Polyp
is a pathological proliferation of the mucous membrane. By its nature, this is a benign formation, however, there is a risk of the polyp degenerating into a malignant tumor.
The mucous membrane lines the inside of the hollow organs of those systems of our body that communicate with the external environment, in particular the respiratory, urinary, reproductive and digestive systems. The functions of the mucous membrane are varied - this includes a protective function, absorption (typical of the gastrointestinal tract), hydration, and some others.
As a result of various reasons, the mucous membrane may become weakened, and then it begins to grow. So the body tries to compensate for the loss of properties of the mucous membrane by increasing its area. The result is a polyp that looks like a mushroom-shaped body on a stalk or on a thick base. Polyps can be either single or multiple (in this case the disease is called polyposis
).
Causes of appearance and main symptoms
For clarity, we will place information about the causes and symptoms of the disease in a table.
| Causes of polyps in the nasal cavity | Symptoms of the disease | Risk group |
|
| Children under the age of 10 years (it is in them that this disease most often occurs). |
Nasal polyps can cause a lot of inconvenience to a person, but the main danger is that benign formations can transform into malignant ones.
They are characterized by gradual growth, so if you do not seek help immediately, polyps can close the entire nasal passage. This is the main reason why nasal polyps need timely treatment.
Surgical intervention is a last resort measure to get rid of the disease, but we will tell you about alternative ways to solve the problem.
Nasal polyps: diagnosis
When examined by an ENT doctor, nasal polyps can be identified visually.
Additional methods, such as computed tomography, provide additional information about the extent of the pathological process. Examination by an ENT doctor.
First, the specialist asks about the patient’s complaints and previous diseases (allergies, sinusitis, etc.). Symptoms such as problems with nasal breathing, impaired sense of smell or frequent sinusitis already raise suspicions about polyposis rhinosinusitis.
Then the doctor carefully examines the ENT organs. Large nasal polyps that protrude into the nasal cavity may already be visible to the naked eye. With the help of speculums and a nasal endoscope, the doctor often finds smaller polyps located more deeply.
Radiation diagnostics.
To obtain accuracy in diagnosis, it is necessary to understand the extent of the spread of polyps in the paranasal region; imaging methods, in particular computed tomography (CT), are suitable for this purpose. Conventional x-rays of the sinuses are considered obsolete. Ultrasound and MRI can be used in the diagnosis of nasal polyps only in rare cases.
Polyps in a child
The incidence of such diseases as nasal polyps in children is quite high. And it is detected late in children, since at the beginning of its development it does not have obvious and specific symptoms. A number of symptoms that may indicate nasal polyps:
- headache (other causes of headache are described here);
- snore;
- insomnia;
- frequent sneezing;
- smell dysfunction;
- nasal congestion;
- frequent tonsillitis and adenoids;
- voice change;
- pain and sensation of a foreign object in the nose;
- hearing loss.
There are no specific reasons for the formation of nasal polyps in a child, but there are conditions that precede their development: chronic sinusitis or rhinitis, allergic rhinitis, hereditary and congenital predisposition, cystic fibrosis. To establish a diagnosis, the doctor performs rhinoscopy, and tomography to determine the degree of prevalence.
Is it possible to get rid of polyposis using folk remedies?
The opinion of experts regarding traditional treatment is that it can be complementary to the main treatment program.
At the initial stages of pathology development, the use of folk recipes can be effective. Traditional medicine recipes should be used after consultation with your doctor.
Often the cause of polyposis is an allergy, and herbal remedies can also cause this phenomenon. Careless use of such medications may not only not help, but also cause harm. Usually a test is done on the elbow for a possible reaction.
Traditional medicine recipes for polyps often influence the cause of polyps in their action. Therefore, if you follow the dosages and do the procedures persistently, adhering to the dosage schedule, you can achieve positive results.
Photo: what polyps look like in adults and children
To help the doctor understand what the patient’s polyps look like and how much they have grown, Hartman mirrors are used.
During rhinoscopy, the specialist sees formations in the nose with a smooth surface of a yellow or transparent color, on a stalk. Possible discharge of pus.
What nasal polyps look like in children - the photo is presented below. When examined without tools and apparatus:
What nasal polyps look like in adults - the photo is presented below:
What does a polyp look like from the inside:
Possible complications
Constant disruption of nasal breathing causes the development of hypoxia, which has a bad effect on the body as a whole. This condition is especially dangerous for the development of children. Nasal congestion leads to psychological problems. Symptoms of sinus polyposis often cause poor mood and increased irritability in adults and children. Advanced stages of the pathology cause resorption of the bone structures and cartilage of the nasal septum and the walls of the paranasal sinuses. If polyps grow into the nasolacrimal duct, constant lacrimation appears.
Treatment of polyps without surgery
The tricky thing about polyps is that they can grow. Conservative treatment is appropriate only at the initial stage of the disease; in advanced stages, growths must be removed.
Hormone therapy
This type of conservative disposal of polyps involves:
- injection into the body of the neoplasm;
- use of nasal hormonal sprays;
- taking corticosteroids in tablet form.
The term “corticosteroids” refers to medications containing hormonal substances.
Selecting material for injection into a polyp is a scrupulous process that depends on numerous nuances. The principle of this therapy is that the injected drug destroys the polyp cells, which are then removed from the nose with mucus when blowing the nose.
A one-time procedure includes 2 injections. The break between procedures is 2 weeks.
The most commonly prescribed corticosteroid sprays include:
- "Aldecin";
- "Nasobek";
- “Fluticasone”, “Flixonase”, “Avamys” and “Nazarel” - a group of medications containing the active ingredient Fluticasone;
- "Nasonex" (can be prescribed to children aged 2 years and older).
The last corticosteroid drug worth mentioning is Prednisolone . It is taken orally. In the first week, the daily dose of medication for an adult is 30-60 mg, in the next 3 weeks the dose is gradually reduced.
All medications containing hormonal substances, regardless of the method of administration (orally, by injection or in the form of sprays), have the same effect. Unfortunately, in quantitative terms, the list of negative consequences of taking corticosteroids exceeds the beneficial properties of drugs.
| The benefits of hormonal medications in the fight against nasal polyps | Side effects of hormonal drugs |
|
|
Hormone therapy does not guarantee getting rid of benign tumors. Having disappeared, polyps can reappear in the nasal cavity after some period of time. This happens when the cause of their initial appearance is not identified and eliminated.
Allergy treatment
The occurrence of nasal polyps is often associated with an allergy to a particular substance.
In this case, therapy consists of 2 stages:
- identification of allergens;
- prescription of antihistamines.
If tests show that the allergen is a substance contained in the food, it is necessary to create a special diet.
When prescribing treatment, experts give preference to modern antihistamines , which have a minimum of side effects. Let's list some of them:
- "Levocetirizine";
- "Cetirizine";
- "Erius";
- "Loratadine."
Relief from chronic sinusitis
If chronic sinusitis is the cause of the appearance of a neoplasm, getting rid of it leads to healing from polyps.
In the context of the task at hand, for the treatment of sinusitis, the doctor prescribes:
- antibiotics;
- anti-inflammatory drugs;
- means for auxiliary therapy.
Due to the fact that the list of prescribed drugs is very large, we will place the necessary information in the table.
| Antibiotics | Anti-inflammatory medications | Adjuvant therapy drugs |
|
|
|
Physiotherapeutic procedures
Possible procedures:
- salt inhalations,
- acupuncture,
- ozone-ultraviolet sanitation,
- excision of polyps using laser coagulation (this procedure is performed on an outpatient basis).
Nasal polyps: causes
What causes nasal polyps is not known. But the main risk factors are allergies and chronic rhinosinusitis.
The nasal cavity and paranasal sinuses have a complex self-cleaning mechanism. The cells of the mucous membrane form a thin film of secretion, into which pathogens (viruses, allergens, dust particles) enter from the inhaled air. As a result, the air entering the lungs is purified and moisturized. The cells contain movable hairs (cilia), which transport secretions from the sinuses continuously to the posterior sections of the nasal cavity, from there to the nasopharynx, pharynx, and eventually this mucus enters the acidic environment of the stomach.
Impaired outflow of mucus from the sinuses.
The paranasal sinuses are connected to the nasal cavity through narrow “channels” of the anastomosis. Deviation of the nasal septum and other anatomical features can lead to a narrowing of these “channels”. As a result, discharge accumulates in the sinus cavity and provides ideal soil for the proliferation of pathogenic microorganisms.
Due to frequent infections, the mucous membrane is constantly irritated and swollen - which further aggravates the situation. Polyps may form, which, in turn, further block the outflow from the sinus.
Allergies are a possible precursor to nasal polyps.
Allergies contribute to prolonged irritation and swelling of the mucous membrane in the nasal cavity and sinuses, which can lead to the formation of polyps. Many patients with nasal polyposis simultaneously suffer from various forms of allergies. Even patients without allergies who constantly inhale too dry or polluted air have an increased risk of developing polyps.
Frequent combination: intolerance to analgesics, asthma, polyps (aspirin triad).
People with bronchial asthma are prone to developing nasal polyps, as well as people who cannot tolerate analgesics, specifically non-steroidal anti-inflammatory drugs (NSAIDs). Patients with such NSAID intolerance suffer from asthma attacks as soon as they take certain medications - for example, acetylsalicylic acid (aspirin), ibuprofen, diclofenac, analgin. This is a so-called “pseudo-allergy”; the body does not form specific antibodies against drugs, as with a real allergy.
The combination of NSAID intolerance, nasal polyps and asthma is also called: Samter's triad, Fernand-Vidal triad.
Cystic fibrosis.
Nasal polyps are rare in children—with one exception: About one-third of all children with the congenital metabolic condition cystic fibrosis also develop nasal polyps. With this pathology, the glands secrete an abnormally viscous secretion, which accumulates in the sinuses, which contributes to chronic sinusitis and, consequently, nasal polyps.
A rare cause is primary ciliary dyskinesia.
This is a congenital pathology, which is manifested by underdevelopment of the “cilia” and can manifest itself as frequent respiratory diseases and persistent nasal congestion.
You should be aware that long-term use of vasoconstrictor nasal sprays can affect cilia function in a similar way.
ethnoscience
The most famous methods:
- treatment with celandine juice,
- rinsing the nasal passages with herbal decoctions,
- putting essential oils into the nose.
celandine juice yourself. The plant, dug up along with its roots in May, is washed, put through a meat grinder and infused for a week. After this time, it begins to ferment (a sure sign that the drug is ready). The juice is diluted with water in a 1:1 ratio.
Instill 2 drops into the nostril every morning (regardless of the location of the polyp, both nostrils are subjected to the procedure). The full cycle consists of 5 courses, each of which lasts one week. There is a 10 day break between courses.
Treatment with essential oils lasts even longer: for 6 months, 2 drops of oil from one of the plants are instilled into the nostrils twice a day:
- St. John's wort,
- wild rosemary,
- thuja occidentalis.
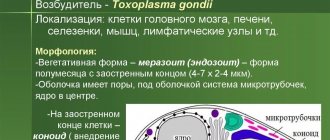
Chronic rhinosinusitis (CR) is one of the most common and controversial diseases in the practice of otolaryngologists, many aspects of its pathogenesis, and therefore adequate treatment, are under study [1, 2]. Currently, large-scale consensus documents have been created - EPOS-2005, -2007 and -2012, which analyze the entire world experience in diagnosing and treating this condition [3, 4]. As a result of the analysis, experts propose a simple classification scheme for chronic disease: chronic disease with polyposis and chronic disease without polyposis.
In Russia, the term “polypous rhinosinusitis” is more often used, which also reflects the involvement in the pathological process of not only the paranasal sinuses, but also the nasal cavity. This, in turn, makes it somewhat difficult to make a diagnosis using the ICD-10 system, since the doctor has to make a choice between the diagnosis of “polyposis sinus degeneration” and “nasal polyps.” The ambiguity of the etiopathogenesis, as well as terminological paradoxes, currently determine the absence of an ideal method of treating polyposis rhinosinusitis with an anti-relapse guarantee [4, 5].
Despite the rapid development of endoscopic technology and the popularization of functional endoscopic sinus surgery, a decrease in the number of such patients has not been observed. Radical surgery on the maxillary sinuses in combination with total ethmoidectomy also does not guarantee the absence of relapse, and the significant traumatic nature of the intervention causes a long recovery period with the development of postoperative sinus disease, the need for long-term antibacterial therapy, and frequent visits to an otolaryngologist [4].
Many authors note that the causes of the polypous process in the paranasal sinuses are different. In this regard, the tactics of treating polyposis sinusitis should have a differentiated approach, since there are a sufficient number of conservative methods of treating such patients, which in some cases can effectively combat this disease [5].
The basis of drug therapy for long-term control of the inflammatory process in the nasal cavity is intranasal glucocorticosteroids (ICS) or topical GCS for intranasal use. The creation of the GCS can be called one of the key scientific achievements of the middle of the last century. However, since initially only systemic drugs existed, their use was accompanied by severe side effects from Itsenko-Cushing syndrome to systemic osteoporosis. With the advent of topical forms 30 years later, this problem was solved, since even the use of high doses of these drugs was not accompanied by significant systemic absorption [6].
The first topical GCS was beclomethasone dipropionate, which successfully proved itself in a group of patients with allergic rhinitis and later bronchial asthma. Subsequently, other topical corticosteroids were created, the molecules of which were characterized by improved pharmacological properties, and clinical experience in their use was also accumulated [6].
The anti-inflammatory effect of topical corticosteroids is associated with inhibition of inflammatory mediators, including the production of cytokines; interference with the metabolism of arachidonic acid; thus leading to the stabilization of cell membranes, a decrease in vascular permeability, and an improvement in the function of cellular receptors [6].
Currently, among the topical corticosteroids, the most studied and widespread in ENT practice are beclomethasone dipropionate, budesonide, fluticasone propionate, fluticasone furoate and mometasone furoate.
The effectiveness of ICS in the treatment of patients with polypous rhinosinusitis is regularly reviewed in EPOS documents. To date, the 3rd edition of this document has already been published - EPOS-2012, which is a detailed analysis of all aspects of rhinosinusitis in general, performed by a group of experts using modern principles of evidence-based data [4]. The document also discusses a number of positions regarding ICS, which often cause the greatest controversy among practical otolaryngologists, namely:
- effectiveness of ICS monotherapy for polypous rhinosinusitis;
- effectiveness of the ICS + surgical treatment regimen;
- when ICS are more effective before and/or after surgical treatment;
- what is the most effective method of delivering ICS – drops or spray;
- what is the duration of ICS prescription?
Unfortunately, not all of these issues can be answered with an unambiguous recommendation in this document, which is due to the fact that not all analyzed studies could be included in the meta-analysis due to their quality, however, a number of problematic issues in EPOS-2012 are covered in sufficient detail.
ICS and surgical treatment
In general, the improvement of nasal breathing using the scheme of surgical treatment + subsequent use of ICS was more effective than in the case of ICS monotherapy, but statistical significance of the results in general was not achieved.
Drops or spray
A number of GCS available on the Russian pharmaceutical market for intranasal use are presented in the form of nasal drops. In this regard, EPOS-2012 emphasized the advantage of ICS in the form of nasal aerosols (sprays), which were recognized as more effective in reducing the symptoms of polyposis rhinosinusitis, however, the objective reduction of polyposis tissue when compared between two options for delivering GCS (drops or spray) was not statistically significant, which experts attribute to the insufficient quality of available studies to be included in the meta-analysis.
“Old” generations of ICS versus “new” ones
According to a meta-analysis of studies available in the literature, experts found that there is no significant difference in the effectiveness of “new” or “modern” generations of ICS (mometasone furoate, fluticasone dipropionate) compared to the “old” ones, which, of course, is interesting with from the point of view of the economic component - it is no secret that drugs based on the “old” generations of GCS are significantly cheaper than the “new” ones.
In general, according to EPOS-2012, the proportion of studies confirming the effectiveness of ICS for polypous rhinosinusitis is significantly greater than those that do not confirm their effectiveness or indicate a placebo advantage (see table) [4].
If we consider the problem of choosing ICS from a pharmacological point of view, then their comparison is possible according to a number of parameters, one of which is the therapeutic index, which is the ratio of the average lethal dose to the dose that causes a therapeutic effect in 50% of experimental animals. This indicator is the highest for budesonide, which is due to the high affinity of the drug for glucocorticoid receptors and accelerated metabolism after systemic absorption [7, 8].
In addition, important characteristics of topical corticosteroids (which distinguish them from systemic ones) include lipophilicity and a short half-life from blood plasma. These properties also have certain differences depending on the drug. Thus, compared to fluticasone propionate/furoate and mometasone furoate, budesonide is less lipophilic, which allows it to penetrate the mucus layer covering the mucous membrane more quickly and more effectively. Presumably, this property is responsible for the greater effectiveness of budesonide compared to the listed ICS when used in the form of aqueous suspensions for allergic rhinitis [9–11].
Once inside the cell, budesonide forms esters with long-chain fatty acids and remains in the tissues for a long time. It was found that when it enters the upper respiratory tract, at least 70% of budesonide is esterified, while its esters are not detected in plasma [9–11].
Esterified budesonide deposited in tissues, when the concentration of its free form in cells decreases with the participation of intracellular lipases, is able to be released from esters and bind to the GC receptor. A similar mechanism, not characteristic of other corticosteroids, contributes to the prolongation of the anti-inflammatory effect (up to 24 hours) and, as a number of authors believe, is a more important property than receptor affinity, however, in terms of the latter indicator, budesonide is superior to a number of “old” drugs - beclomethasone dipropionate , flunisolide triamcinolone, and is comparable to the activity of fluticasone propionate/furoate [12].
One of the topics discussed in the literature and the main cause of concern for patients when prescribing ICS is concerns about the possible systemic effects of these drugs. If we talk about this topic from a pharmacological standpoint, then to determine the systemic activity of ICS it is necessary to analyze their systemic bioavailability, lipophilicity, volume of distribution, and degree of binding to blood proteins [13].
The total systemic bioavailability of ICS is determined by the fraction of the drug that enters the systemic circulation from the mucosal surface and the portion of the ingested fraction that was not metabolized during the first passage through the liver (oral bioavailability). Moreover, budesonide is one of the IHSCs with the lowest oral bioavailability [12, 14].
Other properties that determine the safety of budesonide are intermediate lipophilicity, which has already been discussed above, and a relatively small volume of distribution compared to beclomethasone dipropionate and fluticasone propionate/furoate. High lipophilicity corresponds to a larger volume of distribution, better penetration into tissues and cells, and a longer half-life. In general, these drugs will be clinically more effective, but the risk of systemic side effects increases [15].
Another property that provides budesonide with low systemic activity is the degree of binding to plasma proteins, which does not differ from that of beclomethasone dipropionate, fluticasone propionate/furoate and mometasone furoate, but in combination with a shorter half-life significantly reduces its potential systemic activity [ 12].
Officially, budesonide for intranasal use is approved for children from 6 years of age, although there are separate studies of younger children. Thus, in a double-blind, randomized, placebo-controlled, prospective study by KT Kim (2004) involving 78 children 2–3 years old, intranasal use of budesonide for 6 weeks was not accompanied by an increase in plasma cortisol levels [16].
It should also be noted that budesonide is the only drug among topical corticosteroids that has the best safety rating during pregnancy (B) according to the FDA (US Food and Drug Administration) classification [17]. This position was based on an analysis of 3 Swedish registries from 1995 to 2001, which recorded no increased risk of late toxicosis of pregnancy, preterm birth, fetal malnutrition and congenital malformations in 2000 newborns whose mothers used inhaled budesonide during pregnancy [15, 16, 18, 19].
Thus, budesonide combines all the necessary properties of intranasal GCS that ensure the clinical effectiveness of this class of drugs: high corticosteroid activity, long-lasting action and low systemic bioavailability.
The effectiveness of non-surgical treatment
The presented material allows us to conclude that the effectiveness of polyp treatment directly depends on the accurate diagnosis of the cause of its appearance. Eliminating the root cause increases the guarantee of lifelong freedom from unwanted growth.
The fastest non-surgical method of getting rid of a nasal polyp is laser coagulation.
In terms of the degree of destructive impact on nasal tumors, traditional medicine lags many times behind other methods. The optimal area of its application is the prevention of growths.
The decision on the choice of therapy to get rid of nasal polyps should be made only by a doctor.
Nasal polyps have terrible consequences, which is why the appearance of one or more symptoms of this disease is an urgent reason to consult a specialist.
Rhinoscopy, CT, pharyngoscopy - this is an incomplete list of procedures that allow the doctor to find the right solution for getting rid of nasal polyps.
If there are no indications for surgical intervention, based on the individual characteristics of the patient, the doctor will choose the most appropriate method of treating nasal polyps without surgery and, if necessary, select auxiliary therapy drugs.
Preventive actions
To prevent the occurrence of nasal polyposis and paranasal sinuses, it is recommended to prevent this condition: Treat infectious diseases in a timely manner. If nasal breathing problems occur, immediately contact an otolaryngologist. If bronchial asthma develops, be constantly monitored by an otolaryngologist and an allergist. Prevent relapses of surgical treatment. For this purpose, irrigation therapy and conservative treatment are used. Nasal polyposis is a fairly common disease that leads to chronic impairment of nasal breathing, which significantly reduces the quality of life of adults and children. To get rid of this problem, you need to promptly consult a doctor who will make a diagnosis and select effective treatment. Typically, surgery helps eliminate the symptoms of polyposis, and postoperative monitoring and therapy help prevent relapses of the disease.
How to remove nasal polyps: surgical methods
1. Laser polypectomy
The method of removing nasal polyps with a laser has some distinctive features - safety and quick implementation.
Many people have no idea how a doctor removes polyps with a laser, but the method is quite simple: using a laser device and an endoscope, pathological areas are cauterized. The result is achieved after the first session, sometimes the procedure is repeated after a week, an excellent option for treating nasal polyps without pain. After laser removal, free breathing is restored, health changes for the better, and the risk of bleeding and scarring is small.
The cost of treatment varies from 7,000 to 30,000, and the price of laser removal depends on the severity and severity of the disease and the number of surgical interventions.
2. One of the cheapest and first ways to remove nasal polyps is surgical polypotomy. When performing the manipulation, the surgeon uses a special instrument, at the end of which there is a small closed loop. Under local anesthesia, the specialist carefully inserts the instrument into the nasal passage without damaging the polyp and places a loop around its stem. Afterwards the loop is tightened and the polyp is excised.
Unfortunately, the manipulation is quite traumatic - scarring and bleeding are inevitable. Recurrence is also common with the described method. The only advantage is the possibility of free removal upon referral from a local physician.
3. Endoscopic removal
It is distinguished by the possibility of excision of formations in the cavity of the nasal sinuses. Even polyps located in groups can be removed endoscopically. It is characterized by careful removal, leaving no scars and reducing the risk of recurrence. The postoperative period is short. The price is no more than 10,000 rubles.
For more information about the causes of polyps and their treatment, watch the video:
This article has been verified by a current qualified physician, the Site Administrator, and can be considered a reliable source of information for site users.
Rate how helpful this article was
4.4 46 people voted, average rating 4.4
Did you like the article? Save it to your wall so you don’t lose it!
Treatment with hydrogen peroxide for sore throat
Treatment of sore throat consists of taking antibacterial agents; rinsing with hydrogen peroxide for sore throat is only an addition. This remedy is effective for cleansing plaque from tonsils.
So, how to gargle with hydrogen peroxide for a sore throat? Gargle only with hydrogen peroxide diluted in water. The solution is prepared as follows:
- Add a tablespoon of 3% peroxide to 100 ml of water.
- Second option: dissolve 1 tablet of hydroperite in 200 ml of water (this is hydrogen peroxide in dry form, in tablets).
You need to gargle 4-5 times a day with a break of more than 3 hours. After the procedure, the mouth and tonsils are washed, using another rinse: plain warm water, soda solution, sage decoction, chamomile flower tincture and others.
Symptoms of nasal polyposis
The appearance of polyps very often cannot be detected without examination by a doctor. The signs of this disease can be easily confused with ordinary rhinitis. The growth of the mucous membrane is accompanied by a feeling of congestion and a decrease in the function of smell. The sick person has to breathe through the mouth because the airways are blocked.
Due to the impossibility of normal nasal breathing, the mucous membrane of the larynx dries out. A dry, hacking cough may appear. When polyps grow towards the auditory canals, hearing impairment and speech distortion in adults may occur. Young children may develop an abnormal bite.