- Types and causes of placental insufficiency
- Diagnosis of placental insufficiency
- Treatment of placental insufficiency
Most women know that the placenta connects mother and baby during pregnancy and through it, nutrients and oxygen are supplied to the baby.
Are there situations when the placenta stops performing its function correctly and fully? Is it possible to somehow prevent this?
What is the function of the placenta?
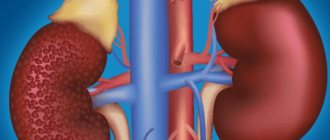
So, the placenta is an important organ that is formed only during pregnancy. The placenta is formed from the chorion - the embryonic membranes of the fetus. At the very beginning of pregnancy, chorionic villi - outgrowths of the membrane - evenly cover the entire surface of the fetal egg; starting from the second month of pregnancy, on one side of the fetal egg, the villi begin to lengthen, increase in size and form the placenta.
The baby's blood flows inside the villi, and outside they are washed with the mother's blood. Between the bloodstream of mother and baby there is only one layer of cells, which acts as a barrier between the body of mother and child. Thanks to this membrane, the blood of the mother and fetus does not mix.
However, in recent years it has become known that fetal blood cells do penetrate the placental barrier into the mother’s bloodstream, and thanks to this, it has become possible to conduct genetic tests and determine chromosomal abnormalities, Rh factor and fetal sex using the blood of a pregnant woman (non-invasive prenatal test).
In the placenta there is a constant exchange of substances between mother and child. Oxygen and nutrients flow from the mother's blood to the fetus, and carbon dioxide and metabolic products that must be excreted from the body return to the mother from the fetus.
The placental barrier performs an immunological function, since it allows the passage of some protective antibodies - blood cells that ensure the fight against infectious agents; in addition, it is impermeable to some harmful substances, viruses and bacteria. Unfortunately, the placental barrier is easily overcome by drugs, alcohol, nicotine, components of many medications and some viruses.
An important function of the placenta is the production of hormones and biologically active substances. First of all, these are hormones that are important for successful pregnancy, for example, human chorionic gonadotropin, placental lactogen, estrogens, etc.
Unfortunately, things don’t always work out quite well. For a variety of reasons, at different stages of pregnancy, deviations in the development and functioning of the placenta can occur. These changes never go unnoticed for mother and baby, and often have dire consequences.
If the placenta ceases to perform its functions fully, so-called placental insufficiency develops. In essence, it consists in deterioration of blood circulation in the mother-placenta-fetus system.
Types and causes of placental insufficiency
Doctors distinguish between acute and chronic placental insufficiency:
Acute placental insufficiency
This is a condition that requires emergency medical intervention. It is characterized by a rapid deterioration of placental blood flow. Acute placental insufficiency occurs mainly as a result of placental abruption or death of individual areas of placental tissue, for example, due to the formation of blood clots in blood vessels. The cause of detachment may be abdominal trauma or antiphospholipid syndrome.
Phospholipids are complex fats that are part of the membranes of all cells in the body. In some cases, the body's immune system produces large amounts of antibodies to some of its own phospholipids and proteins that bind these lipids. They are called antiphospholipid antibodies and when interacting with the cells of the body, they cause cell damage and activation of the blood coagulation system, which leads to blood clots.
Antiphospholipid syndrome is the most common cause of thrombotic complications during pregnancy, including placental abruption and acute placental insufficiency. Placental abruption can also be caused by severe gestosis, a dangerous complication of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine.
Acute placental insufficiency develops when more than 2/3 of the surface of the placenta is detached.
If acute placental insufficiency develops, it is necessary to perform a cesarean section as quickly as possible to save the life of the baby and mother.
Chronic placental insufficiency
Chronic placental insufficiency occurs much more often in pregnant women. In this case, the formation and maturation of the placenta is disrupted, uteroplacental and fetal-placental blood flows are reduced, gas exchange and metabolism in the placenta is limited, and the synthesis of placental hormones is reduced. All these changes determine the insufficient supply of oxygen and nutrients to the baby and cause retarded growth and development of the fetus.
The causes of placental insufficiency most often are previous abortions, especially surgical abortion during the first pregnancy, smoking, while the number and strength of cigarettes smoked do not matter, since tobacco smoke, not nicotine, has a negative effect on the formation of defective blood vessels of the placenta.
The risk group for the development of placental insufficiency also includes women with chronic diseases, such as arterial hypertension, iron deficiency anemia, pyelonephritis, diabetes mellitus, and thyroid diseases. In recent years, there has been a significant increase in placental insufficiency caused by bacteria, viruses, and fungi. The reason for this may be either an acute infection suffered by the expectant mother during pregnancy or the activation of a chronic infectious process in the body of a pregnant woman.
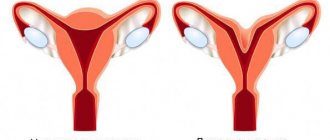
Uterine pathology plays an important role in the formation of chronic placental insufficiency: endometriosis, uterine malformations (saddle-shaped, bicornuate). Doctors also consider uterine fibroids to be a risk factor. Of course, a number of medications have an adverse effect on the formation of the placenta and fetal development. Currently, a list of drugs that are not approved for use during pregnancy has been determined.
Also of great importance in the development of placental insufficiency is thrombophilia - an increased tendency of the body to form blood clots - thrombi in the vessels.
In some cases, placental insufficiency may be due to the presence of chromosomal abnormalities in the fetus, in particular with Down syndrome (the presence of an additional 21st chromosome in the fetus) or Edwards syndrome (an additional 18th chromosome in the fetus), a dysfunction of the placenta is diagnosed already in the early stages of pregnancy.
It should be noted that among the pregnancy complications that most often lead to the development of chronic placental insufficiency, a significant factor is preeclampsia (or late gestosis) - these are complications of the second half of pregnancy, manifested by edema, increased pressure and the appearance of protein in the urine. Regardless of the factors contributing to the development of placental insufficiency, it is based on circulatory disorders in the uteroplacental complex, leading to disruption of all functions of the placenta. Consequently, symptoms of chronic placental insufficiency will be caused by a lack of oxygen and nutrients to the fetus.
This is, first of all, intrauterine growth retardation - a lag in the size of the fetus and a slowdown in its growth rate. There are often changes in fetal motor activity. At first there may be some increase in movements, and then a decrease. Violation of the protective function of the placenta leads to intrauterine infection of the fetus under the influence of pathogenic (disease-causing) microorganisms penetrating the placenta. The fetus, whose development occurs under conditions of placental insufficiency, is at a much greater risk of trauma during childbirth; they have impaired adaptation to extrauterine life and increased morbidity in the first year of life.
Based on the time of occurrence, doctors divide placental insufficiency into early and late.
Early (or primary) placental insufficiency
Develops before 16 weeks of pregnancy. It occurs already at the stage of placenta formation and is associated with diseases of a pregnant woman that existed before pregnancy, for example, pathology of the uterus, chronic arterial hypertension, and endocrinological diseases. In this case, the formation of defective vessels in the placenta occurs.
Late (or secondary) placental insufficiency
Occurs after 16 weeks of pregnancy and is most often associated with diseases that arose during pregnancy. Most often, these are iron deficiency anemia (that is, a decrease in the concentration of hemoglobin and iron in the blood), gestational diabetes mellitus (that is, a violation of the body's absorption of glucose that occurs during pregnancy), and previous viral and bacterial infections.
It is important to divide placental insufficiency into compensated and decompensated forms.
Compensated placental insufficiency
It develops, for example, when there is a threat of miscarriage and mild forms of late gestosis, if these complications can be successfully corrected with medication.
Decompensated placental insufficiency
Causes development of delayed fetal development, chronic intrauterine hypoxia, up to fetal death.
Diagnosis of placental insufficiency
It is almost impossible to treat already developed placental insufficiency, so doctors are actively seeking to identify pregnant women at risk of developing placental dysfunction. If placental insufficiency is detected in the 3rd trimester of pregnancy, unfortunately, there is no effective treatment. Therefore, all methods of identifying in the early stages of pregnancy those women whose placenta formation has undergone disturbances are being very actively used.
First of all, when registering for pregnancy, the most significant risk factors are identified - smoking, previous abortions, family history (low birth weight, tendency to thrombosis), the presence of chronic heart disease, vascular disease, diabetes mellitus.
Preventive measures against the development of placental insufficiency are especially relevant and necessary until 16-17 weeks of pregnancy, when the formation of placental structures occurs.
Prenatal screening, which is carried out at 11-14 weeks of pregnancy, provides significant assistance in assessing the risk of developing placental insufficiency. It is carried out to identify Down syndrome, Edwards syndrome and other chromosomal diseases in the fetus. Currently, the most urgent thing is to conduct comprehensive early screening of pregnant women to predict the risk of developing placental insufficiency, preeclampsia and intrauterine growth retardation. Since this type of diagnostics is one of the most modern and advanced, unfortunately, it is not yet included in the list of services provided in the antenatal clinic as part of compulsory medical insurance, but is available to everyone at prenatal diagnostic centers.
Determination of proteins produced by the placenta
First of all, the PAPP-A protein is determined; it is also a marker of fetal chromosomal abnormalities. A decrease in the concentration of PAPP-A in the blood at 11-14 weeks of pregnancy occurs in pregnant women who have a high risk of placental insufficiency and fetal growth retardation.
The second placental hormone that helps in assessing the risk of placental insufficiency is PIGF (placental growth factor). Its concentration in the blood decreases long before the first manifestations of placental insufficiency. Its definition is not used as widely as PAPP-A, but nevertheless, many laboratories have already included this protein in prenatal screening of the 1st trimester. Measuring blood flow in the vessels of the uterus is extremely important when conducting 1st trimester screening. It has been unequivocally proven that the narrowing of the vessels of the uterus, determined during the study, indicates the inferiority of the formation of the placenta, which will worsen with increasing gestational age and will lead to a decrease in the baby’s nutrition and oxygen supply, that is, to the development of placental insufficiency and delayed fetal development. With normal sizes of the uterine vessels at 11-14 weeks of pregnancy, the risk of severe placental insufficiency is negligible.
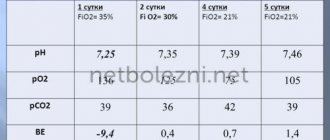
The next mandatory screening ultrasound examination is carried out at 20-21 weeks of pregnancy. In this case, it is necessary to take measurements of the fetus to assess whether there is growth retardation. Indeed, with oxygen starvation, the growth rate of the fetus slows down and its size begins to lag behind the norm for each stage of pregnancy. In addition, the doctor must evaluate the condition and maturity of the placenta. During ultrasound, Doppler measurements of the uterine vessels are also performed to identify early changes that precede the clinical manifestations of placental insufficiency.
In patients belonging to the high-risk group, in addition to ultrasound and Doppler measurements, daily monitoring of blood pressure fluctuations is also carried out, determination of the amount of protein in a urine test collected per day, and evaluation of blood coagulation system parameters.
The third ultrasound is performed for all expectant mothers at 30–34 weeks of pregnancy. The doctor measures the circumference of the baby's head and abdomen, the length of the bones of his arms and legs, and calculates the estimated weight of the fetus. These measurements allow the doctor to make sure that the baby is developing normally. Also important is the structure of the placenta, the presence of signs of aging in it, as a result of which it usually ceases to fully supply the baby with blood, which means that he ceases to have enough oxygen and nutrients and the child’s development is disrupted. During an ultrasound, the amount and type of amniotic fluid is assessed, which can also change with intrauterine fetal suffering.
Doppler
Doppler testing of the vessels of the placenta and umbilical cord (a method for studying the speed of blood flow in these vessels) also allows you to assess the baby’s well-being. The doctor examines the blood flow in the arteries of the uterus, umbilical cord, heart and brain of the child. This study allows you to determine whether the placenta is working well, whether there are signs of a lack of oxygen in the baby, or the development of gestosis in the mother. When the speed of blood flow in any vessel decreases, we can talk about fetal nutritional disorders of varying degrees of severity.
A timely examination allows us to identify the initial stages of blood supply deficiency. In such cases, treatment can prevent serious complications, such as hypoxia and intrauterine growth retardation. Dopperometry is carried out at 20–21 weeks and at 30–32 weeks of pregnancy; if there are changes, monitoring is carried out at least every two weeks.
Cardiotocography
This is an important method for assessing the condition of the fetus. CTG is performed during pregnancy of 33 weeks or more, since only at this stage of the baby’s intrauterine development is full regulation of the activity of the fetal cardiovascular system established by the centers of the spinal cord and brain. The fetal heartbeat is recorded for 20–40 minutes, and if necessary, the study can be extended to 1.5 hours.
The device detects and records the baby's heart rate. The obstetrician-gynecologist evaluates the heartbeat recording curve, episodes of decrease and sharp increase in the fetal heart rate and, based on these data, makes a conclusion about how comfortable the baby feels in the mother’s stomach. For example, when the concentration of oxygen in the blood of the fetus decreases, its supply to the cells of the nervous system also decreases, which in turn affects the heart rate. In the normal course of pregnancy, CTG is performed after 33 weeks once every 10–14 days, sometimes more often. Some clinics currently offer the service of continuous CTG monitoring, which becomes relevant if there are signs of placental insufficiency. A pregnant woman is given a monitor that records changes in the baby’s cardiac activity and this data is transmitted via the Internet to the attending physician.
Therapy
There is no universal treatment regimen. This is due to the fact that pathology has many forms and types and can develop due to a variety of factors. Therefore, doctors in most cases send the expectant mother to the hospital to monitor the intensity of FPN and take correct measures.
Under no circumstances should you prescribe treatment on your own! At the first signs of malaise, a decrease in the number of movements, or bleeding, you should immediately consult a doctor.
Treatment of placental insufficiency
There are currently no specific treatments for placental insufficiency, since there are no drugs that selectively improve uteroplacental blood flow. That is why all measures to combat placental insufficiency are aimed at prevention. If the patient is at high risk for the development of placental insufficiency, from early pregnancy she is prescribed medications whose effectiveness is well proven and which prevent the early development of severe placental dysfunction.
If, during additional methods of assessing the condition of the fetus, initial disturbances in the supply of oxygen to the baby are detected, drug treatment is carried out aimed at increasing the flow of blood and oxygen through the placenta and mandatory control examinations during the therapy. If the changes are serious and the baby experiences a severe deficiency of oxygen and nutrients, his condition suffers, then in such cases an emergency delivery is performed.
Symptoms
There are no identical and exact signs of FPN. It all depends on the form of the pathology. Naturally, in case of acute insufficiency, the symptoms cannot be ignored: the woman’s well-being changes, bleeding begins, and the child suddenly calms down and stops moving.
The chronic form proceeds calmly, only slight bleeding is possible periodically, and the size of the abdomen does not correspond to the norm for the duration of pregnancy.
That is why a woman must attend all prescribed ultrasounds and screenings. It is with the help of these procedures that the doctor can assess the functionality and condition of the placenta.