Mumps (colloquially called mumps) used to be one of the most common infections, affecting almost all young children. This continued until the 60s of the twentieth century, until vaccination against this disease was introduced. The pathology is acute, affecting mainly the parotid salivary glands. Viral cells can penetrate various organs of the body and the central nervous system, causing the development of serious complications.
Ways of transmission of the disease
Mumps is a disease that only affects humans. The mechanism of infection for mumps is almost always airborne. The pathogen is found in the saliva and mucous secretions of the patient, which are dispersed into the environment when talking, coughing or sneezing.
Indirect transmission of the virus is possible. You can become infected by contact with surfaces or surrounding objects that have been touched by someone with mumps. With unwashed hands, the infection enters the nasal or oral cavity of a healthy person and infection occurs.
Infection of healthy patients from a patient with mumps is possible in the prodromal phase, two days before the development of primary symptoms, and for five days after the onset of characteristic manifestations of the disease. Therefore, you should refrain from contact with an infected person for 5-6 days after clinical signs of mumps appear.
Symptoms of mumps (mumps)
The disease usually begins acutely. The following symptoms appear:
- temperature (over 38°C);
- headache;
- general weakness, loss of appetite;
- pain while chewing or talking.
Towards the end of the first or second day of the disease, swelling occurs in the area of the parotid gland; the skin becomes stretched, touching this place is painful. Usually one gland swells first, and the next day or every other day the second one, on the other side, swells. The patient's face takes on a puffy appearance. The maximum increase in glands occurs on the third day, after which the swelling begins to subside and within a week the face
Complications of mumps
Severe forms of mumps are associated with damage to various organs by the virus. The pancreas, testicles in boys and ovaries in girls are most often affected. Mumps can lead to infertility. Another serious complication, which unfortunately occurs quite often, is meningitis.
Symptoms
The clinical picture of mumps, which occurs in adults and children, has almost the same manifestations. The only difference is that in adult patients the pathology is characterized by a more acute course.
There are three main symptoms of mumps:
- Hyperthermia – the body temperature of an infected person rises suddenly. The thermometer readings immediately reach critical values. At the same time, it is almost impossible to reduce the temperature with the help of medications in such a case. Although there is no need to worry about this - the immune system itself must eliminate the inflammatory process and produce antibodies to the virus. If the fever persists for a sufficiently long time after the other symptoms of mumps have subsided, then this already indicates the development of another disease.
- Swelling of the salivary glands behind the ears - this sign is the most striking evidence of the presence of mumps in a child or adult. The swelling is always large, the area is painful to the touch, and swallowing and chewing food is difficult. Due to the symptoms of mumps, the patient's appearance changes - the cheeks become larger and droop, and the earlobes rise slightly. These manifestations disappear 7-8 days from the start of therapy.
- Poor health and weakness - children infected with mumps are usually lethargic and indifferent. In adults, the disease is more severe; they suffer the disease while lying down. Often with this pathology, patients are irritated by extraneous sounds, photophobia and headaches occur.
How to identify infertility after mumps
As a rule, the effects of mumps are not symptomatic. Patients who have had mumps do not experience problems in their sexual life and think about treatment only after prolonged unsuccessful attempts to conceive a child.
To diagnose male infertility, the patient takes a spermogram. Laboratory examination of sperm allows you to see the morphology of sperm, their structure and quantity.
The diagnosis is confirmed by the results of a spermogram, according to which the absence of active healthy sperm is detected in the seminal fluid or their number is negligible for natural fertilization.
Ultrasound of the scrotum reveals areas of necrotic tissue and testicular atrophy. If neoplasms are detected during diagnosis, a biopsy is prescribed. Selected tissues are examined in the laboratory to exclude or confirm oncology.
Complications after mumps
Mumps provokes the development of various disorders in the body. With this disease, in addition to the salivary glands, other organs can be affected; usually, such complications occur in post-pubertal patients. Among them are:
- Damage to the reproductive system - develops in 15-20% of adult men in the form of orchitis (inflammation of the testicles). The disorder usually manifests itself on one side, causing pain in the scrotum, swelling and hyperemia, high sensitivity and a feeling of heat in the problem area. Sometimes the inflammation process ends with testicular atrophy. Oophoritis may occur in women, but it is much less common and is characterized by milder symptoms.
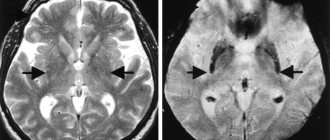
- Disruption of the central nervous system - this complication of mumps is observed in 1-10% of patients and is expressed in the form of meningitis and encephalitis. The first occurs with the presence of vomiting, migraine, and decreased neck mobility. Signs of encephalitis include seizures, drowsiness, or coma.
- Pancreatitis - occurs on the 6-7th day of the disease. Its clinical signs include stomach pain, vomiting and nausea. The pathology disappears on its own 13-14 days after the first symptoms appear.
Very rare complications of mumps are: nephritis and polyarthritis, prostatitis, hepatitis, deafness, mastitis and myocarditis.
Mumps is an acute infectious disease caused by a virus of the paramyxovirus family. The main signs of the disease are intoxication and inflammation of the parotid salivary glands. In some cases, other organs may be involved in the pathological process: the nervous system, testicles, pancreas. After the disease, in almost all cases, stable lifelong immunity is formed.
There is a vaccine against mumps that can significantly reduce the risk of infection, and before the introduction of mass vaccination, it was widespread. Nowadays, outbreaks of infection are quite rare in developed countries. Most often, children aged 2-12 years become ill, although recently the percentage of adults among those who become ill has increased - those who were not vaccinated in a timely manner and who, as a result of vaccination, did not develop a sufficiently strong immunity.
The prognosis for mumps is generally favorable. Complications are quite rare and in most cases do not lead to irreversible pathological changes. However, sometimes mumps can cause infertility, deafness, and neurological problems.
Synonyms Russian
Mumps, mumps, ear infections.
English synonyms
Parotitis, mumps.
Symptoms
The initial stages of the disease are characterized by nonspecific symptoms of general intoxication. About 20% of patients experience virtually no discomfort - the disease can be unnoticeable. The most characteristic sign of mumps - inflammation of the parotid salivary glands - develops only on the third day of illness or may be completely absent.
The main symptoms of mumps are:
- fever,
- malaise,
- loss of appetite,
- swelling, pain in the area of the parotid salivary gland on one or both sides, which intensifies when chewing, drinking sour drinks, or talking.
General information about the disease
The mumps virus belongs to the paromyxovirus family and is structurally similar to the influenza virus. It consists of single-stranded RNA surrounded by a glycoprotein shell.
You can become infected from an infected person through airborne droplets. The virus is not stable in the external environment. The incubation period, that is, the time between contact with the source of infection and the appearance of symptoms, is 2-3 weeks. A sick person is contagious two days before the first symptoms and for about a week after their onset. Uncomplicated mumps usually lasts about seven days, rarely up to ten.
Children aged 2-12 years are most susceptible to mumps. During the first year of life, the child's body is usually protected by maternal antibodies. At the same time, in adults the disease is more severe.
The onset of mumps is usually accompanied by nonspecific symptoms: fever, muscle pain, weakness, loss of appetite. The temperature is highest on the second day of illness. On the third day, 95% of patients experience swelling and pain in the area of the parotid salivary glands, after which the manifestations of general intoxication begin to subside. Swelling of the salivary glands persists for up to 10 days. Inflammation of the parotid salivary glands can be unilateral or bilateral, the pain intensifies when chewing and swallowing. The skin over the glands is tense. The pain is especially pronounced when pressing in front of the earlobe and behind it, as well as in the mastoid area. Mursu's symptom is also observed - inflammation in the area of the excretory duct of the gland. The swelling may also spread to the neck area.
Complications of mumps are rare. The most common violations that occur are:
- Damage to the nervous system – encephalitis and meningitis. Mild forms of neurological disorders are observed in 10% of patients with mumps, but in the vast majority of cases they are completely curable and do not lead to serious consequences.
- Sensorineural deafness. Reversible hearing impairment develops in 4% of patients, but irreversible deafness is much less common and is often unilateral.
- Orchitis is an inflammation of the testicles that affects 20-50% of patients with mumps. Atrophic changes of varying degrees in testicular tissue occur in a third of patients, and fertility (the ability to conceive) may decrease, but infertility as a result of mumps is rare.
- Oophoritis is inflammation of the ovaries. It is very rare and does not lead to a decrease in fertility.
- Pancreatitis is inflammation of the pancreas. It affects 5% of patients with mumps. Changes in the pancreas are rarely irreversible, but several cases of diabetes mellitus have been identified due to damage to pancreatic cells by the virus.
In addition to the mumps virus, inflammation of the parotid salivary glands can be caused by cytomegalovirus, influenza and parainfluenza viruses, HIV infection, various bacteria, in addition, it can be associated with metabolic disorders, neoplasms, salivary stones, and taking a number of medications.
Who is at risk?
- Children from 2 to 12 years old.
- Aged people.
- Patients with reduced immunity.
- Those who have not been vaccinated or those who have not developed a sufficient level of immunity after vaccination.
Diagnostics
Diagnosis of mumps is based primarily on history and presenting symptoms. Additional diagnostic measures may be required to exclude other diseases with a similar clinical picture.
Laboratory diagnostics
- Complete blood count (without leukocyte formula and ESR). Leukocyte formula. With mumps, leukopenia with relative lymphocytosis can be detected.
- Erythrocyte sedimentation rate (ESR). This is a nonspecific sign of inflammation. With mumps it is increased.
- C-reactive protein. With mumps it is sometimes elevated.
- Total amylase in daily urine and total amylase in serum. Amylase is an enzyme produced by the pancreas and salivary glands. It is necessary for the digestion of carbohydrates contained in food. With pathology of the salivary glands or pancreas, the level of amylase in the blood and urine may be increased.
- Pancreatic amylase. Increased with damage to the pancreas.
- Determination of antibodies to the mumps virus in the blood. Class M immunoglobulins and class G immunoglobulins to the mumps virus are detected. IgM is responsible for the primary immune response and appears in the blood in the first days of the disease. IgG begins to be produced a little later.
Other research methods
- X-ray (sialography), computed tomography, magnetic resonance imaging of the salivary glands. These methods make it possible to assess the condition of the glands, identify neoplasms, salivary stones, disturbances in the outflow of secretions, and pathological changes in the tissues of the salivary gland or surrounding areas.
- Ultrasound of the testicle. May be required for orchitis.
In case of complications, the doctor may prescribe a number of additional tests.
Treatment
There is no specific treatment for mumps; therapy is prescribed depending on the symptoms. Bed rest is of great importance, reducing the risk of complications several times. Patients with complications, severe concomitant diseases, as well as all male patients over 12 years of age are subject to hospitalization.
Prevention
Prevention of mumps involves timely vaccination. It is given to all children aged 12-15 months, usually as part of a comprehensive vaccination against measles, rubella and mumps. Vaccination against mumps is repeated at the age of 4-6 years.
Recommended tests
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein, quantitative
- Total amylase in daily urine
- Serum total amylase
- Mumps Virus, IgM
- Mumps Virus, IgG
Therapeutic measures
There are no specific treatments for mumps. Treatment is mainly aimed at reducing clinical manifestations and preventing complications of this disease. Patients are prescribed antibacterial agents and novocaine blockades. Be sure to adhere to bed rest, diet and drink plenty of fluids.
In order for the immune system to defeat the virus, the patient needs good rest and sleep for 1.5-2 weeks. The menu of such a patient should not include spicy, fried, fatty and starchy foods. You need to take food in small portions and often.
If a child gets mumps, his diet should consist of plant and dairy products. With mumps, the patient is bothered by severe dryness in the oral cavity, so the oral mucosa must be constantly moisturized. That is why such patients are recommended to drink frequently in large volumes.
Anti-inflammatory and antihistamine medications are prescribed for mumps. It would also be a good idea to take vitamins and antitoxic drugs.
Effective therapy for the disease
The main task of doctors in the process of treating mumps is to prevent the development of complications. The patient is prescribed strict bed rest for 10 days or longer, depending on the condition. Statistics show that if bed rest is not followed, cases of orchitis develop three times more often than in those who follow medical recommendations. In uncomplicated cases, the patient remains at home; hospitalization is necessary only if a severe complication occurs or to prevent further spread of the infection. It is important to provide the patient with proper care, including:
- drinking plenty of warm drinks to reduce intoxication by cellular decay products;
- liquid or semi-liquid food that does not require chewing;
- regular brushing of teeth and rinsing the mouth with boiled water or a weak soda solution;
- dry warm compresses on the tumor.
If complications develop, the doctor prescribes appropriate treatment according to the indications. Recovery occurs two to three weeks after the onset of the disease.
The most important factor in the prevention of mumps is the timely administration of a live vaccine to the child. Routine vaccination is carried out for one-year-old children with revaccination at 6 years of age. Older patients are vaccinated according to epidemiological indications. Statistics show that vaccinated children and adults get mumps much less often, and if infected, the risk of developing complications is significantly reduced.
Acute non-epidemic parotitis
Acute non-epidemic parotitis is inflammation of the parotid gland as a result of impaired salivation due to general and local factors.
Causes of non-epidemic mumps
The causes of non-epidemic mumps, as mentioned earlier, are general and local factors.
Common factors include infectious diseases, exhaustion of the body, and surgical interventions. Local factors: inflammation of the mucous membrane, foreign body in the excretory duct of the gland, lymphadenitis, otitis media, sinusitis.
Non-mumps clinic
The non-mumps clinic is quite vibrant. The patient complains of pain and swelling, most often in the area of one gland. Body temperature is above 39 C. Then the entire parotid area swells, the earlobe protrudes, difficulty swallowing and breathing appears, and after this xerostomia appears. Due to swelling, the skin in the outer ear area is smoothed, the ear canal is compressed, and hearing is reduced. When massaging the gland, a cloudy or purulent exudate appears. Inflammation increases for 3-4 days, then acute inflammatory reactions subside, and compaction remains in the area of the gland for a long time.
There are 3 forms of acute non-epidemic parotitis: catarrhal, purulent, gangrenous.
The purulent form is characterized by intense tearing pain. This occurs due to the accumulation of pus, formed from the breakdown of glandular tissue, under the capsule of the gland. Over time, a fistula may form in the external auditory canal, then spread into the peripharyngeal space with the formation of peripharyngeal phlegmon, up to mediastinitis.
The gangrenous form is characterized by extensive tissue necrosis and the development of mediastinitis, thrombosis, phlebitis, and sepsis.
Treatment of non-mumps
Treatment of non-epidemic mumps at the initial stage is conservative. A gentle diet, UHF, dry heat and compresses based on dimexide, anti-inflammatory drugs, and antibiotics are prescribed. Sulfonamide drugs intramuscularly and antibiotic-novocaine blockades subcutaneously and from the oral cavity along the excretory duct are indicated.
In severe cases, antibiotics are prescribed every 3 hours. Also, washing the excretory ducts with chymotrypsin has a good effect. For purulent forms, treatment is surgical. One incision is made along the angle of the jaw, the pancreas and parotid-masticatory fascia are dissected, and a second incision is made along the edge of the zygomatic arch and drainage is placed.
Prevention of non-epidemic mumps
Prevention of non-epidemic mumps includes good oral hygiene, administration of salivary agents in case of xerostomia and disinfectants that are secreted through the salivary glands (phenyl salicylate, hexamethylenetetramine).
Chronic mumps
Acute mumps rarely becomes chronic, so chronic mumps often occurs as a primary disease.
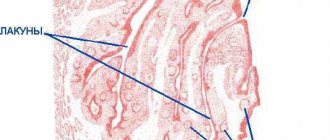
Chronic mumps are classified into 2 groups: parenchymal and interstitial.
Chronic parenchymal parotitis
Chronic parenchymal parotitis is often asymptomatic. However, the clinic is varied. Patients may complain of swelling, pain in the gland area, and a taste of pus in the mouth. The disease lasts a long time, periodically exacerbating. Most often one gland is affected.
Objectively we can see a swelling of the gland with clear contours. Palpation is painless, the gland is dense, the surface is lumpy. When massaging the gland - saliva with pus.
Diagnostics
For diagnosis, a contrast sialogram is performed. On the sialogram you can see deformation and/or necrosis of the ducts of 2-4 orders and the parenchyma of the gland - in the image there are cavities filled with a contrast agent. As the disease progresses, the cavities merge, areas of necrosis increase until the glandular tissue is replaced by fibrous tissue.
The radiosialographic method allows us to identify the stage of the disease. At the initial stage, there is a rapid accumulation of radioactivity. In the stage of pronounced signs - slow accumulation. In the late stage, radioactivity is low.
The cytological method for diagnosing punctate and gland secretions is also used.
Treatment of chronic parenchymal parotitis
Treatment of chronic parenchymal parotitis is difficult due to the inability of dead gland tissue to regenerate. Therefore, the dentist’s task is to relieve the disease.
The gland is stimulated with ocular probes and washed every day with antibiotic solutions and massaged, freeing it from solution and pus until clear saliva appears. The ducts can also be washed with chymotrypsin, a solution of potassium iodide. Novocaine blockades and radiotherapy are indicated.
With frequent relapses, extinguishing the function of the gland is carried out by three times instillation of ethyl alcohol with increasing concentrations of 60-80-96.
Surgical treatment: parotidectomy, extirpation of the parotid duct + denervation of the auriculotemporal nerve.