Roaccutane
Roaccutane (isotretinoin) is one of the most effective drugs for the treatment of acne and other skin diseases accompanied by hyperplasia of the sebaceous glands (rosacea, etc.). Belongs to the group of synthetic retinoids. It stops the hyperproliferation of the excretory ducts of the sebaceous glands, promotes the unhindered secretion of sebum, its production decreases, and accordingly, the inflammatory reaction of the skin decreases.
A distinctive feature from other drugs is the ability to suppress the secretion of sebum, eliminate hyperkeratosis, and also suppress the activity of the bacterium P. Acnes. Only a doctor who has experience with this drug should prescribe treatment with Roaccutane. Each individual patient is prescribed an individual dose depending on the form and severity of the disease, as well as the condition of the skin. During the course of therapy, the doctor may adjust this dose by decreasing or increasing it.
Effect
A positive result after treatment with Roaccutane occurs within several months. Already in the first month, you can observe a decrease in the signs of seborrhea and the release of sebaceous ducts. Inflammation on the face and body disappears almost completely after 3-4 months, and by the end of 5-6 months the patient recovers. As a rule, one course is enough. In 90% of cases, after treatment with Roaccutane, acne relapses do not occur. However, if necessary, it is possible to conduct a repeat course.
Side effects
Dermatological reactions such as:
- dry mucous membranes,
- itching,
- skin rash,
- cheilitis.
In some cases, photophobia, conjunctivitis, and hearing loss are likely.
Contraindications and precautions
Contraindications include pregnancy, breastfeeding, individual intolerance to isotretinoin (the main active ingredient), taking tetracycline antibiotics during the period of intended treatment. Avoid taking Roaccutane orally if you have existing liver and kidney damage, pancreatitis, or hypervitaminosis. Use with caution for various chronic intoxications.
If the disease worsens during therapy, as a rule, taking Roaccutane is canceled for several days and then resumed again. The doctor should warn women about the peculiarities of treatment with Roaccutane. Since the drug has teratogenic properties (disruption of the process of embryogenesis), women of childbearing age should discuss all possible risks before taking the drug. The possibility of pregnancy during the treatment period, as well as for a year after it, should be completely excluded.
Roaccutane caps 20mg N30 (Hoffman-La Roche)
Roaccutane should only be prescribed by physicians, preferably dermatologists, who are experienced in the use of systemic retinoids and are aware of the drug's teratogenicity risk. Both female and male patients should be given a copy of the Patient Information Leaflet. To avoid accidental exposure of the drug to the body of other people, donated blood should not be taken from patients who are receiving or have recently (1 month) received Roaccutane. It is recommended to monitor liver function and liver enzymes before treatment, 1 month after treatment, and then every 3 months or as indicated. A transient and reversible increase in liver transaminases was noted, in most cases within normal values. If the level of liver transaminases exceeds the norm, it is necessary to reduce the dose of the drug or discontinue it. Fasting serum lipid levels should also be determined before treatment, 1 month after initiation, and then every 3 months or as indicated. Typically, lipid concentrations normalize after dose reduction or discontinuation of the drug, as well as with diet. It is necessary to monitor a clinically significant increase in triglyceride levels, since their rise above 800 mg/dL or 9 mmol/L can be accompanied by the development of acute pancreatitis, possibly fatal. In case of persistent hypertriglyceridemia or symptoms of pancreatitis, Roaccutane should be discontinued. In rare cases, depression, psychotic symptoms, and very rarely, suicide attempts have been described in patients treated with Roaccutane. Although their causal relationship with the use of the drug has not been established, special caution should be exercised in patients with a history of depression and all patients should be monitored for the occurrence of depression during treatment with the drug, if necessary, referring them to an appropriate specialist. However, discontinuation of Roaccutane may not lead to the disappearance of symptoms and further observation and treatment by a specialist may be required. In rare cases, at the beginning of therapy, an exacerbation of acne is observed, which resolves within 7-10 days without adjusting the dose of the drug. Several years after the use of Roaccutane for the treatment of dyskeratosis, at a total course dose and duration of therapy higher than those recommended for the treatment of acne, bone changes developed, including premature closure of the epiphyseal growth plates, hyperostosis, calcification of ligaments and tendons. Therefore, when prescribing the drug to any patient, the ratio of possible benefits and risks should first be carefully assessed. Patients receiving Roaccutane are recommended to use moisturizing ointment or body cream, lip balm to reduce dry skin and mucous membranes at the beginning of therapy. During post-marketing surveillance with the use of the drug Roaccutane, cases of severe skin reactions, such as erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis, have been described. These events can be serious and can lead to disability, life-threatening conditions, hospitalization or death. Patients receiving Roaccutane require careful monitoring to identify severe skin reactions and, if necessary, consider discontinuing the drug. While taking Roaccutane, pain in muscles and joints and an increase in serum creatinine phosphokinase are possible, which may be accompanied by a decrease in tolerance to intense physical activity. Deep chemical dermoabrasion and laser treatment should be avoided in patients receiving Roaccutane, as well as for 5-6 months after the end of treatment due to the possibility of increased scarring in atypical places and the occurrence of hyper- and hypopigmentation. During treatment with Roaccutane and for 6 months after it, hair removal using wax applications cannot be performed due to the risk of epidermal detachment, scar development and dermatitis. Since some patients may experience a decrease in night vision acuity, which sometimes persists even after the end of therapy, patients should be informed about the possibility of this condition, advising them to exercise caution when driving at night. Visual acuity must be carefully monitored. Dryness of the conjunctiva of the eyes, corneal opacities, deterioration of night vision and keratitis usually disappear after discontinuation of the drug. If the mucous membrane of the eyes is dry, you can use applications of a moisturizing eye ointment or an artificial tear preparation. Patients with dry conjunctiva should be monitored for possible development of keratitis. Patients with vision complaints should be referred to an ophthalmologist and consider the advisability of discontinuing Roaccutane. If you are intolerant to contact lenses, you should use glasses during therapy. Exposure to sunlight and UV rays should be limited. If necessary, use sunscreen with a high protection factor of at least 15 SPF. Rare cases of the development of benign intracranial hypertension (“pseudotumor cerebri”) have been described, incl. when used in combination with tetracyclines. In such patients, Roaccutane should be discontinued immediately. During therapy with Roaccutane, inflammatory bowel disease may occur. In patients with severe hemorrhagic diarrhea, Roaccutane should be immediately discontinued. Rare cases of anaphylactic reactions that occurred only after previous external use of retinoids have been described. Severe allergic reactions dictate the need to discontinue the drug and carefully monitor the patient. Patients at high risk (with diabetes, obesity, chronic alcoholism or lipid metabolism disorders) may require more frequent laboratory monitoring of glucose and lipid levels when treated with Roaccutane. If diabetes is present or suspected, more frequent monitoring of glycemia is recommended.
The use of systemic retinoids in a “low dose” mode in patients with moderate to severe forms of acne
Application of Systemic Retinoids In the mode of small doses in patients with moderate-severe form of acne
Acne is a chronic, recurrent disease of the sebaceous glands and hair follicles (2).
The disease is widespread in adolescence. Acne is less common in infants and adults. The main role in the genesis of acne is played by hereditary predisposition, which determines the number, size and increased sensitivity of sebaceous gland cell receptors to the male sex hormone testosterone and its metabolites (3, 5). The initial stage of acne development is the formation of retention hyperkeratosis at the mouth of the hair follicle. Hyperandrogenemia leads to hyperplasia and hypersecretion of the sebaceous glands. Hyperkeratosis and excessive sebum production lead to obstruction of the sebaceous gland duct and the formation of comedones (6, 7).
Under the created anaerobic conditions, Propionibacterium acnes multiplies. Despite the key importance of this microorganism, staphylococci are also involved in the development of the inflammatory process in the sebaceous glands. The growth of bacteria initiates the development of the inflammatory process, forming inflammatory elements of acne - papules, pustules, nodules or cysts. Recurrent ruptures of cysts with their subsequent re-epithelialization lead to the formation of epithelial tracts, which are often accompanied by disfiguring scars.
Severe forms of acne, as well as the tendency of the disease to recur, are usually genetically determined. In this regard, traditional therapy with antibiotics, topical agents, as well as various cosmetic treatments do not allow achieving a lasting therapeutic result. Often the use of topical agents (topically acting retinoids and antibiotics, azelaic acid, combination drugs) turns out to be very effective directly in the treatment of patients. However, frequent relapses of the disease during standard therapy not only contribute to the formation of post-acne, but also have an adverse psychological effect on adolescent patients, leading to the formation of dysmorphophobia, depression, and in some cases, suicidal thoughts.
Systemic retinoids are effective therapeutic agents for severe forms of acne, ineffectiveness of antibacterial drugs, and the formation of hypertrophic and keloid scars (4, 8, 9, 15).
In recent years, dermatovenerologists have begun to increasingly use drugs from this group in the treatment of acne patients. This is due to the accumulated experience of their use in real clinical practice in Russia, as well as the emerging confidence of specialists in the high safety of systemic retinoids with long-term use in people with severe forms of acne.
Of no small importance in the popularity of isotretinoin is its universal mechanism of action, which allows it to have a beneficial effect on all four components of acne pathogenesis. Isotretinoin is able to suppress sebum production by 80%; effectively reduce the phenomena of follicular hyperkeratosis and indirectly inhibit the growth of anaerobic bacteria, reducing inflammation of the sebaceous glands and hair follicles (10, 11).
Moreover, when using standard doses and dosage regimens, isotretinoin induces long-term remission of the disease or leads to permanent cure of patients (12, 13, 14).
At the same time, in 2010, the expert council of the Russian Society of Dermatovenerologists considered it appropriate to recommend to practitioners a new strategy for managing patients with moderate to severe forms of the disease using a “low-dose” isotretinoin regimen (1). First of all, this strategy is aimed at managing patients suffering from recurrent acne of moderate severity, who had a good therapeutic result from the use of topical agents, but the process resumed again after discontinuation of topical therapy.
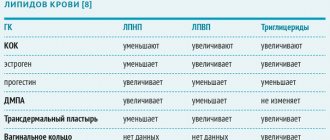
Table 1.
Dynamics of main laboratory parameters in patients with acne who used the “small dose” regimen of Roaccutane (M±m)
| Laboratory indicator | Donors (n=40), | Patients with acne before treatment (n=40) | Patients with acne who received Roaccutane for 1 month (n=40) | Patients with acne who received Roaccutane for 2 months (n=40) | Patients with acne who received Roaccutane for 3 months (n=40) | R |
| Cholesterol, µmol/l | 3,7±0,1 | 5,0±0,7 | 5,1±0,7 | 5,3±1,2 | 5,2±2,7 | >0,05 |
| Triglycerides, µmol/l | 1,7±0,01 | 1,8±0,02 | 1,9±0,02 | 1,8±0,4 | 1,9±0,8 | >0,05 |
| AST, U/l | 32±0,5 | 34±0,9 | 35±0,9 | 35±0,7 | 35±0,8 | >0,05 |
| ALT, U/l | 24±0,8 | 25±0,7 | 25±0,8 | 25±1,7 | 25±1,9 | >0,05 |
Note: p - significance of differences between the group of people treated with Roaccutane and donors
In such cases, the initial dose of the drug should be calculated in the range of 0.1-0.15-0.3 mg/kg/day. in permanent (daily) or intermittent (every other day) regimens, or prescribed in a standard dose of 10 mg per day, regardless of body weight, followed by a stepwise reduction (after 1 month - up to 5 times a week; after another month - up to 3 times a week a week, after another month - up to 2 times a week; after another month - up to 1 time a week). The duration of treatment with isotretinoin according to the “low-dose” regimen should not on average exceed 3 to 6 months. From a practical point of view, an important advantage of this method of using isotretinoin is that there is no need to calculate the total course dose of the drug.
The purpose of our study was to study the effectiveness and safety of the use of isotretinoin (Roaccutane) in a “low dose” regimen in patients with recurrent acne of moderate severity.
Material and research methods
We observed 40 patients with acne aged 18 to 27 years (women - 25 (62.5%); men - 15 (37.5%). In all study participants, acne manifested itself at puberty.
The inclusion criteria for the study were: the presence of moderate to severe acne; good therapeutic effect from 2 or more courses of adequate topical therapy for the disease with subsequent relapses of acne; signing an informed consent to participate in the study.
Exclusion criteria were: a history of indications for therapy with systemic retinoids, antiandrogen drugs; the fact of use of systemic antibiotics or topical retinoids during the last 3 months; the presence of clinically significant changes in hematological and (or) biochemical blood tests; presence of mild or severe forms of acne; presence of pregnancy; the presence of chronic liver failure or Gilbert's syndrome.
Inflammatory efflorescences were predominantly recorded on the skin in the form of multiple papules and papulopustules of a bright pink color, small in size (up to 0.5 cm in diameter) with uneven outlines, slightly rising above the surface of the skin. In 8 (20%) cases, single nodes (cysts) were also visualized.
Against this background, all patients had severe seborrhea, as well as the presence of non-inflammatory forms of acne - open and closed comedones. Despite a long history of acne, the observed individuals did not have scars or other post-acne lesions on their skin.
In 32 (80%) of the observed patients with acne, skin lesions were limited to the facial area. In 8 (20%) cases, multiple papulopustular elements were also localized in the upper third of the chest and back.
All patients had previously received various types of therapy. 18 (45%) patients received systemic antibiotics more than 3 months before participating in the study. Topical retinoids had previously been used by 26 (65%) patients; azelaic acid preparations - 11 (27.5%) respectively; topical agents with antibacterial action - 35 (87.5%); combination drugs - 19 (47.5%). It is noteworthy that, according to the recommendations of specialists, all 40 patients previously observed used other various topical agents, which, from the point of view of evidence-based medicine, are ineffective for acne.
Facial skin care in 16 (40%) patients with acne was ineffective and consisted of repeated use throughout the day of various cleansing gels, scrubs, as well as alcohol-containing products, which contributed to additional irritation of the skin. On the contrary, 5 (12.5%) study participants did not carry out any hygienic care measures for oily or dry skin in seborrheic areas.
To assess the severity and extent of the disease, the Acne Dermatology Index (ADI) was used, which takes into account the number of comedones, papules, pustules, and nodules in the subject being examined.
All patients were prescribed isotretinoin (Roaccutane), Switzerland, at a standard dose of 10 mg/day for three months.
A study of the content of triglycerides, cholesterol, ALT, AST in the blood serum of observed individuals with acne was carried out before the start of treatment with isotretinoin (Roaccutane), and was also carried out during therapy with “small doses” of the drug once a month for three months. 40 healthy individuals were examined as a control group.
After completing a 3-month course of isotretinoin monotherapy, patients were prospectively monitored for 6 months.
Results and its discussion. In all patients, before treatment, the presence of many miliary and lenticular papules of a conical shape of a bright pink color, pustules with a tense cap, cloudy contents, single nodes of a purplish-bluish color, dense consistency, without signs of fluctuation, associated with an increase in the ADI index to 9, was detected. 7±0.5 (Fig. 1) on the back, chest and face.
By the 7th day from the start of therapy with isotretinoin (Roaccutane), 25 patients (62.5%) registered the development of a peculiar reaction of exacerbation of dermatosis, manifested by the appearance of fresh nodules and miliary pustules on the face and back. However, already on the 14th day of treatment, a clear decrease in the signs of seborrhea was recorded in all patients receiving isotretinoin (Roaccutane). After 3-4 weeks from the start of taking isotretinoin (Roaccutane), a pronounced positive dynamics was noted in the skin pathological process (papules flattened, faded, pustules shriveled into crusts, nodes decreased in size), which was accompanied by a statistically significant decrease in the value of the ADI index to 5. 1±0.1 (p<0.001). By the 2nd month of therapy with isotretinoin (Roaccutane), this indicator decreased to 3.1±0.1 (p<0.001), clinically reflecting the disappearance of comedones, a decrease in the number of papular nodes and the complete disappearance of pustular efflorescence. After 3 months from the start of treatment with isotretinoin (Roaccutane), the vast majority of patients had complete resolution of comedones, papules, and pustules, and the ADI index reached 0.6 ± 0.01 (p < 0.001) (Fig. 1).
Rice. 1. Dynamics of the ADI index in patients with acne who used the “low-dose” isotretinoin (Roaccutane) regimen.
Six months after the start of isotretinoin (Roaccutane) therapy, it was possible to prospectively assess the condition of the skin process in 38 patients (two patients dropped out of the observation group for personal reasons). Thus, in the 36 individuals we observed, there were no signs of seborrhea and acne; the value of the ADI index was zero. Only in two patients were single lenticular pale pink nodular efflorescences recorded on the back against the background of a complete absence of pustules, comedones, nodes and seborrhea (ADI index = 2.4 ± 0.1) (Fig. 1).
It was also found that isotretinoin (Roaccutane) was generally well tolerated by patients, and side effects were minimal in severity and spectrum. Thus, all patients (100%) developed cheilitis on the 7th–14th day of treatment. 18 patients (45%) had retinoid dermatitis of the face, and 22 patients (55%) had dry nasal mucosa. The above-mentioned side effects did not require discontinuation of isotretinoin (Roaccutane) and were easily and quickly relieved by the prescription of moisturizers, in particular the drug Clobeyz.
Upon re-examination, laboratory parameters in all patients (in particular AST, ALT, triglycerides) at the end of the three-month course of isotretinoin (Roaccutane) therapy were comparable to control values. In 2 patients, an increase in the concentration of cholesterol in the blood was noted, but no significant differences were obtained with the control group (p>0.05) (Table 1).
conclusions
1. The use of a mild dosing regimen of isotretinoin (Roaccutane) in patients with moderate to severe forms of acne is very appropriate.
2. The use of small doses of isotretinoin (Roaccutane) allows for rapid and lasting resolution of skin rashes, prevents relapses, minimizes the risk of side effects, and also does not require any additional therapy for both the main disease and side effects identified during treatment. effects.
A.L. Bakulev, S.S. Kravchenya
Saratov State Medical University named after V.I. Razumovsky
Bakulev Andrey Leonidovich - Doctor of Medical Sciences, Professor of the Department of Skin and Venereal Diseases
Literature:
1. Acne. Clinical recommendations of the Russian Society of Dermatovenerologists / ed. A.A. Kubanova. - M.: DEX-Press, 2010. - 28 p.
2. Samtsov A.V. Acne and acneiform dermatoses. - M., 2009. - P. 32-45.
3. Layton AM, Knaggs H, Taylor J et al. Isotretinoin for acne vulgaris - 10 years later: a safe and successful treatment. Br J Dermatol., 1993; 129: 292-296.
4. Goodfield MJ, Cox NH, Bowser A. Advice on the safe introduction and continued use of isotretinoin in acne in the UK 2010. Br J Dermatol., 2010 Jun; 162(6):1172-9.
5. Layton A. The use of isotretinoin in acne. Dermatoendocrinol., 2009, May; 1(3): 162-9.
6. Roodsari MR, Akbari MR, Sarrafirad N. et al. The effect of isotretinoin treatment on plasma homocysteine levels in acne vulgaris. Clin Exp Dermatol. 2010 Aug; 35 (6): 624-6.
7. Li L., Tang L., Baranov E. et al. Selective induction of apoptosis in the hamster flank sebaceous gland organ by a topical liposome 5-alpha-reductase inhibitor: a treatment strategy for acne. J Dermatol., 2010 Feb; 37 (2): 156-62.
8. Sardana K., Garg VK Efficacy of low-dose isotretinoin in acne vulgaris. Indian J Dermatol Venereol Leprol., 2010 Jan-Feb; 76 (1): 7-13.
9. Ingram JR, Grindlay DJ, Williams HC Management of acne vulgaris: an evidence-based update. Clin Exp Dermatol., 2010, Jun; 35(4): 351-4.
10. Merritt B., Burkhart CN, Morrell DS Use of isotretinoin for acne vulgaris. Pediatr Ann., 2009, Jun; 38 (6): 311-20.
11. Bener A., Lestringant GG, Ehlayel MS et al. Treatment outcome of acne vulgaris with oral isotretinoin. J Coll Physicians Surg Pak., 2009, Jan; 19 (1): 49-51.
12. Kontaxakis VP, Skourides D, Ferentinos P et al. Isotretinoin and psychopathology: a review. Ann Gen Psychiatry., 2009, Jan 20; 8:2.
13. Degitz K., Ochsendorf F. Pharmacotherapy of acne. Expert Opin Pharmacother, 2008, Apr; 9 (6): 955-71.
14. O'Reilly K., Bailey SJ, Lane MA Retinoid-mediated regulation of mood: possible cellular mechanisms. Exp Biol Med (Maywood), 2008, Mar; 233(3):251-8.
15. Berbis P. Systemic retinoids (acitretin, isotretinoin). Ann Dermatol Venereol., 2007, Dec; 134 (12): 935-41.
The use of roaccutane for the treatment of acne in cosmetology
Korchevaya T.A.
Acne is a disease of the hair follicles and sebaceous glands. In the pathogenesis of acne, four interrelated factors are important: pathological follicular hyperkeratosis, excessive secretion of the sebaceous glands, proliferation of Propionibactertum acnes (P. acnes) and inflammation. In addition, the nature and volume of secretion of the sebaceous glands is influenced by androgens, which can also play an important role in the pathogenesis of acne.
Excess sebum production plays an additional role in the pathogenesis of acne. In patients suffering from acne, sebum production increases significantly, which usually correlates with the severity of the disease. The secretion of the sebaceous glands is a substrate for the proliferation of P. acnes. In this case, lipolysis of sebum occurs by bacterial lipases to free fatty acids, which in turn contribute to inflammation and the formation of comedones.
In patients with acne, P. acnes multiplies and plays a key role in the inflammatory phase of the disease. When the contents of the follicle enter the skin itself, aseptic inflammation occurs. Depending on the location and extent of inflammation, papules, pustules and cysts are formed.
In connection with the above, for rational treatment of acne, it is important for us to solve the following main tasks:
- reduce the effect of androgens on the sebaceous glands,
- reduce sebum formation,
- reduce inflammation,
- reduce the number of P. acnes,
- normalize the mitotic activity of the skin.
Rational treatment is based on correct clinical assessment. The duration of acne, the maximum severity and location of the lesion should be determined.
Topical treatment alone may be indicated for mild to moderate noninflammatory acne, mild superficial inflammatory acne without scarring, and as an adjunct to oral therapy for moderate to severe acne.
Systemic therapy is necessarily combined with local therapy and is indicated for the treatment of patients with moderate to severe acne, especially in cases of scarring or a tendency to psychosocial disorders.
Currently, Roaccutane is the most effective drug for the treatment of severe forms of acne. Clinical experience shows that it can cause long-term remissions or cures in most patients. Roaccutane reduces sebum production by 80%. There is a significant reduction in comedogenesis and P. acnes counts within 4 to 8 weeks after initiation of treatment.
Roaccutane is teratogenic. When prescribing it to women of childbearing age, it is necessary to exclude pregnancy two weeks before treatment. But the drug does not stay in the tissues for a long time and therefore, 1-2 months after treatment with Roaccutane, pregnancy is not prohibited. The opinion of some gynecologists and a number of other specialists who do not recommend getting pregnant for the entire first year after treatment with Roaccutane is erroneous: the level of the drug in the blood returns to the physiological norm within two weeks after discontinuation of the drug. And for men, in terms of childbearing, it has no contraindications, since it has no effect on sperm.
Economic efficiency. The cost of a course of treatment with Roaccutane is not always clearly perceived not only by the patient, but even by the doctor. But we must remember the high effectiveness of the drug, its surprisingly lasting effect on severe cystic, atheromatous acne, which, unfortunately, has always been considered a chronic recurrent skin disease. And here the doctor is faced with a choice: either he offers the patient treatment for a long time followed by numerous cosmetic procedures to prevent relapse; carry out repeated courses of treatment in case of relapse of inflammation, which, especially in cystic forms, is almost inevitable. With this tactic for treating acne, the total costs of treatment extended over time without the use of Roaccutane will undoubtedly be higher. Doctors are attracted to treatment with Roaccutane, of course, by the result itself: “I receive deep satisfaction from the results of treatment with this drug, as the patient’s skin improves and evens out almost without much effort on the part of the doctor.” Indeed, often even with the most complex cosmetic procedures we cannot achieve the same cosmetic effect on the skin that Roaccutane treatment provides. And most importantly, clinical cure is observed in the vast majority of patients. We understand that investing money in a temporary effect such as we often see from antibiotics for acne would, of course, be inappropriate. Therefore, the patient asks about guarantees. According to various authors, the percentage of effectiveness is very high: from 80% to 95%.
We have noticed that treating foci of chronic infection increases the effectiveness of treatment and reduces the percentage of relapses.
We begin to prepare the patient for taking Roaccutane already at the stage of a standard examination for the drug:
1. Sanitation of foci of chronic infection (gastrointestinal tract, ENT organs, etc.), 2. Sanitation of the skin with concomitant demodicosis: - Delex-acne gel (contains sulfur), - Metrogyl jelly (contains metronidazole).
We believe that it is not always advisable to carry out monotherapy with Roaccutane. To improve skin smoothing, enhance the anti-inflammatory effect, accelerate healing, eliminate post-acne defects in the early stages, when they are more susceptible to influence, we recommend combining Roaccutane at different stages of treatment with a number of medications and cosmetic procedures:
- vitamin E (taken orally in a prophylactic dosage),
- homeopathy and antihomotoxicology,
- Skinoren,
- oxygen ozone therapy,
- mesotherapy,
- myostimulation,
- enzymatic peeling (to remove possible peeling of facial skin),
- diathermocoagulation of abscesses,
- massotherapy.
Among antihomotoxic drugs, I would like to especially highlight the use of Traumeel in complex therapy with Roaccutane.
The use of Traumeel S and Roaccutane in the treatment of severe forms of acne (240 patients)
| Roaccutane | Roaccutane and Traumeel S | |
| Stopping new items from appearing | 5-8 weeks | After 2-4 weeks |
| Duration of treatment | 12-16 weeks | After 10-12 weeks |
| Anti-scarring effect | Moderate | Expressed |
The table shows that when Roaccutane is combined with the antihomotoxic drug Traumeel, the effect of treatment occurs much earlier and the smoothing of scars is more pronounced.
Unfortunately, Roaccutane does not combine well with liquid nitrogen, cosmetic cleansing, dermabrasion, chemical and acid peels. After completion of treatment with this drug for different periods of 3 months. up to 6 months if necessary, chemical and acid peeling and dermabrasion can be performed. Cosmetic cleansing - earlier: after 1-2 weeks, and with small dosages - at the end of the Roaccutane course.
Conclusion.
Roaccutane acts on the most important mechanism of acne - increased sebum secretion. Gradually, the sebaceous glands decrease in size, sebaceous cysts disappear, and therefore, inflammation in the area of these glands decreases. It is with the restructuring of the sebaceous glands that a lasting effect or clinical recovery is associated with treatment with Roaccutane.
It is possible to combine Roaccutane at different stages of treatment with anti-scarring and anti-inflammatory homeopathy, as well as with a number of cosmetic procedures.
Roaccutane®
Pregnancy is an absolute contraindication for therapy with Roaccutane®. If pregnancy occurs, despite warnings, during treatment or within a month after the end of therapy, there is a very high risk of giving birth to a child with severe malformations.
Isotretinoin is a drug with a strong teratogenic effect. If pregnancy occurs during a period when a woman takes isotretinoin orally (at any dose and even for a short time), there is a very high risk of giving birth to a child with developmental defects.
Roaccutane® is contraindicated in women of childbearing potential unless the woman's condition meets all of the following criteria:
- she must have severe acne that is resistant to conventional treatments;
- she must accurately understand and follow the doctor’s instructions;
- she must be informed by the doctor about the danger of pregnancy during treatment with Roaccutane® within one month after it and urgent consultation if pregnancy is suspected;
- she should be warned about the possible ineffectiveness of contraceptives;
— she must confirm that she understands the essence of the precautionary measures;
- she must understand the need and continuously use effective methods of contraception for one month before treatment with Roaccutane®, during treatment and for a month after its completion (see section “Interaction with other drugs”); it is advisable to use 2 different methods of contraception at the same time, including barrier;
- she must have received a negative result from a reliable pregnancy test within 11 days before starting the drug; A pregnancy test is strongly recommended monthly during treatment and 5 weeks after the end of therapy;
- she should start treatment with Roaccutane® only on the 2-3 day of the next normal menstrual cycle;
- she must understand the need for mandatory visits to the doctor every month;
- when being treated for a relapse of the disease, she must constantly use the same effective methods of contraception for one month before starting treatment with Roaccutane®, during treatment and for a month after its completion, as well as undergo the same reliable pregnancy test;
- She must fully understand the need for precautions and confirm her understanding and desire to use reliable methods of contraception as explained to her by the doctor.
Use of contraception as directed above during treatment with isotretinoin should be recommended even in women who do not routinely use contraception due to infertility (except in patients who have had a hysterectomy), amenorrhea, or who report not being sexually active.
The doctor must be sure that:
— the patient has a severe form of acne (nodulocystic, conglobate acne or acne with a risk of scarring); acne that does not respond to other types of therapy;
- a negative result from a reliable pregnancy test was obtained before starting the drug, during therapy and 5 weeks after the end of therapy; the dates and results of the pregnancy test must be documented;
- the patient uses at least 1, preferably 2 effective methods of contraception, including a barrier method, for one month before starting treatment with Roaccutane®, during treatment and for a month after its completion;
— the patient is able to understand and fulfill all of the above requirements for pregnancy protection;
— the patient meets all of the above conditions.
Pregnancy test
According to current practice, a pregnancy test with a minimum sensitivity of 25 mIU/ml should be performed in the first 3 days of the menstrual cycle:
Before starting therapy:
— To exclude possible pregnancy, before starting contraception, the result and date of the initial pregnancy test must be recorded by a doctor. In patients with irregular menstruation, the timing of a pregnancy test depends on sexual activity and should be performed 3 weeks after unprotected intercourse. The doctor should inform the patient about contraceptive methods.
— A pregnancy test is carried out on the day of prescription of the drug Roaccutane® or 3 days before the patient’s visit to the doctor. The specialist should record the test results. The drug can only be prescribed to patients receiving effective contraception for at least 1 month before starting therapy with Roaccutane®.
During therapy:
— The patient must visit the doctor every 28 days. The need for monthly pregnancy testing is determined in accordance with local practice and taking into account sexual activity and previous menstrual irregularities. If indicated, a pregnancy test is performed on the day of the visit or three days before the visit to the doctor, the test results must be recorded.
End of therapy:
- 5 weeks after the end of therapy, a test is performed to exclude pregnancy.
A prescription for Roaccutane® for a woman capable of childbearing can be issued only for 30 days of treatment; continuation of therapy requires a new prescription of the drug by a doctor. It is recommended that a pregnancy test, writing a prescription and receiving the drug be carried out on the same day.
The drug Roaccutane® should be dispensed at the pharmacy only within 7 days from the date of issuing the prescription.
To help physicians, pharmacists and patients avoid the risk of fetal exposure to Roaccutane®, the company aims to warn about the drug's teratogenicity and emphasize the absolute mandatory use of reliable contraceptive measures for women of childbearing age. The program contains the following materials:
for doctors:
— a doctor’s guide to prescribing Roaccutane® to women
— informed consent form for the patient
— form for recording the prescription of the drug to women for the patient:
— patient information brochure
- what you need to know about contraception
— for the pharmacist:
— a guide for the pharmacist on the dispensing of the drug Roaccutane®.
Full information about teratogenic risk and strict adherence to measures to prevent pregnancy should be provided to both men and women.
For male patients
Existing data indicate that in women, exposure to the drug from the semen and seminal fluid of men taking Roaccutane® is not sufficient to cause the teratogenic effects of Roaccutane®.
Men should exclude the possibility of other persons, especially women, taking the drug.
If, despite the precautions taken, pregnancy does occur during treatment with Roaccutane® or within a month after its end, there is a high risk of very severe fetal malformations (in particular, from the central nervous system, heart and large blood vessels) . In addition, the risk of spontaneous miscarriage increases.
If pregnancy occurs, therapy with Roaccutane® is discontinued. The advisability of maintaining it should be discussed with a doctor specializing in teratology. Severe congenital malformations of the fetus in humans associated with the use of Roaccutane® have been documented, including hydrocephalus, microcephaly, cerebellar malformations, anomalies of the external ear (microtia, narrowing or absence of the external auditory canal), microphthalmia, cardiovascular anomalies (tetrad Fallot, transposition of the great vessels, septal defects), malformations of the face (cleft palate), thymus gland, pathology of the parathyroid glands. Because isotretinoin is highly lipophilic, it is very likely that it passes into breast milk. Due to possible side effects, Roaccutane® should not be prescribed to nursing mothers.
Retinoids (in-depth review)
Acnecutane, Roaccutane, Erase
Acnecutane, Roaccutane, Erase
Systemic retinoids contain the active ingredient isotretinoin. This substance has been used in world medicine for almost 40 years and is the gold standard for the treatment of acne and acne.
What kind of substance is this? This is trans-retinoic acid and it very powerfully suppresses the activity of the sebaceous glands.
When does acne occur?
Acne occurs when, under the influence of excessive effects of the hormone testosterone on the sebaceous gland, powerful production of sebum in large quantities is stimulated.
How do systemic retinoids work?
Systemic retinoids act on the sebaceous gland receptors, joining the sebaceous gland receptors, they inhibit the activity of sebum secretion from the gland and acne goes away.
The most frequently prescribed drugs from systemic retinoids (approved in the Russian Federation):
- Roaccutane
- Aknekutan
- Will erase
Comment from cosmetologist, dermatologist Yuliana Shiyan:
When I prescribe one of these drugs, I am asked why this particular drug and what is the difference between retinoids? All these drugs have one substance in common: Isotretinoin. Roaccutane was the very first to appear. This is the original drug, and all other drugs are its *generics. All generics of isotretinoin have their own registration certificates and are approved in Russia.
*GENERIC - approved copy of the original drug
Roaccutane and Sotret practically do not differ from each other either in formula or dose. When assigning them, there is no difference and the choice in favor of one or the other is immaterial. Acnecutane contains the same substance, but its formula is slightly different from Roaccutane and Sotret.
Why is Acnecutane more interesting for a cosmetologist and the patient himself, as a choice for treatment and how to understand which retinoid drug is better?
Isotretinoin is a fat-soluble substance. It is absorbed by the body only in combination with absorbed fats. If you take Roaccutane and wash it down with plain water, you will absorb less than 40% of it. If you take Acnecutan and drink it with plain water, it will be absorbed by the body by about 70%.
When prescribing Acnecutane, the doctor insures patients against their own mistakes. Patients may neglect fatty foods while taking Roaccutane and Sotret, forget to eat anything fatty or fatty foods are forbidden to them (on a diet), and the required dose of the drug must enter the body! Necessary, not a small part of it! Therefore, the drug Acnekutan is more preferable for the patient; a lack of fat when taking it is less likely to affect the outcome of treatment.
Its daily dose is regulated by the doctor, but there is also a cumulative dosage of the drug that the patient’s body must accumulate. It is when it is achieved that we can talk about a high chance of stable remission in the patient.
Due to the fact that Acnecutane is better absorbed, the manufacturer made slightly less active ingredient in one dose, which means: The working dose is 20 mg. Roaccutane corresponds to the working dose of Acnecutane with 16 milligrams of Isotretinoin.
The conclusion is simple: if less isotretinoin accumulates in the body, then the risks of side effects are also reduced. This is very good for the patient!
For ardent supporters of all original and original drugs, Roaccutane is recommended. But all other retinoids will be useful for you, provided that they are prescribed by a dermatologist, and you, in turn, comply with all the conditions for taking retinoids.