- What function do lymphocytes perform?
- Types of lymphocytosis
- Physiological lymphocytosis
- Lymphocytosis in viral diseases
- Lymphocytosis in bacterial infections
- Hematological diseases
- Endocrine system diseases
- Rheumatological, allergic and parasitic diseases
- Diagnosis of lymphocytosis
- Treatment of lymphocytosis
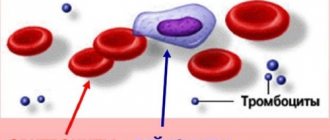
Lymphocytosis is a type of leukocytosis.
This is a condition in which the level of lymphocytes in the blood of an adult exceeds 4000 units, and in children under 5 years of age - 6000 units per microliter. In percentage terms, this ranges from 40% or more for adults and 55% for young children. Normally, the blood of a healthy adult contains 20-40% lymphocytes. Lymphocytosis can occur for physiological and pathological reasons. As a rule, in most cases it is one of the symptoms of the disease. The cause of lymphocytosis can be not only blood diseases, but also viruses, infections, and certain physiological reactions.
To diagnose lymphocytosis, venous or capillary blood is used. Laboratory testing determines the main blood parameters, including the level of lymphocytes.
What function do lymphocytes perform?
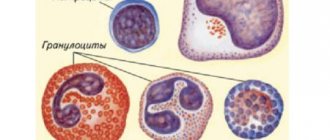
These blood cells provide the body's defense against pathogens. Lymphocytes produce immunoglobulins - antibodies that bind to viral infection and thereby prevent it from entering the cells of organs and tissues. Lymphocytes are also part of the mechanism to destroy cells that are already infected with the virus. In a similar way, lymphocytes can fight certain types of bacterial and parasitic infections. Thus, an increase in lymphocytes in the blood is the response of the immune system when an infection enters the body.
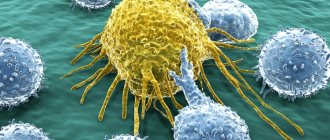
Causes of development of chronic lymphocytic leukemia
Possible etiological factors for the development of chronic lymphocytic leukemia include:
- chromosomal mutations
- hereditary predisposition
- viral infections
According to a number of scientists, long-term stimulation of the human immune system (for example, during frequent infections) can lead to genetic damage and tumor degeneration of lymphocytes, the formation of a clone of leukemic cells and the occurrence of CLL.
A direct causal relationship between exposure to carcinogens and ionizing radiation and the occurrence of CLL has not been established.
The mechanism of development of chronic lymphocytic leukemia is the transformation of lymphocytes into tumor cells and their proliferation, which leads to inhibition of normal hematopoiesis, the development of anemia and thrombocytopenia.
Types of lymphocytosis
The disease is divided into relative and absolute types. Relative is characterized by an increase in the number of lymphocytes against the background of normal or reduced levels of leukocytes in the blood.
With absolute lymphocytosis, the level of lymphocytes is exceeded, as is the content of leukocytes.
According to the degree of excess, moderate and high lymphocytosis are distinguished. If the percentage of lymphocytes is below 60%, we are talking about moderate lymphocytosis. When the lymphocyte content is high, it is above 60%, which may be a sign of a malignant hematological disease or diseases of the lymphatic system.
Physiological lymphocytosis
Sometimes an increase in lymphocytes is not associated with a disease and is a natural reaction of the body. The main reasons for this phenomenon are:
- early childhood;
- psycho-emotional stress;
- fasting, avoidance of animal products;
- taking certain medications.
In children under 4-5 years of age, an increased level of lymphocytes is a physiological norm. Already from the first week of life in a newborn, the lymphocyte count reaches 55-60%. This is due to age-related characteristics of the immune system. By 4-5 years, the level of lymphocytes decreases to 40%. If in a small child this figure exceeds 60%, this is a pathology.
As for lymphocytosis during stress, fasting, and taking medications, the change in the leukocyte formula is short-term. The indicators return to normal as soon as the causative factor ceases to affect the body.
Classification
There are no clear numerical criteria for dividing lymphocytosis according to severity. Conventionally, moderate (up to 60%) and high lymphocytosis (more than 60%) are distinguished. The main cause of high lymphocytosis is considered to be malignant diseases of the hematopoietic and lymphatic tissue. Lymphocytosis, like other types of leukocytosis, is divided into:
- Absolute
. Absolute lymphocytosis means an increase in the number of lymphocytes along with the total number of leukocytes (in adults more than 4000, in children under 5 years of age more than 6000). - Relative
. Relative lymphocytosis is much more common and means a percentage increase in lymphocytes (more than 40%) against the background of a normal or even reduced total number of leukocytes.
Lymphocytosis in viral diseases
Diseases caused by viruses are a common cause of lymphocytosis. In adults, it occurs with influenza and acute respiratory infections. In children - with chickenpox, measles, rubella. As a rule, patients are diagnosed with moderate lymphocytosis, which occurs as the symptoms of the disease increase. After recovery, blood counts return to normal.
The exception is infectious mononucleosis caused by the Epstein-Barr virus. The pathogen belongs to the herpevirus family. It multiplies in B lymphocytes and stimulates their growth. Adults and children are susceptible to this disease, but in childhood the risk of getting sick is much higher. In middle-aged and mature people, the pathology occurs without pronounced symptoms, since specific immunity has already been formed.
Against the background of infectious mononucleosis, persistent moderate lymphocytosis is observed. In addition, atypical mononuclear cells are found in the blood - large cells characteristic of the disease.
Lymphocytosis in bacterial infections
Some diseases caused by pathogenic bacteria also result in lymphocytosis. As a rule, we are talking about diseases that have a chronic course. In adults, lymphocytosis is diagnosed against the background of tuberculosis, syphilis, brucellosis, and various forms of typhoid diseases. In children, a similar condition is observed with whooping cough.
Changes in leukocyte counts depend on the nature of the pathology. In the chronic form, there may be a slight or moderate increase in levels that persists for several months or even years. If the disease worsens, the number of lymphocytes increases as symptoms increase.
What determines the degree of lymphocyte enlargement?
According to popular belief, the severity of the disease can be judged by how much the patient’s tests are changed. In some cases this is true. For example, the severity of jaundice is determined by the content of bilirubin in the blood (the more it is, the more serious the situation), and by the erythrocyte sedimentation rate - the degree of activity of rheumatic diseases. But with lymphocytes everything is not so simple. For example, with the same viral infection they can be normal, elevated, and sometimes it even happens that with ARVI, lymphocytes are reduced.
It is also appropriate to remember that there is such a thing as hyperimmunity. In this case, in response to the slightest irritation, for example to a slight viral runny nose, a huge number of lymphocytes are produced, and the test results terrify the attending physician, who immediately begins to suspect the person has lymphocytic leukemia. But in fact, the nature of such changes is only that the patient’s immunity reacts strongly to any threat.
In general, if a person has elevated lymphocytes, the reasons for this should be determined not by their number, but by their general health, symptoms, data from other studies, and the results of a conversation with a doctor.
If the doctor identifies any disease, the patient needs to follow the proposed treatment regimen in order to quickly bring the level of lymphocytes and general health back to normal. To achieve faster and better results, it is recommended to take Transfer Factor.
– a special tool created on the basis of information molecules. It has a universal training effect on the immune system and normalizes its functioning, regardless of what exactly the person is sick with. Taking the drug gives positive results in the treatment of most diseases.
Hematological diseases
High lymphocytosis is observed in diseases of the hematopoietic system and lymphatic tissue. Malignant diseases cause proliferation - uncontrolled cell division and tissue growth. In myeloproliferative and lymphoproliferative diseases, a corresponding change in cells in the bone marrow occurs.
The most common hematopoietic diseases that cause lymphocytosis are lymphosarcoma, lymphogranulomatosis, and chronic leukemia. Lymphocyte counts in such pathologies can reach 70-90%. Growth occurs gradually, reaching a maximum several years after the onset of the disease. To treat lymphocytosis, it is necessary to address the underlying cause that led to an increase in the number of lymphocytes. Chemotherapy courses and bone marrow transplants help bring lymphocyte counts back to normal.
In addition to malignant diseases of the hematopoietic system, lymphocytosis occurs against the background of anemia caused by deficiency of vitamin B12 and folic acid. In patients who have undergone blood transfusion, an increase in the number of lymphocytes may appear as one of the signs of post-transfusion syndrome.
Endocrine system diseases
Diseases that are accompanied by impaired hormonal secretion also cause lymphocytosis. What causes this reaction has not yet been precisely established. A moderate increase in lymphocytes is observed in acromegaly, a pathology that is accompanied by an increase in the production of growth hormone by the pituitary gland.
Thyrotoxicosis - excess secretion of thyroid hormones - can also lead to lymphocytosis. The same is observed in patients with adrenal insufficiency. In children with congenital dysfunction of the gonads, an increase in the number of lymphocytes is observed.
In all of these cases, the condition can be corrected by prescribing hormonal therapy.
Symptoms of chronic lymphocytic leukemia
In the initial stage of CLL, patients do not complain, their general condition is satisfactory. Some may experience nonspecific symptoms such as: severe sweating, fatigue, weakness, and frequent colds. At this stage, CLL is usually discovered by chance during a routine examination or when visiting a doctor about another disease. The disease is manifested by absolute lymphocytosis in a general blood test and an increase in peripheral groups of lymph nodes (cervical, axillary, inguinal). Enlarged lymph nodes in CLL are soft on palpation - elastic, painless, not fused with the surrounding tissues, the skin over them is not changed.
With a slow course, the initial stage can last several years; with a progressive course, there is a rapid deterioration in the general condition, a significant enlargement of the lymph nodes and spleen.
The advanced stage of CLL is characterized by the severity of symptoms. The main clinical manifestations include:
- intoxication syndrome: severe weakness, fatigue, decreased performance, a sharp decrease in body weight, significant sweating at night, an unexplained increase in body temperature;
- progressive lymphadenopathy: almost all groups of lymph nodes enlarge. They are soft-elastic to the touch, painless, not fused with the surrounding tissues, and can merge into conglomerates;
- infiltration of all organs and systems by tumor cells with a decrease in their function.
In this case, the following are observed:
- enlarged spleen;
- enlargement of the liver, which is associated with the syndromes of portal hypertension (dilation of the esophageal veins, accumulation of free fluid in the abdominal cavity, liver failure) and cholestatic jaundice (pain in the right hypochondrium, nausea, yellow discoloration of the skin and sclera, itching, discoloration of stool, darkening urine);
- gastrointestinal ulcers, malabsorption syndrome (malabsorption in the intestines, accompanied by abdominal pain, diarrhea), dyspeptic disorders (nausea, bloating, feeling of heaviness), as a result of infiltration of the gastrointestinal tract;
- frequent pneumonia and other respiratory tract infections, respiratory failure due to the accumulation of tumor cells in the lungs.
In the general blood test - leukocytosis (50-200*109/l), lymphocytosis (up to 100*109/l or 80-90% in the leukocyte formula), anemia and thrombocytopenia, increased ESR, Botkin-Gumprecht cells (destroyed lymphocytes).
End-stage CLL is characterized by:
- a sharp significant deterioration in general condition;
- prolonged high body temperature;
- exhaustion;
- severe generalized infections (staphylococcal, streptococcal, herpetic, tuberculosis, etc.);
- severe renal failure (characterized by oligoanuria, increased blood urea and creatinine);
- severe anemia;
- severe thrombocytopenia;
- hemorrhagic syndrome;
- due to the infiltration of the meninges by tumor cells, the development of neuroleukemia, manifested by severe headache, vomiting, paresis and paralysis, and the development of meningeal symptoms, is possible;
- infiltration of the spinal roots is accompanied by intense shooting “radicular” pain;
- the development of severe cardiomyopathy, manifested by progressive heart failure and cardiac arrhythmias, is possible.
Rheumatological, allergic and parasitic diseases
In patients with systemic lupus erythematosus, rheumatoid arthritis, and rheumatic fever, there is a change in the leukocyte blood count towards an increase in the number of lymphocytes.
Allergy sufferers and patients with bronchial asthma also experience a similar condition.
When infected with schistosomiasis, a parasitic infection caused by helminths of the genus Schistosoma, the level of lymphocytes increases against the background of damage to internal organs. The most rare causes of lymphocytosis include tropical infections: malaria and Chagas disease. The carriers of such infections are insects; infection occurs through a bite. In our country, travelers who visit countries in Latin America, Africa, and the states of the Western Pacific are at risk of contracting such diseases.
Diagnosis of lymphocytosis
A clinical blood test helps to identify excess lymphocytes. An adult patient can go to a medical laboratory for an examination, or make an appointment with a general practitioner or therapist. Children are advised to visit a pediatrician.
Since lymphocytosis is not a separate disease, but a symptom of disorders, the doctor collects anamnesis and suggests undergoing a comprehensive diagnosis. It includes:
- Blood analysis. He determines the leukocyte formula to identify the ratio of all types of leukocytes, determine the indicators of ESR, CRP. The biomaterial is examined for the presence of atypical mononuclear cells. If cancer of the hematopoietic system is suspected, diagnostics are performed to identify tumor antigens.
- Special studies to identify the pathogen. To normalize blood counts during an infectious disease, you need to know the exact cause of lymphocytosis. To do this, the doctor collects anamnesis and, taking into account the existing symptoms, prescribes examinations. The PRC method is used to detect antibodies to viruses. If tuberculosis and whooping cough are suspected, a microbiological examination of sputum is performed. Serological diagnosis helps identify brucellosis.
- Hardware and instrumental diagnostics. Patients with lymphocytosis are prescribed hardware and instrumental studies. If tuberculosis is suspected, an x-ray of the lungs is required, which will show the lesions and help assess its extent. For mononucleosis and hematological malignancies, an abdominal ultrasound is prescribed. Patients with this disease exhibit pathological enlargement of the spleen and, in some cases, the liver.
- Histology. For leukemia, lymphomas and other dangerous pathologies, patients require a histological examination of the bone marrow. It will show the presence of altered blood cells and help assess the type of pathology. A puncture is performed to obtain biomaterial.
Lymphocytosis
Lymphocytosis, defined by an increase in the absolute lymphocyte count (ALC) to more than 4000 lymphocytes/μL in adult patients, is a common hematologic abnormality. ALC is calculated as the total white blood cell count (WBC) multiplied by the percentage of lymphocytes in the peripheral blood. Different subsets of lymphocytes (T cells, B cells, or NK cells) may be increased depending on the specific etiology. Lymphocytes make up about 20-40% of WBC. The definition of relative lymphocytosis is an increase in WBC of more than 40% in the presence of a normal absolute white blood cell count.
Distinguishing reactive from malignant lymphocytosis can be difficult because it varies by age and other demographics. The following is a list of the most common causes of reactive lymphocytosis:
Infectious:
- Viral infections:
- Epstein-Barr virus (EBV): Infectious mononucleosis (IM) is a classic example of viral infections associated with lymphocytosis. Acute IM is a disease characterized by fever, lymphadenopathy, pharyngitis, splenomegaly and various hematological manifestations, of which lymphocytosis is the most common, occurring in two-thirds of cases.
- Cytomegalovirus (CMV): CMV can cause illness indistinguishable from EBV-IM.
- Human immunodeficiency virus (HIV): Although chronic HIV infection results in lymphopenia and decreased CD4+ lymphocyte counts, primary HIV infection can lead to acute febrile mononucleosis-like illness with associated lymphocytosis. A negative heterophil test can help differentiate the two conditions.
- Other viruses: influenza, hepatitis, mumps, measles, rubella and human T-lymphocyte virus type 1 (HTLV-1), adenovirus, and many others.
2. Bacterial infections: Most acute bacterial infections cause neutrophilia; However, notable exceptions include:
- Bartonella henselae: Bartonella henselae causes cat scratch disease, a disease transmitted by a scratch or bite from an infected cat that primarily results in self-limited lymphadenopathy, but may be associated with ocular or neurological manifestations. Lymphocytes are large and atypical.
- Bordetella Pertussis: Pertussis is characterized by altered lymphocytes that are small with a deeply cleaved nucleus, clinical correlation is necessary to differentiate from some lymphoid malignancies that may have a similar morphological appearance.
- Other: Brucellosis, syphilis, malaria
3. Parasitic Infections: Toxoplasma gondii: Symptomatic toxoplasmosis most often occurs in immunocompromised people. Lymphocytosis with atypical lymphocytes is a hematologic feature of the disease that may present as a mononucleosis-like disease. 4. Mycobacterial tuberculosis Lymphoproliferative disorders. Lymphocytes tend to be monomorphic for malignant reasons, which is in contrast to lymphocytes being pleomorphic for reactive reasons. Some common etiologies are listed here:
Hypersensitivity reactions to drugs. Some drugs, such as allopurinol, carbamazepine, vancomycin, and sulfa drugs, may be correlated with drug reactions with eosinophilia and systemic symptoms (DRESS), and this may be associated with lymphocytosis. A relatively new CLL drug, the bruton tyrosine kinase (BTK) inhibitor ibrutinib, has shown impressive results. However, it is correlated with worsening lymphocytosis after treatment initiation. Its effect likely represents a redistribution of CLL cells from lymphoid tissues to the peripheral blood and does not indicate a negative response to therapy. Monoclonal B lymphocytosis (MBL): This refers to the presence of monoclonal B cells at a level of less than 5000 cells/μL in the absence of evidence of lymphoproliferative disorders, splenomegaly, or cytopenia. These B cells most often have the same phenotype as CLL (CLL-like); however, their phenotype may be different (atypical MBL). Congenital B-cell lymphocytosis: This is due to a heterozygous germline missense mutation in CARD11, a scaffolding protein required for nuclear factor kappa B (NF-KB) in both B and T lymphocytes. It usually progresses to CLL by the 4th decade of life. Persistent B-cell polyclonal B-lymphocytosis. It is a rare clinical entity described as polyclonal binucleate lymphocytes occurring predominantly in young female smokers. Unlike CLL or MBL, lymphocytes are polyclonal with expression of both kappa and lambda chains. It is associated with a polyclonal gammopathy of HLA DR-7 and IgM and shows a stable clinical and biological course. Stress: Severe and urgent health conditions may correlate with transient lymphocytosis that precedes neutrophilia. Most patients here are diagnosed with heart disease, epileptic conditions or adrenaline use. Asplenia: Similar to other blood components, lymphocyte counts may increase postsplenectomy but usually remain stable over many years. Epidemiology of EBV: EBV infection is widespread throughout the world among all age groups, and about 90% of adults will eventually become seropositive. IM, although traditionally peaks in young people between the ages of 15 and 24, can occur later in life. Symptomatic clinical infection is much more common Whooping cough and cat scratch disease: Whooping cough mainly affects children under ten years of age, but can occur in adults, where it may herald a more severe course in older people. Cat scratch disease is also more common in children and young adults CLL is the most common leukemia in adult patients, especially in older adults with an average age of diagnosis of 70 years. This disease is more common in men (male to female ratio is about 1.5:1) The incidence of peripheral blood lymphocytosis varies depending on the type of lymphoma and ranges from 20 to 80% MBL: the prevalence of MBL is very high compared to CLL and reaches 5–9 % among the population over 60 years of age. MBL is also more common in men than women Drug reaction with eosinophilia and systemic symptoms (DRESS). Lymphocytosis in DRESS can occur in approximately 30-70% of cases. Pathogenesis Increased lymphocyte production may be caused by a clonal or reactive process. Additionally, redistribution of lymphoid cells may be the primary etiology in some patients with lymphocytosis. The mechanism of some of the most common causes is as follows: EBV: In the early stages of IM, EBV infects resting B cells, and large numbers of infected B cells circulate in the blood. However, atypical lymphocytes are activated cytotoxic CD8+ cells that appear 1–3 weeks after symptom onset. In patients infected with EBV, memory B cells become latently infected and lead to chronic infection with possible reactivation and predisposition to lymphoproliferative disorders. Atypical large lymphocytes are seen in EBV and other viral infections such as CMV or early HIV. Treatment is usually supportive: analgesics and/or non-steroidal anti-inflammatory drugs. Because most patients have splenomegaly, they should be instructed to avoid contact sports in the early acute stage to avoid splenic rupture. The use of corticosteroids is controversial, and current literature does not provide sufficient evidence to support its use for symptomatic relief. However, EBV-infected latent B cells may lead to the development of EBV-associated lymphoproliferative disorders, including post-transplant lymphoproliferative disorder (PTLD), Hodgkin's lymphoma (HL), and non-Hodgkin's lymphoma in immunocompromised individuals. Pertussis: The mechanism of lymphocytosis in pertussis may be due to decreased extravasation of lymphocytes from peripheral blood into lymphoid organs and/or expansion of morphologically normal CD4+ T cells. Antibiotics (such as azithromycin or clarithromycin) are usually prescribed to adult patients when a cough appears within three weeks of the onset of cough. Congenital B-cell lymphocytosis is associated with mutations in CARD11, a scaffolding protein required for nuclear factor kappa B (NF-KB) in both B and T lymphocytes.
Treatment of lymphocytosis
If the increase in the number of lymphocytes is caused by physiological reasons, no treatment is required. A pathological change in the leukocyte formula of the blood, which is accompanied by prolonged lymphocytosis, requires attention from a doctor.
There are no special drugs or techniques to normalize the lymphocyte count. The doctor’s task is to identify the cause of the pathology and eliminate it. Conservative and surgical methods can be used for treatment. For example, for chickenpox, rubella, ARVI and influenza, symptomatic therapy is prescribed: antipyretic and anti-inflammatory drugs. The patient is advised to drink plenty of fluids and gargle. Antiviral drugs are effective in the first days when flu symptoms appear.
Bacterial infections are treated with antibiotics. Lymphocytosis in tuberculosis can be eliminated if you undergo a course of treatment with drugs chosen by your doctor.
Long-term and complex therapy is required for high lymphocytosis in patients with leukemia and other diseases of the hematopoietic system. First of all, chemotherapy is prescribed, which is carried out in courses. If it does not lead to improvement, a bone marrow transplant is recommended.
Correction
There are no direct ways to normalize the concentration of lymphocytes. To combat lymphocytosis, it is necessary to treat the underlying pathology that caused the increase in lymphocytes. Minor short-term lymphocytosis that occurs due to stress, taking medications, or during recovery from a cold does not require therapy. In case of long-term lymphocytosis, both absolute and relative, you should consult a doctor.
For many viral infections (varicella, rubella, ARVI), no etiotropic therapy has been developed to date. For their treatment, pathogenetic and symptomatic methods are used - plenty of hot drinks, antipyretic, anti-inflammatory drugs. For catarrhal syndrome, gargling and irrigating the throat with antiseptic solutions and sprays are prescribed. In the first days of influenza, the use of antiviral drugs (oseltamivir, rimantadine) is effective.
There is evidence of a reduction in the number of complications of infectious mononucleosis in adults by prescribing acyclovir and valciclovir. For bacterial infections, antibiotics are prescribed, for tuberculosis, a combination of anti-tuberculosis drugs. If the cause of lymphocytosis is a lymphoproliferative disease, then long repeated courses of chemotherapy are required. If conservative treatment of chronic myeloid leukemia in adults is ineffective, allogeneic bone marrow transplantation is used.