For the development of the disease, it is necessary not only to enter the pathogen, but also to have factors that contribute to the further proliferation of the fungus:
- deep skin folds of the feet;
- changes in the chemical composition of sweat;
- endocrine disruptions;
- hyperhidrosis;
- leg skin injuries;
- vegetative-vascular dystonia.
After fungi enter the skin, they can remain in saprophytic form for a long time without causing clinical symptoms. Athlete's disease is characterized by several variants of its course, some of which involve the spread of the process to the nail plate.
Causes
In most cases, athlete's foot is diagnosed in men. Cases among children and adolescents are extremely rare.
The causative agent of the disease (fungus) is transmitted through contact and household contact. You can become infected with athlete's foot, for example, in a bathhouse or after using someone else's personal hygiene products.
Factors that provoke the development of the disease include:
- high temperature and humidity of the environment;
- excess weight;
- skin microtraumas;
- increased sweating;
- sedentary lifestyle.
Treatment of athlete's foot
For a better prognosis, it is important to pay sufficient attention to the correct treatment of infected areas. Doctors strongly recommend daily foot baths with potassium permanganate. All crusts should be carefully removed; the blisters can be opened and the covering removed for better healing. After the baths, wet dressings are applied moistened with 0.1% copper sulfate and 0.4% zinc, or 1% resorcinol solution.
As soon as it is possible to achieve cessation of weeping, the use of Dermozolon or Mycozolon is indicated. To dry and epithelize the ulcers, you can use alcohol dyes and Castellani paint. If necessary, it is possible to use fungicidal pastes or ointments.
The result is determined not only by the chosen drugs, but also by their correct use, taking into account the phase of the disease and the doctor’s advice. After visual normalization and disappearance of painful symptoms, experts recommend conducting a microscopic control examination. If the results are negative, you can stop using antifungal ointments.
Having achieved a positive response from treatment, do not forget about possible relapses. After the main process has subsided, it is necessary to wipe the feet for another month with 1% thymol or 2% salicylic alcohol, after which they must be powdered with boron powder.
It is important to properly care for your shoes. For this purpose, it is recommended to wipe shoe insoles with a solution of formaldehyde, after which the shoes should be stored in an airtight bag for 2 days and then dried. It is advisable to boil the rest of the clothes for 10 minutes. If this is not possible, then you need to get rid of clothes and shoes, because reusing these wardrobe items contributes to a new infection.
Complicated athlete's foot must be treated with antibiotics. Methicillin, Cephaloridine, and Erythromycin are most often prescribed. During the treatment period, you should follow the correct daily routine and bed rest.
Prevention of athlete's foot
In prevention, disinfection of surfaces in all public places that involve skin contact is important. Employees of these places and their regular visitors are recommended to be periodically examined by a dermatologist.
Potential carriers of the fungus must strictly follow the rules of foot and shoe care: at the end of the day, wash your feet with soap, then wipe them dry with a towel, change your socks daily and never wear someone else’s shoes. When going to public baths or a swimming pool, you should use individual slippers, which should preferably be disinfected regularly.
Prevention
To avoid the possibility of inguinal athlete's foot, you need to follow the rules of personal hygiene, especially in saunas and swimming pools. Use a personal towel, washcloth, and underwear.
If a person has suffered this disease, his household items, linen and clothing must be thoroughly disinfected.
If symptoms of inguinal athlete's foot appear, SM-Clinic specialists recommend not delaying going to the doctor and not delaying treatment. You can make an appointment in St. Petersburg by calling the phone number listed on the website.
Symptoms of athlete's foot
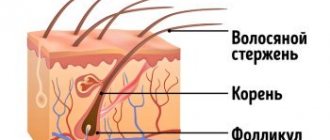
The first symptoms of the disease appear in the form of itching in the interdigital folds, especially between the 4th and 5th fingers. Initially, the itching is minor, accompanied by peeling and cracks, from which serous fluid is released. If nothing is done at this stage, then the remaining interdigital spaces and part of the foot are gradually affected. In conditions of constant weeping, fungi multiply even more abundantly, which contributes to the progression of the disease.
Through the ulcers, the pathogen easily penetrates deep into the tissue, which provokes the development of an eczematous reaction. This complication is manifested by abundant, itchy blisters filled with serous contents.
Such a course can last for years. In this case, periodic purulent complications are possible, when the blisters are filled with thick liquid, and the inflammation spreads to the dorsum of the foot, accompanied by severe pain and limitation of movements.
In one of the variants of the course, conglomerates of deep-lying dense blisters with serous fluid may appear on healthy skin. The vesicles open on their own: first the cover falls off, and then the bottom of the vesicle is exposed, from which serous fluid is regularly separated. The resulting ulcers can merge and spread to large areas of the skin of the soles, causing significant discomfort when walking.
During the process of reproduction, fungi produce toxins that have a sensitizing effect. The immune system responds by developing an allergic reaction in the form of a rash, localized mainly on the palms. The rash consists of small blisters with a serous component, which, when bursting, expose the delicate, weeping surface of the epidermis. Microscopy of scrapings from these ulcers fails to identify fungi, since the process is caused not by the pathogen itself, but by their toxins.
The peak incidence of dermatomycosis is observed in the summer, since during this period all predisposing factors are realized.
When the nail plate is damaged, excessive subungual hyperkeratosis develops. The nail becomes yellow and the edge becomes jagged. Most often, such changes appear on the 1st and 5th toes, since they have the maximum contact with the infected surface.
Symptomatic picture of mycosis
Candidiasis of the inguinal folds is caused by specific fungi, which are opportunistic microorganisms that live on the skin and mucous membranes of any healthy person. The immune system, functioning without failures, suppresses the active activity of pathogenic microflora, so they remain in a latent state in the human body. However, under the influence of pathological exogenous and endogenous factors, the immune system is weakened and ceases to fully perform its functions. This contributes to the activation of the infection and its unhindered reproduction.
The active activity of a fungal pathogen on the skin in the groin area is manifested by the following pathological symptoms:
- Formation of spots in the groin. The lesions have clear boundaries and differ in color from healthy areas. The shade of the spots ranges from light pink to deep red.
- Peeling of the skin. In places where a fungal infection is localized, the skin becomes covered with a white coating and peels off. Peeling may spread to the perianal and pubic areas, as well as to the folds of skin between the groin and thigh.
- Uncomfortable sensations. In the groin area, the patient is bothered by severe, sometimes unbearable itching, which can cover the femoral part of the lower limb.
- Irritation. Swelling, redness, and irritation form at the site of active fungal activity.
On the skin of the groin area affected by the fungus, round, deformed areas are visualized, which differ from healthy skin in shade and the presence of peeling on the surface. Thanks to such visual signs, the doctor can make a preliminary diagnosis, which will be confirmed by the results of a comprehensive diagnostic examination.
results
ECS was recorded significantly more often (1.8 times) in men compared to women (63.8 and 36.2%, respectively; p
<0.05).
The largest number of patients belonged to the age group 35-55 years (48.1%; p
<0.05); aged 18-35 years - 25.1%; over 55 years old - 22.5%; rarely the disease was registered before 18 years of age (4.3%).
The distribution of ECS patients, taking into account the duration of the disease, is presented in Fig. 1. More than 1/3 (37.6%) of patients had a disease duration of up to 1 month, up to 2 months - 21.6%, up to 6 months - 20%, over 6 months - 20.8%.
Rice. 1. Distribution of ECS patients taking into account the duration of the disease, % (n=235).
In 146 (62.1%) patients, ECS occurred against the background of concomitant somatic pathology. The spectrum and incidence of somatic pathology are presented in Fig. 2. In the structure of concomitant ECS somatic diseases, diabetes mellitus was in the lead (40.6%), gastrointestinal pathology accounted for 20.6%, vegetative-vascular dystonia 15.1%, bronchial asthma 11.6%, 6.3% - chronic venous insufficiency, 7.1% - other diseases. Against the background of dermatological pathology, ECS was registered in 41 (17.4%) patients. Its structure was dominated by acne (19.5%), microbial eczema (17.1%), psoriasis (14.5%), rosacea (12.2%). The proportion of other dermatoses was minimal: seborrhea (9.8%), basal cell carcinoma (4.9%), true eczema (4.9%). It is important that almost half of the patients (45.1%) with ECS received treatment with TA of various groups before the start of the survey. The choice of drug depended on the qualifications, experience and personal priorities of the doctor. Preference was given to azoles (64.2%), less often allylamines were prescribed (18.8%), as well as drugs of other groups (17%). Repeated visits to the doctor during the multicenter study clearly indicate a relapse of the disease, the cause of which could be non-compliance with treatment regimens, self-medication, re-infection, lack of disinfection measures, as well as the development of fungal resistance to TA.
Rice. 2. Spectrum and incidence of concomitant somatic pathology in patients with ECS, % (n=235).
Features of the course of ECS at the present stage have been identified. The main subjective symptom was itching, which was reported in almost all patients ( n
=231;
98.3%), including weak ( n
=113; 48.9%), moderate (
n
=80; 34.6%) and strong (
n
=38; 16.5%).
Only a few people reported pain, mainly during ECS with complications ( n
= 21; 8.9%).
The frequency of lesions of various large folds (by anatomical region) was determined (Fig. 3). Almost all patients ( n
=224;
95.3%) localization of rashes was identified in the area of the inguinal folds (Fig. 4, a, b). Less frequently infected were the intergluteal fold ( n
=37, 15.7%) (see Fig. 4, c), folds under the mammary glands (
n
=23; 9.8%) and axillary folds (
n
=11; 4.7% ) (see Fig. 4, d).
One atomic region of the folds was affected in ¾ ( n
= 180; 76.6%) of patients, two - in 40 (20%), three - in 8 (3.4%) patients (Fig. 5). The average number of regions per ECS patient was 1.26±0.25. In most cases, the damage to large folds with epidermophytosis was symmetrical (61.3%). With a unilateral process, an experienced clinician, with a certain degree of probability, assumes the possibility of mycocarriage and/or a hidden course of the process on the opposite side. Therefore, in order to prevent relapse of the disease, prophylactic treatment of a symmetrical, externally unchanged large fold is carried out.
Rice. 3. Frequency of damage to various large folds (by anatomical region) with epidermophytosis, % (n=235).
Rice. 4. Localization of the process during ECS. a - inguinal folds with the process spreading to the thighs and scrotum; b - inguinal folds with the process spreading to the thighs and labia majora; c — epidermophytosis in the area of the intergluteal fold; d — epidermophytosis in the axillary region.
Rice.
Fig. 5. Distribution of ECS patients, taking into account the number of large folds involved in the process, % (n=235). An assessment was made of the characteristics and occurrence of rashes during ECS (Fig. 6). The main clinical manifestations of ECS were erythema ( n
=235, 100%), scales (
n
=208; 88.5%), infiltration in the area of the lesion (
n
=159; 67.7%), papules (
n
=134; 57%), maceration (
n
=75 ; 31.9%), cracks (
n
= 73; 31.1%).
Exudative morphological elements were recorded less frequently - pustules ( n
= 51; 21.7%) and vesicles (
n
= 39; 16.6%), accompanied by oozing (
n
= 69; 29.4%). The clinical characteristics of the rashes indicate that in 70.6% of patients with ECS, TA in the form of a cream was initially indicated.
Rice.
6. Characteristics and incidence of rashes in patients with ECS, % (n=235). The main clinical characteristics of ECS are the presence of pink or red erythema, with a bluish tint in the chronic form of the disease. The spots have peripheral growth and merge with each other. Along the periphery of the lesion there is a pronounced continuous edematous ridge, on the surface of which papules and vesicles are located. It’s not for nothing that ECS is called “fringed eczema” ( exezema
marginatum
).
In the center of the lesion, resolution of the process is observed with pronounced fine-plate peeling and weak erythema (Fig. 7, a). This classic course of ECS was recorded in 1/3 of patients (32.7%). It should be noted that in 2/3 (67.3%) of cases, erythema was combined with skin infiltration. The spread of the process along the upper third of the thighs occurred in more than half of the patients ( n
= 135; 57.7%) (see Fig. 7, b). Clinically verifiable damage to the scrotum in the form of erythema of varying intensity was detected in 101 (67.3%) men (Fig. 8).
Rice. 7. Inguinal athlete's foot. a - the classic version of the course, designated as “fringed eczema” (eczema marginatum); b - peripheral growth of the focus of inguinal epidermophytosis with the spread of the process to the thighs.
Rice.
8. Inguinal epidermophytosis in men with lesions of the scrotum of varying degrees of intensity. a - light; b - moderate; c - strong. Concomitant ECS mycosis of the feet was present in 1/3 of the patients ( n
=77; 32.7%) (Fig. 9). Among the clinical forms of mycosis of the feet, the leading form was the intertriginous form (66.2%) (Fig. 10, a, b). Dyshidrotic (19.5%) and squamous (14.3%) forms were equally common. In men, mycosis of the feet was recorded 1.7 times more often than in women (63.6% versus 36.4%).
Rice. 9. Incidence of concomitant mycosis of the feet in patients with ECS, % (n=235).
Rice.
10. Mycoses of the feet identified in patients with athlete's foot. a - intertriginous athlete's foot with severe maceration of the epidermis; b - intertriginous athlete's foot with peeling and single blisters. Onychomycosis was diagnosed in ¼ of patients ( n
=58;
24.7%), as well as its combination with mycosis of the feet - in 55 (71.4%) patients. Onychomycosis was recorded significantly 1.9 times more often in men (65.5% versus 34.5%). The nail plates of the fifth finger were most often affected ( n
= 31; 53.4%), less often - II (
n
= 18; 31%), and in some patients - III (15.5%). The normotrophic type of onychomycosis prevailed 2.2 times over the hypertrophic type (69% versus 31%).
The data obtained indicate that ECS often occurs as a multifocal process, when not only the inguinal folds are affected, but also the folds of other localizations, the scrotum, thighs, feet, and nail plates (Fig. 11).
Rice. 11. Patient V., 47 years old. Multiple foci of epidermophytosis. a - in the intergluteal region; b - in the area of the inguinal folds; c — intertriginous and dyshidrotic athlete’s foot; d — vesiculobullous epidermophytids on the hands.
Complications of pacemaker were registered in 1/3 ( n
=78;
34.6%) patients. In the structure of complications, secondary pyoderma predominated ( n
= 38; 48.7%) (Fig. 12, a), mycotic eczema (
n
= 27; 34.6%) took second place (see Fig. 12, b, c) , allergic dermatitis was recorded less frequently (
n
= 13; 16.7%). Epidermophytids were detected in 20.4% of patients: they predominated on the hands in 54.2% of patients (see Fig. 12, d), less often recorded on the hips - in 29.2% (Fig. 13, a, b) and on buttocks - in 14.7%. Mycotic sensitization in men was recorded significantly more often (1.5 times) than in women (60.4% versus 39.6%).
Rice. 12. Complications of epidermophytosis of large folds. a - inguinal epidermophytosis, complicated by secondary pyoderma, epidermophytida on the thigh; b — epidermophytosis of the intergluteal fold, complicated by mycotic eczema (left buttock) after local therapy with zinc paste, epidermophytida on the right buttock; c — epidermophytosis of the intergluteal fold, complicated by mycotic eczema on both buttocks after local therapy using furatsilin solution.
Rice.
13. Epidermophytids. a - erythematous-urticarial rashes on the thighs with damage to the inguinal folds; b - erythematous-squamous rashes on the thighs with damage to the intergluteal and inguinal folds. The effectiveness of sertaconazole has been assessed ( Zalaina
) in the treatment of ECS, taking into account the clinical features of the disease. Treatment regimens for patients with ECS occurring alone or in combination with epidermophytosis of other localizations have been unified.
1. For uncomplicated ECS, sertaconazole cream ( Zalain
) rubbed into lesions on the skin (folds, thighs, scrotum, feet) and nails 2 times a day (morning and evening) until clinical manifestations are completely resolved. To enhance the penetration of the cream into the nail plates, patients were asked to file off the shiny layer after a soda-soap bath.
2. For ECS complicated by mycotic eczema or allergic dermatitis, and in the presence of epidermophytis, suprastinex or parlazin was prescribed orally, 1 tablet at night. The course of treatment was 10 days.
3. In the presence of pustules (athlete's foot, complicated by secondary pyoderma or mycotic eczema), betadine solution (area of folds) or betadine ointment (outside the folds) was used externally.
Recovery was considered to be the resolution of all clinical manifestations of dermatophytosis in the patient; significant improvement - reduction in the area of lesions, predominance of erythema in the clinical picture of the disease, disappearance of papules, vesicles, epithelization of erosions; improvement - preservation of the area of lesions with positive dynamics of resolution of rashes.
After 1 week, doctors noted improvement in 80.9% of cases (Fig. 14). In 15.7% of patients, no signs of recovery or positive dynamics were recorded. After 2 weeks, recovery occurred in 11.1% of patients, significant improvement in 73.2%. The overall therapeutic effect (recovery and significant improvement) was 84.3%.
Rice. 14. The effectiveness of treatment with sertaconazole in patients with epidermophytosis of large folds in the entire sample (n=235, %).
After 3 weeks, ECS was completely resolved in 45.5% of patients, and significant improvement was noted in 54.5% of patients. The overall therapeutic effect was 100%. After 1 month, almost all patients recovered (98.7%).
The use of Spearman's correlation coefficient (SCC) made it possible to identify the dependence of the timing of resolution of clinical manifestations of ECS and mycosis of other localizations on a number of factors.
— The recovery time correlated with the age of the patients (CCR = 0.276) (Fig. 15). After 2 weeks, recovery occurred 2.4 times faster in the age group under 35 years than in older patients (18.8% versus 7.8%); after 3 weeks - 1.8 times faster (66.7% versus 36.7%).
Rice. 15. Recovery time for patients with ECS, taking into account the age of the patients (CCR = 0.276).
— The recovery time was associated with the duration of the pathological process on the skin (up to 2 months or more) (KCR = 0.204) (Fig. 16). In patients with a disease duration of up to 2 months, after 2 weeks the process resolved 1.6 times faster (13.2% versus 8.1%), and after 3 weeks - already 3.8 times faster (50% versus 13.1 %).
Rice. 16. Recovery time for patients with ECS, taking into account the duration of the disease (CCR = 0.204).
— The presence of concomitant somatic pathology seriously influenced the recovery time of patients (CMR = 0.411) (Fig. 17). After 2 weeks, recovery was recorded mainly in patients with no somatic pathology (23%), and after 3 weeks this figure increased to 79.8%. In patients with somatic pathology, recovery after 3 weeks was recorded in 27% of cases, but only in isolated cases in the presence of diabetes mellitus (6.8%).
Rice. 17. Recovery time for ECS patients, taking into account concomitant somatic pathology (CCR = 0.411).
— The recovery time of patients was significantly influenced by previous TA therapy (CCR = 0.207) (Fig. 18). If patients had not previously received local TA therapy, then after 2 weeks the process resolved 6.4 times faster (17.8% versus 2.8%), and after 3 weeks - 3.6 times faster (67.4% versus 18.9%).
Rice. 18. Recovery time for patients with ECS, taking into account previous therapy with topical antimycotics of other groups (CCR = 0.207).
— The recovery time of patients depended on the number of large folds (anatomical areas) involved in the process (KCR = 0.411) (Fig. 19). After 2 weeks and after 3 weeks, the process resolved mainly when the rash was localized in the folds of one anatomical area (13.9 and 57.2%, respectively). When two or more folds were involved in the process (according to anatomical areas), recovery occurred mainly after 1 month.
Rice. 19. Recovery time for ECS patients, taking into account the number of anatomical areas involved in the process (KCR = 0.411).
— A correlation was established between the timing of resolution of ECS occurring with and without mycosis of the feet (CMR = 0.334) (Fig. 20). After 2 weeks, recovery was achieved in 27.3% of patients without concomitant mycosis of the feet and in a few patients (3.2%) with it. After 3 weeks, these differences were 8.9%. The presence of onychomycosis also influenced the recovery time of patients (CCR = 0.234). After 2 weeks, in the absence of it, 13.5% of patients recovered, and in its presence, only 3.4%. After 3 weeks, these indicators differed by 1.8 times (52% versus 28.9%).
Rice. 20. Recovery time for patients with ECS, taking into account the presence of mycosis of the feet (CCR = 0.334).
— Complications accompanying ECS also influenced the recovery time of patients (CCR = 0.418) (Fig. 21). After 2 weeks, recovery was observed mainly in patients with no complications (13.6%). After 3 weeks, in this group, complete resolution of clinical manifestations was registered 4.3 times more often than in the presence of complications (58% versus 13.6%). The presence of mycogenic sensitization lengthened the recovery time of patients (CMR = 0.334). Recovery of patients after 2 weeks in the absence of epidermophytis was observed in 13.9% of cases, and in their presence such cases were not registered. After 3 weeks, in the absence of epidermophytids, 3.5 times more patients recovered (45% versus 12.5%).
Rice. 21. Recovery time for patients with ECS, taking into account complications (CCR = 0.418).
Material and methods
The work was carried out as part of a multicenter study “Study of real practice in the treatment of patients with dermatomycosis in the Russian Federation”, conducted in 2012–2013. under the patronage of the pharmaceutical plant EGIS (Hungary) simultaneously in 50 regions of the Russian Federation. 97 medical and preventive institutions of various profiles, 174 doctors are involved. To unify the research, an original version of the questionnaire was developed. Instructions have been prepared for filling out the questionnaire in the form of a multimedia presentation containing a detailed analysis of the differential diagnostic criteria for epidermophytosis, rubromycosis and candidiasis of large folds with photographs of patients. The questionnaire also asked people to express their own opinion about the peculiarities of the course of mycosis in the patient. In total, doctors filled out 5025 questionnaires for patients with MVP. There were 2784 patients with dermatophytosis, including 735 (26.4%) with dermatophytosis of large folds. Patients with ECS predominated ( n
=615; 83.7%). One of the conditions of the experiment was the selection of patients with minimal damage to the nail plates, when the KIOTOS index (clinical index for assessing the severity of Sergeev’s onychomycosis) allowed only local therapy for mycosis of the feet.
The work was carried out in stages.
Stage I. Processing questionnaires of pacemaker patients filled out by doctors using Excel. Of the 615 questionnaires, 235 (38.2%) contained complete data. The sample was representative to obtain reliable data.
Stage II. Studying the features of the course of ECS in Russia.
Stage III. Multivariate analysis of the effectiveness of ECS treatment with sertaconazole ( Zalain
).
Statistical processing of the research results was carried out in the laboratory of mathematical theory of experiment, Faculty of Biology, Moscow State University. M.V. Lomonosov using the statistical software package Stastica 6.0. The method of correlation analysis (Spearman coefficient) was used. Those values of correlation coefficients for which p
was less than the significance level (α=0.05), i.e. these coefficients were statistically significantly different from zero.
Epidermophyton floccosum - the causative agent of athlete's foot
The fungi Epidermophyton flocosum are anthropophylls. They cause disease only in humans. Most often, the superficial layer of smooth skin is affected: most often the inguinal folds, less often the intergluteal folds, folds in the lower abdomen and under the mammary glands.
Microscopy of skin scales taken from the affected areas reveals short (2 - 4 µm) branching intertwined mycelium and rectangular arthrospores arranged in chains. When growing on Sabouraud's nutrient medium, the colonies are round in shape, initially flat or dome-shaped, later folded-lumpy with depressions in the center. The surface is velvety-mealy or leathery with radial folds. Initially grayish-brown, lemon-olive or yellowish-green, later white.
Under microscopy, in mature cultures one can see septate mycelium with blunt-pointed macroconidia, which are arranged in the form of clubs or banana bunches in bunches of 3-5 pieces, growing directly from hyphae. Chlamydospores appear in old crops. Microconidia are absent.
Rice. 3. View of colonies of the fungus Epidermophyton flocosum at different stages of growth.
Rice. 4. Microscopy of mature cultures of the fungus Epidermophyton flocosum.
Who is at risk: causes of the disease
The optimal conditions for the development of fungal infections are heat and humidity. Male professions (driver, military man) oblige a person to wear warm, unventilated clothes for long hours, day after day creating an optimal habitat for the causative agent of the disease.
A weakened body, the presence of mycosis on other areas of the skin, contact with people who are carriers of mycoses, metabolic disorders are factors that increase the risk of epidermophytosis.
Knowing the causes of the disease, we can identify the main categories of men who are at risk:
- elderly people;
- patients with diabetes and (or) obesity (treated and advised by an endocrinologist);
- men with hyperhidrosis (this means profuse, uncontrollable sweating);
- people with immunodeficiency;
- drivers, military, police, rescuers, etc.
Procedures and operations
In advanced forms of onychomycosis and irreversible changes in the nail plate, the patient may be offered surgical removal of the nail plate, which is performed under local anesthesia. After surgery, an antibiotic and antifungal ointment is applied to the wound. The dressing is changed twice a day. The course of treatment with local antifungal agents continues until a healthy nail grows - this may take 6-9 months.
Laser removal of the nail plate is also used. The procedure is less painful and bloodless than conventional surgical nail removal, is characterized by rapid tissue restoration, and there is no deformation of the growing nail. If the nail plate is slightly affected, it is not completely removed using a laser. It is enough to destroy the mycelium and spores of the pathogen with laser exposure. With the help of a laser, this is possible because it penetrates 7-8 mm through the nail into the soft tissue. The course of treatment is 4-5 procedures, and after a month it is recommended to repeat the course of treatment.
What treatment therapy should I use?
Before prescribing treatment for inguinal candidiasis, it is necessary to establish an accurate diagnosis and identify the pathogen. Therefore, after an initial examination and history taking, the doctor gives a referral for a comprehensive diagnostic examination, including the following procedures:
- microscopy;
- bacterial sowing;
- molecular biological analysis.
Treatment of candidiasis in the groin should be comprehensive and carried out under the strict supervision of a doctor. Self-medicating with such a disease is dangerous and fraught with serious complications.
The treatment plan includes the following activities:
- Identification and elimination of factors that provoke immunodeficiency.
- Prescription of antifungal and symptomatic therapy.
- General strengthening therapy.
To combat a fungal infection localized in the groin, local antifungal drugs are prescribed in the form of creams and ointments, which contain an antimycotic component. In the fight against fungi, drugs such as:
- "Nystatin";
- "Natamycin";
- "Clotrimazole".
If the disease is advanced and accompanied by serious complications, in addition to topical medications, antifungal medications are prescribed for oral administration in the form of capsules and tablets:
"Fluconazole";
"Itraconazole"
In the most advanced cases, the doctor will recommend intravenous or intramuscular administration of antimycotics. As soon as the condition improves, you can switch to tablets.
In case of correct treatment, the disease completely disappears within 7–10 days. To confirm complete recovery, repeat tests must be taken after completing the main course. If the fungal infection is completely eradicated, the laboratory test results will be negative.
In addition to drug treatment, it is important to follow preventive measures that enhance the therapeutic effect and reduce the risk of relapse to zero. Therefore, together with drug therapy, it is advisable to follow the following rules of prevention:
- strengthen immunity;
- lead a healthy, active lifestyle;
- get rid of bad habits;
- maintain personal hygiene;
- normalize weight;
- use products that control sweat in large folds.
If there is no treatment for inguinal candidiasis, the fungal infection will gradually spread throughout the body, causing health and life-threatening complications. Therefore, if you have suspicious symptoms, you must make an appointment with a dermatovenerologist, take all tests and be treated under the supervision of a specialist.
How does it manifest?
At the moment, modern medicine has discovered several varieties of the described disease, which include: squamous, intertriginous, dyshidrotic and erased type. All types of illness have the ability to replace each other and be combined. The most common complaints encountered in medical practice include:
- The appearance of allergic rashes.
- The formation of red plaques with the additional effect of whitish peeling on the roof.
- Formation of yellow calluses with cracks on top.
- Irritating itching.
- The presence of edema and erosion.
- The presence of inflamed acne.
- Increased levels of nail brittleness and rejection.
- Bloody and purulent discharge.
Tests and diagnostics
- Microscopy of pathological material is used as a method of preliminary diagnosis.
- Isolation of a pathogen culture (growth of the pathogen in a culture) takes time.
- Polymerase chain reaction (PCR). It makes it possible to obtain results within 24 hours that are highly specific (90-98%). It is especially important for onychomycosis and atypical forms of dermatomycosis, since in the earliest stages it allows to prescribe rational therapy, reduce complications and the severity of lesions.
List of sources
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections (a guide for doctors). M., 2003. 185–193.
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257–311.
- Sergeev V.Yu., Sergeev A.Yu. Dermatophytes: new in the diagnosis, therapy and prevention of the most common human mycoses. Consilium medicum. – Dermatology. – 2008. – No. 1. – P. 30–35.
- Haldin A.A., Sergeev V.Yu., Izyumova I.M. Modern ideas about inguinal dermatophytosis: etiology, epidemiology, clinical picture and effective therapy. Ross.zhur. leather and veins Bol. – 2005. – No. 5. – S. 43–48.