A polyp is an elevation above the level of the mucous membrane of a hollow organ. This is a benign neoplasm that has a different histological structure. Adenomous polyps of the rectum are associated with a high risk of developing a malignant tumor. They are considered precancerous conditions. It is likely that they will develop into colorectal cancer. For this reason, when an adenomatous polyp of the rectum is identified, proctologists at the Yusupov Hospital offer the patient to remove it.
Doctors at the proctology department are fluent in all methods of surgical interventions on the rectum. Surgeons masterfully perform endoscopic and abdominal operations. Patients undergo a comprehensive preoperative examination, which allows us to identify all contraindications to the operation and avoid complications. Sometimes proctologists perform surgery after the patient has been cured of concomitant pathology.
Why are endometrial polyps dangerous?
In this article we will look at the two most commonly diagnosed forms of the disease: adenomatous polyp and glandular polyp, presented in the form of glands and stromas.
The appearance of any polyps is considered to be a disease that should be treated, especially if the growth becomes permanent and widespread. Even if the neoplasms are benign, this condition is diagnosed as precancerous. For women who are still planning to have children, this disease is especially dangerous, as it often leads to infertility.
- Adenomatous polyp.
It is a type of adenoma that manifests itself in the proliferation of endometrial tissue. The endometrium is the mucous membrane that covers the inner surface of the uterus (during menstruation, the functional layers of the endometrium come out in the form of bloody clots that are dark in color).
Adenoma is essentially a benign tumor, and it appears only in organs that have glandular epithelium. The danger of not treating it is as follows: in most cases, this disease leads the patient to oncology - cancer; this risk increases if you do not consult a specialist in a timely manner. An adenomatous polyp can appear on other organs, but its occurrence in the uterine cavity is most dangerous for a woman’s life.
- Glandular polyp.
Already from the name itself you can understand that this type of polyp is formed from glands and endometrial tissue. These polyps are recognized as the smallest and safest among similar neoplasms. The diameter of a glandular polyp can only rarely exceed 1.5 cm.
Such formations are almost never malignant, although medicine knows of cases where endometrial cancer developed due to glandular polyps. In some cases, the lumen of the glands forms cysts, then we are talking about a glandular-cystic polyp. Glandular cystic polyp is not a separate type. Typically, such polyps appear in the form of a node and are located in the stroma of the mucous membrane, which, in turn, is located in the places where the fallopian tubes drain.
Colon
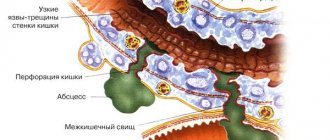
The large intestine is the next section of the gastrointestinal tract after the small intestine and is divided into the cecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. The length of the colon is 1.5-2 m, the diameter is 4-6 cm. The wall of the colon is represented by longitudinal muscle fibers, which are concentrated in the form of three ribbons parallel to each other. The width of each of them is about 1 cm. They stretch from the origin of the appendix in the cecum to the initial part of the rectum. The intestine seems to be corrugated, forming protrusions - haustra. The inner (circular) muscle layer is continuous. The mucous membrane of the colon, unlike the small intestine, does not have villi. The submucosa is represented by loose connective tissue containing the bulk of the vessels. The ascending colon in the right hypochondrium forms a hepatic flexure and passes into the transverse colon, the length of which is 50-60 cm. In the left hypochondrium, the intestine forms a left (splenic) flexure and passes into the descending colon. The descending colon becomes the sigmoid colon and then the rectum.
Symptoms of adenomatous and glandular polyposis
The first sign to start sounding the alarm is menstrual irregularities. Although sometimes the clinical picture is minimal or absent altogether.
- Bleeding and heavy menstruation. In the middle of the cycle, a woman may suddenly start bleeding, or the menstruation itself may proceed with copious amounts of blood. They can be considered abundant when the duration increases by several days or the blood volume exceeds 150-200 ml. Usually menstruation ends on the third or fifth day; if its duration exceeds seven days, then this is a reason to contact a gynecologist. But you should not pay attention to exceptions that may be caused by increased weight or a sudden change in climate, although visiting the doctor once again will not harm anyone.
- Lack of menstruation. All women may experience slight delays from time to time. In this case, it is worth waiting a few days, during which to observe possible changes in the body. But if menstruation, which always arrives on time, has been absent for a week, and pregnancy is excluded, then this indicates that it is urgently necessary to contact an antenatal clinic.
- Pain in the lower abdomen. Pain in the lower abdomen can be caused by both gynecological diseases and other problems; moreover, this pain can be false, that is, radiate from other parts of the body, and the woman thinks that she has a stomach ache. In any case, you need to visit a doctor who will determine the cause. Another symptom of endometrial polyposis is discomfort and pain during sexual intercourse. Any such signal should alarm a woman.
- Infertility. An undiagnosed polyp provokes infertility in a woman, since the outgrowths do not allow the fertilized egg to attach to the walls of the uterus. In most cases, it is during the treatment of infertility that polyps in the endometrium are identified. Unfortunately, patients do not seek help from a doctor in a timely manner, since polyposis is asymptomatic, which leads to a poor diagnosis.
One of the main reasons for the development of polyposis in the uterine cavity is considered to be heredity. This factor has been identified in 50% of women suffering from this disease. If the older generation has a tendency or polyposis itself, then the woman needs to seriously engage in examination to identify polyps in the uterus.
“THE SITE IS UNDER RECONSTRUCTION WE APOLOGIZE FOR THE TEMPORARY INCONVENIENCE”
Familial adenomatosis (diffuse polyposis)- a hereditary disease of the colon, the manifestation of which is the presence of multiple up to several thousand polyps (adenomas) (formations of the colon mucosa), in most cases detected as an accidental finding during colonoscopy or sigmoidoscopy. This disease requires constant monitoring by specialists, since polyps have a tendency to grow progressively and inevitably become malignant if not treated in a timely manner.
Cause and mechanism of development:
Linkage analysis carried out back in 1986-87 in families with FAP led to the mapping of the APC gene (OMIM 611731) on chromosome 5 in the 5q22 region. The largest proportion of cases of familial adenomatous polyposis of the colon are associated with mutations in this gene. Mutations in the APC gene lead to an almost 100% risk of developing the disease. It is known that the manifestations of familial adenomatous polyposis in different families differ in the severity of the disease, the prevalence of the process and the age of onset of the disease. Studying hereditary variants of the APC gene structure in connection with the genetic and clinical characteristics of FAP may provide new information about the mutation-clinical manifestation relationship, which may play an important role in the treatment of the disease.
However, not all patients with familial adenomatous polyposis have hereditary mutations in the APC gene. In 2002, another gene was mapped, mutations in which can also cause familial adenomatosis of the colon. This is the MYH gene located on chromosome 1p34 (OMIM 604933) [Al-Tassan 2002]. At the birth of a child, signs of the disease do not appear; later, as the body grows, at the age of 6-7 years, the appearance of small polyps on the mucous membrane of the colon can already be detected.
Clinical manifestations:
As a rule, symptoms of the disease most often appear during puberty, at the age of 15-19 years; at an early age there are no severe symptoms.
The most common and constant symptom is frequent stools up to 5-6 times a day mixed with blood and mucus. Bloody discharge from the anus is usually an admixture of liquid, semi-formed feces. Abdominal pain can have varying intensity and localization. Symptoms of the disease such as fatigue, weakness, and anemia most often begin to appear by the age of 20. For most patients, this coincides with an increase in workload: the beginning of work, military service, and for women, pregnancy and childbirth. With the development of cancer from polyps, the general condition of patients worsens, and new symptoms characteristic of the oncological process appear.
The most likely detection of the disease in patient groups:
- having clinical signs of polyposis: frequent stools mixed with blood and mucus since childhood, abdominal pain, anemia, etc.;
- relatives of patients with familial adenomatosis (children, parents, brothers, sisters, including cousins).
Diagnostics:
An endoscopic examination of the colon (colonoscopy) with multiple biopsies (sampling of pieces of tissue for histological examination) is required. An examination of the upper gastrointestinal tract is mandatory for a patient with familial adenomatosis. More than half of the patients have pathological changes in the stomach: gastritis, polyps, and sometimes malignant tumors.
The presence of polyps in the colon may be accompanied by formations in other organs and tissues: sebaceous gland cysts ( Alfield syndrome
), malignant formations of the central nervous system (brain) (
Turcot syndrome
), tumors of the endocrine glands (
Solinger-Ellison syndrome
), pigmentation of the mucous membrane and skin (
Peutz-Jeghers syndrome
), while the polyps have a different structure (hamartomas).
Treatment:
Currently, the only treatment for familial adenomatosis of the colon is surgical. The principle of surgical treatment of familial adenomatosis is to remove all parts of the colon where there are polyps, because sooner or later they develop into a cancerous tumor.
Forecast:
If a patient with familial adenomatosis of the colon is not treated, the development of cancer from one or more polyps is inevitable. Performing sphincter-preserving operations is possible in 85% of patients who applied before the polyps become malignant; with the development of cancer, such operations are possible only in 30% of patients.
Diagnostic methods
A person does not always know his ancestry - the lack of information about diseases among relatives reduces the risk of cancer. In addition to seeing a doctor, if you have symptoms, you should perform the following tests:
- transabdominal ultrasound scanning;
- sigmoidoscopy;
- colonoscopy;
- irrigoscopy.
Multiple intestinal polyposis on colonoscopy
The detection of 100 or more polypoid growths in the colon is the basis for diagnosis. It is important to conduct studies to identify extraintestinal tumors (FGS, bone x-ray, soft tissue MRI). It is mandatory to perform a biopsy for endoscopic diagnosis of familial intestinal polyposis - histological examination of tissue helps to detect colorectal cancer in a timely manner.
Reasons for appearance
Endometrial hyperplasia and polyps, that is, an increase in the number of cells in the inner lining of the uterus or cervix, can occur for several reasons.
Until now, scientists and doctors have not clearly established what the main reason for the appearance is. Hormonal disorders are currently considered the main risk factor for endometrial hyperplasia. In particular, an excess of estrogen and a lack of progesterone in a woman’s body affects her.
Risk factors for education are:
- anovulation;
- persistent follicle syndrome;
- hyperglycemia (with diabetes);
- presence of follicular cysts;
- granulosa cell tumors;
- menopausal syndrome;
- obesity;
- trauma to the uterine cavity (long-term wearing of an intrauterine device);
- abortions or miscarriages;
- complications during or after childbirth;
- chronic inflammatory diseases of the internal genital organs, endometritis;
- immunodeficiency states;
- thyroiditis, thyroidosis and other diseases of the thyroid gland.
Familial intestinal polyposis: prognosis for life
In the absence of diagnosis and treatment, familial intestinal polyposis becomes the cause of colorectal cancer in the majority (87-93%) of people over the age of 45 years. After surgery at the pre-tumor stage, the prognosis for life is favorable, but it is necessary to constantly be monitored by a doctor with an annual full examination (tumor markers, endoscopic examination methods).
Treatment with folk remedies
Traditional treatment can sometimes be a fairly rational solution, because alternative methods sometimes turn out to be very effective. Among the folk remedies for the treatment of endometrial polyps, garlic pulp is used, which is placed in gauze, a tampon is made with a long string and inserted into the vagina overnight. The course of folk treatment with garlic is 4 weeks.
Egg yolks and pumpkin seeds are also used. This folk method of treating endometrial polyps has been effectively used for decades. You need to take 6 chicken eggs, boil them, separate the yolks. Add 5 tablespoons of crushed pumpkin seeds and pour in 0.5 liters of sunflower oil. Heat this mass in a water bath and cool. You need to take one teaspoon orally in the morning and evening for 5 days. Then take a break for 1 week and repeat the 5-day course again.
These traditional methods of treatment, as a rule, do not produce any side effects, but may not always be effective.
Familial intestinal polyposis - features of the disease
Genetically programmed colon pathology is inherited, so every person who has a close relative with colon polyposis must undergo an examination with mandatory determination of gene mutations. Main features of the disease:
- early onset of pathology (often found in children and young people);
- the formation of a large number of polyps (hundreds and thousands);
- a real risk of malignancy (if familial intestinal polyposis is detected in a child, then one should be wary of the development of colorectal cancer at the age of about 30 years);
- hidden course of the disease (late detection of multiple polyps reduces the time interval between precancer and cancer);
- combination with other types of benign and malignant neoplasms (soft tissue, bone tumors).
If there is a hereditary predisposition, it is necessary to use all possible methods for early diagnosis of a precancerous condition - there is no need to wait for the first symptoms to appear, it is advisable to perform a full preventive examination with a colonoscopy every year.
Treatment tactics
With massive damage to the colorectal region by adenomatous polyps, only radical surgery is an effective method of treatment - by removing the entire large intestine, one can guarantee the prevention of mandatory malignant degeneration. If there is a family risk of cancer, it is necessary to constantly monitor the possible appearance of symptoms, have an annual colonoscopy and take an occult blood test. An important element of prognosis is performing special genetic studies to assess chromosomal defects, which is especially important for couples planning to have a child (if one of the future parents has familial intestinal polyposis or the presence of an APC gene mutation is confirmed, then the risk of having a baby with the pathology is 50% ).