Hypotrophy in children
Chronic eating disorders can be caused by various factors acting in the prenatal or postnatal period.
Intrauterine malnutrition in children is associated with unfavorable conditions that disrupt the normal development of the fetus. In the prenatal period, malnutrition of the fetus and newborn can be caused by pregnancy pathology (toxicosis, gestosis, fetoplacental insufficiency, premature birth), somatic diseases of the pregnant woman (diabetes mellitus, nephropathies, pyelonephritis, heart defects, hypertension, etc.), nervous stress, bad habits, undernutrition of women, industrial and environmental hazards, intrauterine infection and fetal hypoxia.
Extrauterine malnutrition in young children can be caused by endogenous and exogenous causes. Endogenous causes include chromosomal abnormalities and congenital malformations, fermentopathies (celiac disease, disaccharidase lactase deficiency, malabsorption syndrome, etc.), immunodeficiency conditions, constitutional abnormalities (diathesis).
Exogenous factors leading to malnutrition in children are divided into nutritional, infectious and social. Nutritional influences are associated with protein-energy deficiency due to insufficient or unbalanced nutrition. Hypotrophy in a child may be a consequence of constant underfeeding associated with difficulty sucking when the mother’s nipples are of an irregular shape (flat or inverted nipples), hypogalactia, insufficient amount of formula, excessive regurgitation, qualitatively inadequate nutrition (deficiency of microelements), poor nutrition of a nursing mother, etc. This group of reasons includes diseases of the newborn itself that do not allow him to actively suck and receive the required amount of food: cleft lip and palate (cleft lip, cleft palate), congenital heart defects, birth injuries, perinatal encephalopathy, pyloric stenosis, cerebral palsy, alcoholic fetal syndrome, etc.
Children who suffer from frequent acute respiratory viral infections, intestinal infections, pneumonia, tuberculosis, etc. are prone to the development of acquired malnutrition. An important role in the occurrence of malnutrition in children belongs to unfavorable sanitary and hygienic conditions - poor child care, insufficient exposure to fresh air, rare bathing, insufficient sleep .
Publications in the media
Hypotrophy is a type of dystrophy, a chronic disorder of nutrition and tissue trophism, characterized by a relative decrease in the child’s body weight in relation to its length, disrupting the proper development and functions of individual organs and systems. Based on the time of occurrence, prenatal, postnatal and mixed malnutrition are distinguished. Frequency. In 3–5% of cases, a pediatrician is consulted about insufficient weight gain.
Etiology. Hypotrophy is a polyetiological syndrome; may accompany various diseases.
• Exogenous causes •• Nutritional (underfeeding, overfeeding, imbalance of nutrients) •• Infectious (acute infections, sepsis) •• Toxic (poisoning, burns, use of cytostatics) •• Social factors (defects in education, low social level of the family, etc. .P.).
• Endogenous causes •• Endocrine and neuroendocrine disorders - anomalies of the thymus gland, hypothyroidism, adrenogenital syndrome, pituitary dwarfism •• Malformations of organs •• Hereditary enzymopathies ••• Malabsorption in the intestine (celiac disease, disaccharidase deficiency, malabsorption syndrome) ••• Impairment breakdown of nutrients (cystic fibrosis) •• Primary metabolic disorders (protein, carbohydrate, fat metabolism).
Genetic aspects. Hypotrophy is a manifestation of many genetic diseases; for example, malnutrition is accompanied by almost all chromosomal diseases, dozens of mendelian syndromes, especially malabsorption syndromes (cystic fibrosis, celiac disease, lactase deficiency, etc.).
Clinical picture.
• Degrees of hypotrophy •• First degree hypotrophy ••• Body weight deficiency - 10–20% ••• The child’s condition is satisfactory ••• On examination - a slight decrease in the amount of subcutaneous fatty tissue on the abdomen •• Second degree hypotrophy ••• Body weight deficiency - 20–30%, possible growth retardation of 2–4 cm ••• The general condition suffers slightly ••• Lability of the nervous system (excitement, apathy, lethargy, decreased emotional tone) ••• Paleness, dryness and peeling of the skin, decreased elasticity of the skin and turgor of soft tissues ••• Subcutaneous fatty tissue is preserved only on the face ••• Signs of microcirculation disorders (marbling of the skin, decreased body temperature) ••• Dyspeptic disorders (nausea, vomiting, constipation) ••• Possible breathing problems ( tachypnea), cardiac activity (muffled heart sounds, arterial hypotension, tendency to tachycardia) ••• Possible delay in psychomotor development ••• Anemia is often detected •• III degree hypotrophy ••• Body weight deficiency - more than 30%, severe developmental delay ••• The general condition is severe, lethargy, weakness, anorexia, loss of acquired skills ••• The skin is dry, pale, with a grayish tint, hanging in folds ••• Complete absence of subcutaneous fatty tissue, muscle atrophy ••• Possible signs of dehydration - dry mucous membranes membranes, retraction of the large fontanel, shallow breathing, arterial hypotension, muffled heart sounds, impaired thermoregulation, severe thirst ••• Voltaire's face (triangular in shape) ••• Height deficiency reaches 4–6 cm.
• Prenatal malnutrition. Intrauterine growth retardation can be included in this group of malnutrition. Based on the severity of intrauterine hypoxic damage to the brain and clinical manifestations, the following forms are distinguished •• Neuropathic - characterized by a slight decrease in body weight, impaired appetite and sleep of the child •• Neurodystrophic - decrease in body weight and length, retardation in psychomotor development, persistent anorexia •• Neuroendocrine - disorder endocrine regulation of psychomotor development, functional state of organs •• Encephalopathic - severe retardation in physical and mental development, severe neurological deficit, hypoplasia of the skeletal system, polyhypovitaminosis.
Diagnostics • Life history (obstetric and postnatal) - course of pregnancy, toxicosis, maternal illness; course of labor, duration of the anhydrous interval, use of obstetric aids; monthly weight gain of the child, illnesses suffered in the early neonatal period • Social anamnesis (housing and living conditions, socio-economic condition of the family) • Hereditary anamnesis - metabolic, endocrine diseases, enzymopathies in family members • Examination - anthropometric data, condition of the skin and subcutaneous tissue fiber, physical data • Body weight deficiency (in percent) is determined by the following formula.
where DM is the required mass taking into account growth; FM - actual mass. To assess malnutrition, you can use tables of centile distributions of mass along body length (Mazurin A.V., Vorontsov I.M., 1985)
Laboratory tests • CBC - hypochromic anemia, increased Ht due to increased blood viscosity, increased ESR, possible leukopenia, thrombocytopenia • General and biochemical urine tests • Biochemical blood test • Study of acid-rich hormone, electrolyte content (potassium, calcium, sodium) • Immunogram (for infectious processes) • Coprogram • Feces for dysbacteriosis • Endocrine profile (according to indications) - study of the functions of the thyroid gland, adrenal glands, determination of the concentration of glucose in the blood • Study of sweat chlorides for suspected cystic fibrosis • Bacteriological and virological studies for suspected intrauterine infections and infectious processes • Consultations with a neurologist, endocrinologist, ophthalmologist.
Drugs that affect results. The use of antibiotics causes or aggravates intestinal dysbiosis, indirectly affecting intestinal absorption.
Special research methods • X-ray examination of the chest to exclude a specific pulmonary process (for cystic fibrosis, tuberculosis) • X-ray of the hands to determine bone age • X-ray of the skull bones (sella turcica condition) • ECG to exclude congenital heart disease.
TREATMENT
Mode • Outpatient for grades I and II with satisfactory tolerance to food loads • Hospitalization is required in the following situations •• Age up to 1 year •• Presence of concomitant pathology of internal organs and/or infectious diseases •• Stage II malnutrition with low tolerance to food loads •• III stage of malnutrition • Therapeutic exercises and massage.
Medical nutrition
• The first phase is the adaptation period. The goal is to determine and increase the child’s tolerance to food products •• Restoration of water-salt metabolism •• Food loads are reduced compared to the norm ••• Up to 2/3 of the required volume of food for malnutrition of the first degree ••• Up to 1/2–1/ 3 required volumes of food for malnutrition of II–III degrees ••• Or 100 ml of breast milk per 1 kg of actual body weight for I–II degrees •• Parenteral nutrition for II degree is 1/3 of the volume of food received; in grade III - from 1/2 to 2/3, depending on the severity of the child’s condition. The composition of the injected liquid is colloids and crystalloids in a 1:1 ratio.
• 2nd phase - reparation period. The goal is to restore all types of metabolism and transition to complete intestinal nutrition. The diet is calculated based on energy costs - 150–180 kcal/kg of actual weight, depending on the severity of malnutrition. Gradual introduction of all food and vitamin supplements in age proportions.
• 3rd phase - enhanced nutrition. The goal is to restore the supply of nutrients in terms of age-appropriate body weight.
Drug therapy • Ascorbic acid, thiamine, pyridoxine, cyanocobalamin, retinol, vitamin E, folic acid, calcium pantothenate are widely used. Enzyme preparations: pancreatin, panzinorm forte, pancreatin + bile components + hemicellulase • To increase appetite and stimulate anabolic processes - royal jelly (newborns - 2.5 mg, children over 1 month - 5 mg in the form of suppositories 3 times / day for 7–15 days; contraindicated in Addison’s disease and idiosyncrasy to the drug), bitterness, orotic acid, potassium salt (10 mg/kg/day in 2–3 doses for 3–5 weeks), carnitine chloride (4–5 weeks) 10 drops of 20% solution 3 times a day), calcium glycerophosphate 0.05–0.2 g 2–3 times a day • Anabolic steroids (under the control of bone age) - nandrolone, methandienone • Parenteral nutrition drugs + levocarnitine • For concomitant allergic processes - antihistamines • For intestinal dysbiosis - colibacterin, bificol, lactobacterin, bifidumbacterin • For prenatal dystrophy - sedatives, cerebrolysin, glutamic acid • Hormonal drugs (thyroidin, insulin) - if necessary • Treatment of concomitant pathologies and infectious complications.
Course and prognosis. With timely and rational treatment, including nutrition and drug therapy, the prognosis is favorable. The course of malnutrition is complicated by the lack of child care in asocial families, concomitant pathologies and infectious diseases. In the case of prenatal malnutrition, the prognosis depends on the degree of hypoxic brain damage.
Prevention • Strengthening the health of women before and during pregnancy. • Rational feeding and balanced nutrition • Organizing the correct regimen • Careful child care • Physical education and hardening • Monitoring body weight gain • Carrying out nutrition calculations and timely correction.
Note. In recent years, prenatal malnutrition has been considered as a manifestation of intrauterine growth retardation (IUGR), that is, as a hypotrophic variant of IUGR.
Reduction. IUGR—intrauterine growth retardation.
ICD-10 • P05 Fetal growth retardation and malnutrition • P07 Disorders associated with shortened gestational age and low birth weight, not elsewhere classified
Signs
There are several stages of muscle wasting:
- The amount of subcutaneous tissue throughout the body decreases. A person loses up to 20% of body weight. He has pallor, weak appetite, muscle tone decreases;
- Subcutaneous tissue on the abdomen and chest practically disappears. The skin becomes gray, the muscles become flabby, and the liver increases in size. Mental health disorders and irritability occur;
- Severe wasting (cachexia) occurs when the patient loses 30% of muscle mass. The condition requires intensive therapy.
Common symptoms of muscle wasting include the following:
- Constant muscle pain;
- Weakness;
- Inability to perform normal movements;
- Significant loss of body weight.
If areas of muscle wasting are located symmetrically, this raises suspicion of myopathy or spinal amyotrophy. With progressive muscular dystrophy, relatively isolated wasting of the quadriceps femoris or biceps brachii is observed. If malnutrition is located in the distal limbs, we are talking about polyneuropathy (with impaired sensitivity and loss of reflexes in the distal limbs) or Steinert’s myotonic dystrophy.
Unilateral acquired isolated muscle wasting is always a consequence of damage to the root, plexus or peripheral nerve. Decisive for the topical diagnosis is the characteristic distribution of the process of malnutrition and sensory disturbances or prolonged inactivity of the muscle. Hypotrophy of the quadriceps muscle occurs with arthrosis of the knee joint and with sarcoma of the hip. Focal wasting of individual muscles or muscle groups, isolated and sometimes symmetrical, can slowly progress over many years. This is a sign of focal damage to the ganglion cells of the anterior horns or ischemia in the area of the blood supply of the artery.
Hypotrophy of the calf muscles often occurs. With progressive muscular dystrophy, sometimes in significantly hypotrophied muscles areas with intact muscle fibers are identified, which look like nodules. Doctors at the Yusupov Hospital distinguish them from a muscle roll, which is formed when the short head of the biceps brachii muscle is ruptured and is noticeable on the flexor surface of the shoulder.
Symptoms of malnutrition
The clinical picture of malnutrition is represented by the following signs:
- Trophic disorders:
- weight loss;
- violation of body proportionality;
- changes in the skin: decreased elasticity, dryness, peeling, pale skin; symptoms of hypovitaminosis are also determined (brittle nails, hair loss, seizures, etc.);
- thinning of the subcutaneous fat layer on the abdomen, torso, limbs, and in severe malnutrition - on the child’s face.
- Changes from the central nervous system:
- tearfulness, irritability or vice versa, lethargy, apathy;
- sleep disturbance;
- delayed neuropsychic development;
- muscle weakness;
- thermoregulation disorder.
- Reduced food tolerance:
- loss of appetite, in some cases complete refusal of food is possible;
- manifestations of dyspepsia: nausea, vomiting, bowel dysfunction (constipation or diarrhea).
- Reduced immunological reactivity. Children with this pathology are often susceptible to infectious diseases, have a tendency to protracted inflammatory processes, and may develop atypical variants of the course of diseases and septic conditions.
It is worth noting that the severity of symptoms may vary depending on the stage of malnutrition. If you find the listed signs in a child, you should immediately seek help from a pediatrician for timely diagnosis and treatment of the disease.
Treatment options
Treatment of malnutrition in children begins with the selection of adequate diet therapy. The diet is selected in two stages:
- find out if there is any food intolerance;
- Calculate nutrition for a child with malnutrition.
The calculation is carried out based on the baby’s body weight, his height and the severity of the disease. Meals should be fractional, if necessary, portions are adjusted up or down, so doctor’s supervision over the progress of treatment is necessary.
Diet therapy is accompanied by drug treatment based on the selection of enzymes, vitamins, and hormonal anabolic drugs, if necessary.
Consequences of malnutrition
With timely seeking medical help and adequate therapy, the prognosis is favorable, however, if the main symptoms of the disease are ignored for a long time, the child may develop the following complications:
- impairment of mental and physical development;
- deficiency conditions (rickets, anemia, etc.);
- prolonged colds, more severe course of various inflammatory diseases (pneumonia, otitis media, enterocolitis, etc.).
With third degree malnutrition, even with treatment, the mortality rate is about 50%.
Symptoms
Symptoms of malnutrition in a child depend on the stage of the disease.
At stage I , the doctor can determine the signs by carefully examining the small patient. Pay attention to insufficiently intense staining and decreased skin turgor, lack of fat in the abdominal area.
At stage II, disturbances in motor activity and appetite are evident. The patient's skin becomes flabby, peels, and does not straighten on its own with mild deformities. The layer of subcutaneous fat remains only on the face. Frequent deviations in the functioning of other systems, attacks of tachycardia or too low blood pressure are recorded.
At stage II , a poor reaction to external stimuli is revealed, the face also loses a layer of subcutaneous fat, and muscle atrophy is noted. Characteristic signs are retraction of the eyeballs and the fontanel area. Disturbances in stool and urination appear, and vomiting is common.
Treatment
Neurologists at the Yusupov Hospital prescribe complex treatment to patients suffering from muscle dystrophy, aimed at eliminating the cause of the disease, influencing the mechanisms of development of the pathological process, and reducing the manifestations of the disease. To improve blood flow in peripheral vessels, angioprotectors (trental, pentoxifylline, chimes), low molecular weight dextran, and prostaglandin E preparations (vasaprostan) are used. After dilating blood vessels with no-shpa and papaverine, the supply of muscle fibers with oxygen and nutrients improves.
B vitamins (thiamine hydrochloride, pyridoxine hydrotartrate, cyanocobalamin) normalize metabolic processes and the conduction of nerve impulses. Biological stimulants stimulate the regeneration of muscle fibers and restore muscle volume: aloe, actovegin, plasmol. To restore muscle conduction, prozerin, galantamine, and armin are used.
Diagnosis of malnutrition
The diagnosis of malnutrition is based not only on determining the presence of underweight in a child, but also on identifying the immediate cause of the development of this pathological condition. An obligatory stage is an examination of the child by a pediatrician, as well as a conversation with the parents, during which the doctor learns all the necessary anamnestic data. After a thorough physical examination of the child and analysis of the life history and illness, additional laboratory and instrumental tests and consultations with specialized specialists (pediatric endocrinologist, gastroenterologist, etc.) are prescribed.
Laboratory diagnostics must necessarily include general clinical tests (general blood and urine tests), coprograms, biochemical blood tests with determination of glucose, total protein (as well as its fractions), liver tests and other indicators.
Of the instrumental diagnostic methods, ultrasound of the abdominal organs, electrocardiography (ECG), and echocardiography (ultrasound of the heart) are mandatory.
If necessary, if indicated, other studies , which help determine the underlying disease against which the malnutrition occurred.
Factors leading to development
The causes accompanying the disease can be external and internal. The first group, characterized by disorders in the body, includes:
- encephalopathy, due to which not only the functioning of the nervous system is disrupted, but also secondary changes occur in the functioning of other organs;
- pathological development of lung tissue, due to which the body does not receive the required amount of oxygen, slowing down its internal processes;
- congenital pathological changes in the functioning of the gastrointestinal tract, leading to insufficient absorption of food;
- surgical operations on the intestines, leading to its shortening;
- diseases of the immune system, leading to the inability to fight infections;
- endocrine changes (most often hypothyroidism or pituitary dwarfism);
- hereditary diseases that disrupt the absorption of certain nutrients (galactosemia, fructosemia, etc.).
The second category includes:
- insufficient nutritional value of breast milk;
- underfeeding;
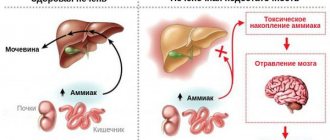
- the impact of toxic factors on the body;
- frequent infectious infections.