm of large vessels, drowning, thromboembolism of the pulmonary artery or cerebral vessels, airway obstruction, electric shock , shock of various etiologies, embolism, drug overdose, exogenous poisoning, etc.).
Causes of cardiac arrest
The main causes of cessation of cardiac activity in sudden cardiac death:
- Ventricular fibrillation (the proportion of cases of cardiac arrest is 75-80%);
- Ventricular asystole (in 10-25% of cases);
- Ventricular paroxysmal tachycardia (up to 5% of cases);
- Electromechanical dissociation (in 2-3% of cases) - the presence of electrical activity of the heart in the absence of mechanical activity.
The leading etiological factors for a high risk of sudden cardiac death are:
- Previous myocardial infarction .
- Cardiac ischemia.
- Non-ischemic cardiomyopathies (hypertrophic, dilated and arrhythmogenic right ventricular cardiomyopathy ).
- Diseases of the valvular apparatus of the heart (mitral, aortic stenosis , aortic valve insufficiency).
- Abnormalities of the thoracic aorta, dissection or rupture of aortic aneurysm.
- Long QT syndrome.
- Sick sinus syndrome.
- Arterial hypertension.
- Heart rhythm and conduction disorders.
Minor risk factors include:
- Hyperlipidemia / atherosclerosis (high cholesterol ).
- Extreme physical stress.
- Abuse of strong alcoholic drinks and drug use.
- Smoking.
- Severe electrolyte disturbances.
- Overweight/ obesity .
Extracardiac causes of cardiac arrest can be:
- Shock states of various origins.
- Obstructions in the respiratory tract.
- Emboli.
- Reflex cardiac arrest.
- Heart injuries.
- Electric shock. Overdose of drugs that cause cardiac arrest. First of all, you should not just look for which pills cause cardiac arrest, but understand that this is only possible in cases of overdose or self-administration of medications without a doctor’s prescription.
- Drugs that can cause cardiac arrest include: tricyclic antidepressants ( Amitriptyline , Tianeptine , Sertraline , Pyrazidol , Clomipramine , etc.), which can cause a slowdown in the conduction of excitation; antiarrhythmic drugs: Sotalol , Aprinidine , Disopyramide , Dofetilide , Encainide , Cordarone , Bepridil , Bretilium , Sematilid , etc.; drugs for the treatment of hypertension and angina - Nifedipine in high doses (above 60 mg per day), which increases the risk of ventricular fibrillation.
It should be noted that drugs that cause cardiac arrest can have a negative effect only if they are significantly overdosed or the conditions for their safe use are violated, for example, taken with alcohol or before/after taking alcohol-containing drinks or while taking narcotic substances.
What can cause the heart to suddenly stop beating?
Typically, myocardial arrest occurs due to pathologies of the cardiovascular system (so-called cardiogenic causes). But often the triggering factor is other acute or chronic diseases, as well as injuries and accidents (non-cardiogenic).
| Cardiogenic causes | Non-cardiogenic causes |
| Myocardial infarction | Stroke |
| Acute and chronic heart failure | Carrying out heart surgery (stenting, valve replacement) |
| Defects of heart structures | Oncological diseases |
| Cardiomyopathies | Infectious pathologies |
| Myocarditis | Complications of bronchopulmonary diseases (respiratory failure, respiratory distress syndrome) |
| Hypertensive crisis | Endocrine disorders (diabetic, hypothyroid, thyrotoxic coma) |
| Heart rhythm disturbances | Acute hypercalcemia and/or hypokalemia |
| Cardiogenic shock | Sepsis |
| Pulmonary embolism | Pancreatic shock |
| Aortic aneurysm | Acute renal and/or liver failure |
| Cardiac tamponade |
Isolated episodes that can cause cardiac arrest include:
- Anaphylactic shock (due to anesthesia, local anesthesia, taking antibiotics and other drugs, insect bites);
- Poisoning (including alcohol and drugs);
- Massive burns;
- Hypo- and hyperthermia;
- Electrical injuries;
- Suffocation.
Causes in children and young people
Most often, older people die from heart failure. However, there are reasons that can cause it in children or young people. They are usually caused by the above conditions associated with trauma and other damage, as well as serious arrhythmias. But there are also some specific pathologies.
So, before the age of one year, sudden infant death syndrome may occur. In such a case, a disturbance in the heartbeat and breathing develops against the background of absolute external well-being, most often at night and during sleep.
Risk factors for sudden infant death may include:
- sleeping on a bed that is too soft in an unventilated room on the stomach - in this case, the baby may simply suffocate;
- multiple pregnancy;
- prematurity;
- delivery by caesarean section;
- bad habits of the mother during pregnancy.
During pregnancy, for one reason or another, fetal cardiac arrest may occur. Most often this happens due to undiagnosed intrauterine developmental disorders of the embryo or genetic pathologies.
Athletes often experience sudden death due to Commotio Cortis syndrome. It occurs as a result of a sharp and strong blow to the heart at the time of diastole. Such an action can cause the reflex development of a dangerous arrhythmia, for example, ventricular fibrillation.
The following sports are considered dangerous in this regard:
- martial arts;
- baseball;
- American football;
- hockey.
Symptoms of cardiac arrest
Let's look at the symptoms that can help identify cardiac arrest. The main signs of cardiac arrest are given below.
Loss of consciousness. Identified using sound effects (loud clapping, shouting) or patting the face.
Absence of pulse in large arteries. The best option for determining the pulse is the carotid artery. To do this, you need to place your fingertips in the middle part of the neck on the front surface of the trachea and, pressing the fingers against the skin, move them to the right side surface of the neck until they stop at the edge of the muscle. With a slight increase in pressure under the fingers, a pulsation should be felt in the carotid artery (Fig. below).
Lack of breathing. To determine the presence/absence of breathing, use visual, auditory and contact control:
- Place your hand on the victim's chest and determine the presence/absence of movement (excursion) of the chest.
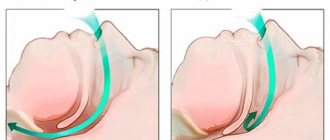
- Apply your face (the cheek is especially sensitive) to the victim’s mouth/nose and look for air movement coming out of the airway or breathing sounds (picture below).
Dilated pupils that do not respond to light (the pupils do not constrict). To do this, you should lift the upper eyelid with your finger and look at the pupil: if the pupils remain wide when exposed to light and do not narrow, a conclusion is made that the pupil does not react to light. At night, you can use a flashlight for this purpose. (picture below).
Pale grey/bluish complexion. That is, the natural pinkish color of the facial skin changes to gray, which indicates a lack of blood circulation.
Complete relaxation of all muscles, which may be accompanied by involuntary release of feces/urination.
Symptoms and signs of the condition
In fact, in medicine, short-term cardiac arrest is considered the equivalent of clinical death. So the symptoms for these conditions are almost the same:
- complete loss of consciousness. The person does not respond to sound and pain stimuli;
- a very short time after stopping, short-term convulsions may appear;
- breathing is either completely absent or very rare and intermittent.
- the skin is very pale and covered with sweat, but on the tips of the fingers, nose, and lips it becomes cyanotic (blue);
- There is no pulse in both the peripheral (wrist) and main arteries (carotid, neck).
- it is also impossible to feel the heartbeat to the left of the sternum;
- the pupils do not react (do not constrict) when light is directed at them;
- expression of fear on the face.
Above are the expanded symptoms of clinical death. However, the European Association of Resuscitation Medicine recommends that persons without medical education limit themselves to only checking the patient’s consciousness and breathing.
Such limitations are due to the fact that there is very little time, and in extreme situations an ordinary person can become confused, afraid and not complete all resuscitation and diagnostic procedures. In addition, when checking the activity of the heart, the so-called “false pulse syndrome” occurs - due to the release of adrenaline, a person can feel his own pulse on the deceased.
First of all, the patient needs to check consciousness:
- Call out to the victim loudly (preferably in his ear).
- if he does not respond, apply a painful stimulus. For example, firmly pinch the upper edge of the trapezius muscle.
- if he does not react at all, this means that there is no consciousness, proceed to the breathing test.
Breathing assessment is carried out as follows:
- Tilt the victim's head back to clear the airway and open the mouth.
- If there are foreign bodies in your mouth, remove them - they may be interfering with breathing.
- Lean over the victim and listen to his breathing for 10 seconds. At the same time, you will feel the movement of air in your cheek and observe the rise of your chest. There should be at least 2-3 breaths in 10 seconds.
- If there is no breathing or less than 2 breaths are recorded, it can be considered that cardiac arrest has occurred and this is an indication for CPR.
Prevention
General nonspecific measures to prevent cardiac arrest include:
- Timely diagnosis and treatment of diseases of the cardiovascular system.
- Control blood pressure and cholesterol levels.
- Quitting alcohol abuse and smoking.
- Moderate physical activity.
- Rational and balanced nutrition.
- Monitoring the correct intake of medications.
- Elimination of hypothermia, extensive injuries with large blood loss.
Consequences and complications
Against the background of cardiac arrest, even in cases of effective emergency therapy, in the medium term the development of ischemic damage to the brain, kidneys, liver and other organs is possible. There is a high risk of developing complications due to improper technique of cardiopulmonary resuscitation in the form of rib fractures at their connection to the sternum/midclavicular line. In this case, pinpoint hemorrhages may occur, merging into foci on the anterior/posterior surface of the heart in places where the heart is compressed by the sternum and spine.
How to act and what to do first
The future fate of the patient largely depends on the quality and timeliness of first emergency care.
Once you have determined the absence of cardiac activity, it is necessary to begin resuscitation measures, which consist of external cardiac massage and artificial ventilation:
Call an ambulance, or ask someone present to do so, and proceed to cardiopulmonary resuscitation;- Find the point on the sternum that is located on the border of the lower and middle third;
- Place the base of your palms there;
- Start pressing with such force that the chest goes down to a depth of 5-6 cm, maintaining a frequency of 100-120 compressions per minute (about two per 1 second);
- After 30 presses, take two breaths into the victim’s mouth, while making sure that the nose is closed
- Don't stop until the ambulance arrives, there are signs of life, or you are unable to continue.
List of sources
- Yakushin S.S., Boytsov S.A., Furmenko G.I. and others. Sudden cardiac death in patients with coronary heart disease according to the results of the Russian multicenter epidemiological study of morbidity, mortality, quality of diagnosis and treatment of acute forms of coronary artery disease. Russian Journal of Cardiology 2011; 2 (88): 59-64.
- Bockeria O. L., Akhobekov A. A. Sudden cardiac death: mechanisms of occurrence and risk stratification. Annals of Arrhythmology 2012; 9(3): 5-13).
- Grishina AA Sudden coronary death at the prehospital stage. /AA Grishina, Ya.L. Gabinsky //Materials of the 9th All-Russian Scientific and Educational Forum Cardiology-2007. Moscow, 2007. - pp. 23-31.
- Bockeria L.A., Revishvili A.Sh., Neminushchiy N.M. Sudden cardiac death. – M.: GEOTAR-media, 2011. – 272 p.
- Revishvili A.Sh., Neminushchiy N.M., Batalov R.E. et al. All-Russian clinical recommendations for controlling the risk of sudden cardiac arrest and sudden cardiac death, prevention and first aid. 2021. Geotar-Med 256 p.