For decades, the scientific community did not pay attention to the Zika virus, which affected residents of distant Africa and, very rarely, Asia. And for those places it was a “small caliber” - either Vibrio cholera or the Ebola virus! It was practically not studied, and therefore the world community was unprepared for the rapid spread of the virus across all continents in just a few years. How dangerous is the Zika virus? How is it built? What can we oppose to him and what conclusions can we draw from the current situation?
When the Zika virus (ZIKV) was first discovered in 1947, it received little attention. Until the 2015 report of a Brazilian wave of neonatal microcephaly. Concerned about the scale of the Zika outbreak and the severity of its associated defects, WHO issued a declaration from the International Health Regulations (IHR) Committee that the Zika virus is an emergency. The global scientific community has responded to this announcement with a flood of research aimed at understanding the functioning and management of the Zika virus.
In the era of globalization, due to the free movement of people around the world, the penetration of ZIKV into new regions becomes inevitable. There it can persist for a long time, transmitted from animals to animals and occasionally causing minor outbreaks of disease in humans, or circulate in the human population. The threat posed by any new disease depends on its epidemiology, clinical features, and the ability of the medical community to effectively control it (Fig. 1). And now enormous efforts have been devoted to studying the characteristics of the Zika virus and the mechanisms of its impact on human health, in particular on the health of pregnant women [1].
Figure 1. Municipal employee of the city of Recife (Brazil) during an operation to eradicate Aedes aegypti mosquitoes that carry the Zika virus.
website inosmi.ru
Chronology of events in the Zika epic
In African Uganda, near the port city of Entebbe near Lake Victoria, grows the Zika rainforest, whose name means “overgrown” in local Lugandan. This forest is famous for its huge diversity of plants, butterflies and especially mosquitoes, of which there are more than 40 species [2].
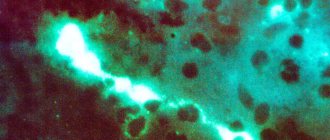
Figure 2. Transmission electron microscope (TEM) photomicrograph of Zika virus. Viral particles measuring 40 nm are colored blue.
"Wikipedia"
The Uganda Virus Research Institute (UVRI) is located in Entebbe, whose employees in 1947, while studying yellow fever in the Zika forest, isolated a hitherto unknown flavivirus from the blood of macaques. Scientists described it as the Zika virus (Figure 2). And the next year, the virus was discovered in Aedes africanus mosquitoes [3].
In 1952, the virus was identified in humans - in Uganda and Tanzania, and in 1954 - in Nigeria. ZIKV was clearly associated with fever and skin rash, leading to it being definitively declared pathogenic in humans. At the same time, in the 50s, the main carrier of the virus was established experimentally with the participation of volunteers - the Aedes aegypti mosquito, a common carrier of yellow fever, dengue fever and chikungunya. Later, it was accompanied by other species, including Aedes albopictus [1].
In the 60–80s, mild forms of infection were detected in Africa, Asia and India. The long-term presence of ZIKV in these regions was confirmed by detection of the virus in mosquitoes and non-human apes. Before 2007, not many clinical cases were recorded in humans, and therefore the health care system was in no hurry to sound the alarm [4].
The first major outbreak of Zika fever was reported in 2007 on the island of Yap in the Pacific Federated States of Micronesia, where 73% of the population were infected, but the vast majority had mild and short-lived symptoms. The next outbreak occurred in French Polynesia in 2013–2014, where 66% of the inhabitants were infected. A simultaneous wave of incidence of Guillain-Barré syndrome raised the question of its association with the Zika virus: then 42 cases were recorded - which is an order of magnitude more than in 2012, when three people were diagnosed with the syndrome [1].
In 2014, Zika spread across the South Pacific to New Caledonia, the Cook Islands and Easter Island. At the end of the year, reports appeared about the first confirmed cases of infection in northeastern Brazil (it was recently established that the virus was then spreading throughout Haiti). Over the next few months, ZIKV spread throughout Brazil.
In July 2015, it was suggested to be related to Guillain-Barré syndrome, and in October - to microcephaly. In February 2021, WHO issued the first IHR Committee emergency declaration [1], [4]. In the spring-summer of 2021, the connection between the infection and microcephaly received the first confirmation, which, however, does not yet allow us to state unequivocally that “the Zika virus causes microcephaly in the human fetus.”
By July 27, ZIKV was circulating in 67 countries and territories (Figure 3). A major outbreak occurred in Colombia, where 65,000 people were infected. Many of them had neurological syndromes, and cases of microcephaly were also noted [1].
In July 2021, two deaths associated with ZIKV infection were recorded: in the United States and Puerto Rico. It is believed that the deaths were caused not by the virus itself, but by symptoms of chronic diseases that worsened during the fever.
In mid-August 2021, Puerto Rico declared a state of emergency because the spread of the virus was gaining momentum too quickly: in six months (from December 2015 to August 12, 2016), the number of people infected increased from one to 10,000 people.
By September 1, 47 cases of the disease had been registered in American Florida, and in Miami Beach, for the first time in the United States, three mosquitoes carrying the Zika virus were discovered.
Figure 3. History of the spread of the Zika virus around the world.
[1]
The virus was first brought to Russia in February 2021 from the Dominican Republic. Over the past months, 7 more cases have been reported. All are from tourists returning from countries where ZIKV is spreading: most from the Dominican Republic, one from the Caribbean Islands. All patients survived the fever safely.
Zika is not Ebola. How dangerous is the virus?
Unlike Ebola, which has a very high mortality rate, Zika fever is not a fatal disease. Moreover, it is relatively easily tolerated. Its clinical picture is characterized by the following symptoms:
- slight headache,
- skin rash,
- malaise,
- pain in muscles and joints,
- conjunctivitis,
- sometimes elevated temperature.
Most often, the symptoms of an infected person are mild. The duration of their manifestation is usually from 2 to 7 days.
In almost all areas of our planet, with the exception of Antarctica, there are small aggressors - mosquitoes of the genus Aëdes, which translated from ancient Greek means “vile”, “disgusting”. In tropical regions, this “bug” can be a carrier of flaviviruses - yellow fever virus, dengue virus, Zika virus, etc. By the way, the more well-known tick-borne encephalitis virus in Russia also belongs to flaviviruses, but it is transmitted not by mosquitoes, but by ticks.
The Zika virus was first isolated in 1947 from rhesus monkeys in the African state of Uganda, in a tropical area (as you might guess) called Zika. Since then, it has been named after this lost Ugandan region. In 1952, the virus was first identified in humans - in Uganda and neighboring Tanzania. Over the next thirty years—thanks to the ubiquity of the Aëdes biter—evidence of the Zika virus was found not only in many countries in Africa, but also in Asia (as far as Indonesia) and Oceania.
Pathogenesis of Zika fever
Virus transmission and disease development
ZIKV is transmitted to humans by the bite of infected Aedes mosquitoes, which typically attack during the day, with peak activity in the early morning and evening. Several cases of sexual transmission of the Zika virus have been reported [5–7], and the possibility of infection through blood transfusion cannot be excluded [4], [8].
A minority of those infected experience some symptoms: on the island of Yap, only 19% of those infected reported symptoms, and in French Polynesia - 26%. If signs of fever develop, then in 95% of cases this occurs 6–11 days after infection (Fig. 4). Symptoms are similar to those of other similar infections [1], [4]:
- increased body temperature;
- skin rash;
- pain in joints and muscles;
- headache;
- conjunctivitis;
- swelling;
- sometimes vomiting;
- general malaise.
Figure 4. Diagram of the course of infection in humans and mosquitoes. On average, symptoms develop on the sixth day after infection. Around the ninth day, the production of immunoglobulins (antibodies) begins: IgM is detected first, the amount of which later decreases along with an increase in the concentration of IgG. The latter remains in the blood indefinitely. Viremia likely occurs before the onset of symptoms, and its duration affects the risk of infection by susceptible mosquitoes that bite an infected person. After a certain incubation period, the mosquito acquires the ability to transmit the pathogen to other people. Tg is the interval between the episodes of infection of the first and second person.
[1]
ZIKV is present in blood, saliva, urine, semen, amniotic fluid, and nerve tissue. It can be isolated from the blood within an average of 10 days after infection (in 99% of those infected, the blood is completely cleared of the virus within 24 days). According to some reports, the virus remains in urine for 12 days, and in semen for more than 60. Pregnancy can prolong the period of carriage: one patient, infected at 11 weeks of pregnancy, remained viremic for another 10 weeks, but was completely cleared of the virus 11 days after termination of pregnancy . Mosquitoes become infectious approximately 10 days after exposure to ZIKV (Figure 4).
Viremia, or viremia, is a medical condition where viruses enter the bloodstream and can spread throughout the body, similar to bacteremia, where bacteria enter the bloodstream [9]. - Ed.
The Zika virus enters a cell by interacting with certain receptors on its surface. The main one is AXL . And the mediator is the TIM-1 receptor, which binds viral particles and transports them to AXL, which facilitates the penetration of the virus into the cell. However, TIM-1 is not a necessary link; it only increases the concentration of virions on the cell surface and accelerates their interaction with AXL [10].
Once the virus is inside a cell, it responds by increasing the production of interferons IFN-α and IFN-β, as well as the chemokines CXCL10 and CXCL11, which play an important role in innate and adaptive immunity. These chemokines attract T cells and other leukocytes to the site of inflammation and even have a direct antimicrobial effect when their concentration in skin fibroblasts is greatly increased [10].
At the same time, ZIKV infection initiates the autophagy program [11]. Autophagy is intended not only for the degradation of proteins and damaged cell organelles, but also to resist infectious agents, that is, it is an immune tool. For example, when cells are infected with Sendai, vesicular stomatitis, or herpes simplex type I viruses, destruction of viral proteins through autophagy limits viral replication and promotes cell survival. On the other hand, this process can be turned by viruses against the cell itself. Thus, some flaviviruses (for example, dengue and chikungunya viruses) use components of the autophagy pathway to support their replication and spread by “cleaning up” the cell. The importance of autophagy in the Zika virus cycle remains to be seen [10].
Antibodies to the virus are detected in the blood already on the ninth day after infection. The duration of immunity against ZIKV is not yet known, but based on other flaviviruses, it can be assumed to be lifelong [1].
Deaths due to Zika virus infection are extremely rare and are observed only in patients with comorbidity or immunodeficiency. However, those infected are at increased risk of serious neurological complications, such as Guillain-Barré syndrome, which is fatal in 3-10% of cases, regardless of the cause. Other complications, including meningoencephalitis and myelitis, have been reported, but the association with Zika virus in these cases has not been reliably established [1].
Zika virus and pregnancy
Most of all, scientists and society as a whole are concerned about the connection between viral infection during pregnancy and embryonic microcephaly. From the outbreak in late 2014 to May 7, 2021, 7438 suspected cases of microcephaly were reported in Brazil [12]. Before this, no more than 200 were recorded annually, which, of course, leads to certain thoughts.
However, establishing a connection between ZIKV and microcephaly has proven to be quite difficult due to several circumstances:
- It remains unclear how many pregnancies the virus has affected - the infection is often asymptomatic;
- there is still no clear definition of microcephaly;
- There are other infectious agents that cause microcephaly: cytomegalovirus and Rubella virus (rubella virus).
Yet, based on the discovery of Zika virus in the amniotic fluid and brain of microcephalic embryos, the CDC in April 2021 recognized the link between ZIKV and microcephaly. This conclusion was later confirmed by experimental work on mice, which showed that the virus easily penetrates the placenta and infects embryonic neural stem cells [1], [13]. It is believed that the Zika virus prefers neuronal precursor cells, since their surface is more saturated with AXL receptors than others [14]. This assumption has been confirmed by recent experiments. American scientists have shown using a mouse model that when infecting a pregnant animal, the virus rushes to the placenta, where its concentration can be 1000 times higher than in the blood [15]. Chinese researchers went further and injected ZIKV directly into the embryonic brains of 13-day-old mouse embryos. As a result, there was a delay in the development of the organ, corresponding to the concept of “microcephaly”. In this case, the virus infected almost all brain cells, but the main, primary target was progenitor cells and immature neurons. The virus delayed their division and differentiation and provoked apoptosis. With rare exceptions, the dying fetal cells were mature and immature neurons. It was not possible to trace the postnatal history of the pups, since the mothers did not consider such offspring worthy of care and... ate them [16].
Symptoms of infection in pregnant women are the same as in other women, but it is not yet known whether the immunodeficiency characteristic of this period affects the frequency of their manifestations. The results of studies regarding the adverse effects of the disease on the embryo are very heterogeneous: somewhere in 29% of pregnant women with symptoms of the disease, an embryo with microcephaly developed, and somewhere in 74%. Perhaps such discrepancies arose because the studies involved an insufficient number of patients - less than 50 people. What can be said with some certainty is that ZIKV-associated microcephaly will develop in the fetus of one in every hundred women infected in the first trimester, regardless of the presence of symptoms, and this risk becomes insignificant in the second and third trimesters [1].
In addition to microcephaly, other embryonic pathologies are now associated with the Zika virus [1]:
- intracranial calcification;
- ventriculomegaly;
- visual defects;
- brainstem hypoplasia;
- intrauterine growth retardation;
- stillbirth.
Practical Information: Treatment and Prevention of Zika Fever
The Zika virus was first isolated in 1947 from rhesus monkeys in the African state of Uganda, in a tropical area (as you might guess) called Zika.
Since then, it has been named after this lost Ugandan region. In 1952, the virus was first identified in humans - in Uganda and neighboring Tanzania. By the way, the main problem of Zika fever lies in the lack of research, since the virus, in fact, has only just manifested itself. Accordingly, vaccines, and even more so specific drugs, are still far away. However, WHO notes that the disease “does not require specific treatment.” Recommendations include drinking enough fluids, getting plenty of rest, and “taking your usual medications to relieve pain and fever.” Of course, if your symptoms worsen, you should consult a doctor.
Personal preventive measures boil down to the use of repellents, clothing that covers the body as much as possible, preferably in light colors (it is believed that mosquitoes are attracted to dark and bright colors), mosquito nets and other protective measures. You should, of course, avoid accumulation and stagnation of water in containers. During outbreaks of fever, health authorities can organize widespread spraying of insecticides and treatment of water bodies with them.
Zika virus device
Genome organization
By the end of August 2021, 67 complete ZIKV genome sequences were deposited in GenBank. The Zika virus contains a coding RNA molecule 10.8 kb long. with one ORF (open reading frame) flanked by untranslated regions (UTR) - 5′-UTR 106 nt long. and 3′-UTR 428 nt long. (Fig. 5). The ORF encodes a polyprotein precursor that is subsequently divided into three structural proteins (capsid [ C ], premembrane [ prM ], and envelope [ E ]) and seven nonstructural proteins ( NS1 , NS2A , NS2B , NS3 , NS4A , NS4B and NS5 ). The viral polyprotein is cleaved during and/or posttranslation by a viral protease, a signal peptidase, and an unknown host cell protease. The pr fragment is then usually excised in the Golgi apparatus by furin during the production of mature virions [17].
Figure 5. Virus genome (represented as a sequence of RNA-encoded protein products). Structural proteins are colored gray, non-structural proteins are colored blue. The numbers indicate the lengths of proteins (the number of amino acid residues). Arrows indicate sites of polyprotein cleavage.
[17], figure adapted
Basic proteins
Protein E is the main surface glycoprotein of flaviviruses, and the nonstructural proteins NS3 and NS5 are the main enzymes of viral reproduction [17]. The structure of these proteins is shown in Figure 6.
Figure 6. Structure of ZIKV major proteins.
[17]
Protein E is divided into two structural regions - stem and transmembrane (in Fig. 6 - stem and TM) - and three functional domains: domain I is involved in the organization of the shell (Fig. 7), domain II is responsible for the interaction of monomers, and domain III binds cellular receptor.
NS3 consists of protease and helicase-NTPase domains, which process the viral polyprotein and unwind the structured regions during viral RNA synthesis.
NS5 contains a methyltransferase domain, which methylates the 5'-CAP region of genomic RNA, and an RNA-dependent RNA polymerase (RdRp) domain.
Figure 7. Atomic resolution 3D model of the Zika virus , created by the Visual Science biomedical imaging studio. The model is based on scientific publications on the organization of the Zika virus and related viruses and is considered the most reliable at the moment.
website visual-science.com
Glycosylation is known to play an important role in the infectivity, maturation and virulence of flaviviruses [18], [19]. For the Zika virus, potential N- and O-glycosylation sites have been predicted in the prM, E, NS1, and NS4B proteins, which are also glycosylated in other flaviviruses. Studies investigating the role of these sites in the Zika virus life cycle are still being planned [17]. True, one structural difference between the ZIKV E protein and similar proteins of other flaviviruses has already been discovered - an amino acid loop exposed on the surface of the viral particle, to which a glycan binds at the Asn154 position (see video). It is assumed that this loop, together with the attached sugar, may be responsible for the tropism of the virus (interaction with receptors of a certain group of cells) and the pathogenesis of the disease [20].
Differences in the structure of the ZIKV E protein from homologous proteins of other flaviviruses.
research group at Purdue University, USA
Repellent and pharmacy
Our country also has a lot of its own “homegrown” pathogens transmitted by insects. So let's talk about repellents. More often, consumers buy them at a supermarket or hardware store. Why not at the pharmacy? After all, repellents are essentially preventive agents that protect our body from pathogenic factors. Based on this, they should be present in the pharmacy assortment, especially since they are sprayed on the skin. But can they be present there from a legal point of view?
Clause 7 of Article 55 of the Law “On the Circulation of Medicines” (No. 61-FZ dated April 12, 2010) lists the groups of goods that pharmacy organizations have the right to sell. Repellents are not specifically mentioned on this list, but “medical products” are included.
In the All-Russian Classification of Products (OKP), repellents appear in two sections at once. Firstly, in section 23 0000, which lists groups of household chemical products. Here, repellents under code 23 8620 coexist with insecticides (“products for combating household insects”) and zoocides (“products for combating domestic rodents”).
Repellents - under a different code, OKP 93 9260 - are also included in section 93 0000, called “Medicines, chemical-pharmaceutical products and medical products.” Here they are in similar proximity to disinfectants (93 9210), disinfestation (93 9220) and deratization (93 9230) agents.
Thus, the possibility of selling a particular repellent in a pharmacy or pharmacy depends on which of these codes it is registered with Rospotrebnadzor. If the code is 93 9260, then the repellent can be classified as medical products (medical devices) and be present in the pharmacy assortment.
Fighting the Zika virus
Diagnostics
The main problems in diagnosing ZIKV infection are the significant number of asymptomatic cases and the nonspecificity of symptoms: dengue fever and chikungunya, which are also transmitted by Aedes mosquitoes, manifest themselves in a similar way. Zika virus infection can be suspected if symptoms appear in a person who has recently visited or lived for a long time in an area where ZIKV is circulating [1], [4].
A preliminary diagnosis can be confirmed only with the help of a laboratory test of blood or other biological fluids: urine, semen or saliva. For this purpose, the RT-PCR method is used. However, the timing of sampling is very important for such tests: viral RNA is detected in the blood within 3–5 days after the onset of symptoms (about 10 days after infection); in other liquids the virus can be “caught” later [1], [4].
A better solution would be a highly specific antibody test that could be used not only to confirm infection, but also to test immunity against Zika virus early in pregnancy, allowing women to understand their risk level. However, such testing is complicated by cross-reactivity with other flaviviruses. The ELISA test offers some hope. For example, an IgG ELISA used in French Polynesia, where the dengue virus circulates, identified ZIKV-positive blood donors (then <1%) even before the main Zika outbreak [1].
Prevention
The main way is to protect against mosquito bites, including by controlling their spread.
In regions where the Zika virus circulates and in potentially dangerous areas, people are advised to wear light-colored clothing that covers as much of the body as possible, install mosquito nets on windows and doors of their homes, use a net while sleeping, and use repellents containing DEET, IR3535, or icaridin [4] .
Female Aedes mosquitoes, after feeding on blood, lay eggs that can survive for up to a year in an anhydrous environment. Even in a minimal amount of water, larvae emerge from the eggs and further develop into adults. Therefore, to control the number and spread of mosquitoes, it is necessary to constantly monitor and eliminate their breeding places: buckets, barrels, pots of water, gutters, used car tires. In special cases, they resort to spraying insecticides [4].
An example of effective vector control is William Gorgas' efforts to eliminate the yellow fever epidemic in Havana and the Panama Canal region at the beginning of the 20th century. This American military doctor and his team staged a brutal fight against unsanitary conditions and treated all buildings and streets with insecticides (from which, by the way, many residents also suffered). As a result, yellow fever was completely defeated [21].
In the 1950s and 1960s, America used intensive measures to control the spread of the yellow fever pathogen, including widespread spraying of DDT. This has resulted in the elimination of Aedes aegypti from 18 countries and has significantly reduced the area of distribution of the disease. Later, similar programs were successfully implemented by Singapore and Cuba. Of course, after some time the fever returned, but even a short period without infection was of great importance for the population [1].
To reduce the risk of sexual transmission of ZIKV (especially during pregnancy), for men living in areas where the virus is circulating or who have recently traveled there, WHO recommends using condoms or abstaining from sexual activity throughout their partner's pregnancy [4].
Treatment
Usually the disease is mild and does not require special treatment. During fever, rest and drinking plenty of fluids are necessary, and sometimes taking medications to eliminate pain and other unpleasant symptoms [4].
However, there are substances that have an effect on the Zika virus itself. For example, 2′-C-methyladenosine effectively suppresses virus reproduction in vitro, and 7-deaza-2′-C-methyladenosine (MK-608) inhibits ZIKV replication in vitro and inhibits the development of the disease in experiments on mice. The drugs 2′-C-methylcytidine, ribavirin, favipiravir and T-1105 weaken the cytopathic effect of the virus and reduce its yield [22], [23].
Of course, a vaccine would solve the problem radically, but it has not yet been developed. Currently, 18 commercial companies and research institutes are engaged in research [24–26]. However, the first phase of clinical trials will not start until the end of 2016, which means that a ready-made vaccine will not appear soon, and the spread of infection around the world will continue [1].
Helpful information
The majority of the planet's inhabitants - including Russian citizens - do not live in tropical and subtropical regions. Should they be concerned about Zika and what should they know to prevent it?
First. How the Zika virus is transmitted: The virus can be transmitted by two types of mosquitoes - Aedes aegypti and Aedes albopictus. In the current epidemic, the first of them predominates, distributed in tropical and subtropical regions and does not survive in less warm climates. This is a positive thing. But the second species can survive in a state of hibernation in climate zones with lower temperatures. However, it can be noted that in those countries of Latin America where there are no tropics - Argentina, Chile, Uruguay - Zika fever has not yet spread.
In January-February 2021, isolated cases of this disease were recorded in European and North American countries - Spain, Switzerland, USA, Ireland, Canada, Denmark - as well as Australia and China. They are all imported: people returning from Brazil, Africa, etc. were bitten there by mosquito vectors.
In mid-February, the media reported about a woman who returned to Russia from the Dominican Republic and felt unwell a few days later. Laboratory tests revealed the Zika virus in the patient. Her illness was mild, and she was soon discharged. “The fact that a sick person has flown to us, infected somewhere in the tropics, does not mean at all that now Russian residents will immediately begin to get sick,” virologist Alexander Platonov commented on this isolated case in an interview with Vesti.ru, “without the corresponding mosquitoes, and even the virus cannot be transmitted in such weather.”
According to current data, the Zika virus can only be transmitted from person to person through sexual contact. In this regard, the Central Research Institute of Epidemiology of Rospotrebnadzor recommends using barrier contraception for at least a week upon returning from virus-endemic countries (Vesti.ru). You should also refrain from kissing upon returning from these countries. The exact number of days of “limited love quarantine” is arbitrary, since the duration of the incubation period, according to WHO information, is not yet reliably known.
The effects of the Zika virus on the body have also been poorly studied. It is assumed that it may cause the development of microcephaly in newborns whose mothers were infected during pregnancy. Brazilian health authorities have noted an increase in cases of Guillain-Barre syndrome (an autoimmune disease that develops after previous infections) in the country, which coincided with the current Zika fever epidemic. What exactly the consequences of infection with the virus and what symptoms indicate this are not currently known with certainty.
Literature
- Lessler J., Chaisson LH, Kucirka LM, Bi Q., Grantz K., Salje H. et al. (2016). Assessing the global threat from Zika virus. Science. 353 , aaf8160;
- Wikipedia : "Zika (forest)";
- Wikipedia : "Zika fever";
- Disease caused by the Zika virus. (2016). WHO fact sheet;
- Deckard DT, Chung WM, Brooks JT, Smith JC, Woldai S, Hennessey M et al. (2016). Male-to-male sexual transmission of Zika virus — Texas, January 2021. MMWR Morb. Mortal. Wkly Rep. 65, 372–374;
- Venturi G., Zammarchi L., Fortuna C., Remoli M.E., Benedetti E., Fiorentini C. et al. (2016). An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill. 21 , doi: 10.2807/1560-7917.ES.2016.21.8.30148;
- Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da Rosa A, Haddow AD et al. (2011). Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg. Infect. Dis. 17, 880–882;
- Boadle A. (2016). Brazil reports Zika infection from blood transfusions. Reuters;
- Wikipedia : "Virusemia";
- Hamel R., Dejarnac O., Wichit S., Ekchariyawat P., Neyret A., Luplertlop N. et al. (2015). Biology of Zika virus infection in human skin cells. J. Virol. 89, 8880–8896;
- Autophagy, protophagy and others;
- Victora C. G., Schuler-Faccini L., Matijasevich A., Ribeiro E., Pessoa A., Barros F. C. (2016). Microcephaly in Brazil: how to interpret reported numbers? Lancet. 387, 621–624;
- Cugola FR, Fernandes IR, Russo FB, Freitas BC, Dias JL, Guimarães KP et al. (2016). The Brazilian Zika virus strain causes birth defects in experimental models. Nature. 534, 267–271;
- Nowakowski T. J., Pollen A. A., Di Lullo E., Sandoval-Espinosa C., Bershteyn M., Kriegstein A. R. (2016). Expression analysis highlights AXL as a candidate Zika virus entry receptor in neural stem cells. Cell Stem Cell. 18, 591–596;
- Miner JJ, Cao B, Govero J, Smith AM, Fernandez E, Cabrera OH et al. (2016). Zika virus infection during pregnancy in mice causes placental damage and fetal demise. Cell. 165, 1081–1091;
- Li C., Xu D., Ye Q., Hong S., Jiang Y., Liu X. et al. (2016). Zika virus disrupts neural progenitor development and leads to microcephaly in mice. Cell Stem Cell. 19, 120–126;
- Ye Q., Liu Z. Y., Han J. F., Jiang T., Li X. F., Qin C. F. (2016). Genomic characterization and phylogenetic analysis of Zika virus circulating in the Americas. Infect. Genet. Evol. 43, 43–49;
- Kim JM, Yun SI, Song BH, Hahn YS, Lee CH, Oh HW, Lee YM (2008). A single N-linked glycosylation site in the Japanese encephalitis virus prM protein is critical for cell type-specific prM protein biogenesis, virus particle release, and pathogenicity in mice. J. Virol. 82, 7846–7862;
- Li J., Bhuvanakantham R., Howe J., Ng M. L. (2006). The glycosylation site in the envelope protein of West Nile virus (Sarafend) plays an important role in replication and maturation processes. J.Gen. Virol. 87, 613–622;
- Sirohi D., Chen Z., Sun L., Klose T., Pierson T. C., Rossmann M. G., Kuhn R. J. (2016). The 3.8 Å resolution cryo-EM structure of Zika virus. Science. 352, 467–470;
- Patterson R. (1989). Dr. William Gorgas and his war with the mosquito. CMAJ. 141, 596–597, 599;
- Zmurko J., Marques R.E., Schols D., Verbeken E., Kaptein S.J., Neyts J. (2016). The viral polymerase inhibitor 7-deaza-2'-C-methyladenosine is a potent inhibitor of in vitro Zika virus replication and delays disease progression in a robust mouse infection model. PLoS Negl. Trop. Dis. 10 , e0004695;
- 454 sequencing (high-throughput DNA pyrosequencing);
- Cohen J. (2016). Zika vaccine has a good shot. Science. 353, 529–530;
- Abbink P., Larocca RA, De La Barrera RA, Bricault CA, Moseley ET, Boyd M. et al. (2016). Protective efficacy of multiple vaccine platforms against Zika virus challenge in rhesus monkeys. Science. pii: aah6157;
- Larocca RA, Abbink P, Peron JP, Zanotto PM, Iampietro MJ, Badamchi-Zadeh A. et al. (2016). Vaccine protection against Zika virus from Brazil. Nature. 536, 474–478..
Symptoms of Zika virus disease
The first manifestations of the disease are similar to typical arboviral fevers, such as dengue fever. Symptoms of Zika virus infection include:
- High body temperature.
- Rash (exanthema - spotted papular rubella-like rash) on the skin.
- Development of conjunctivitis.
- Presence of muscle pain and joint pain.
- Headache.
All symptoms of the Zika virus are mild, usually their manifestations persist for 2 to 7 days.
During periods of massive outbreaks of the Zika virus, possible complications were recorded, including autoimmune and neurological disorders. Similar cases were recorded in 2013 in French Polynesia and in 2015 in Brazil. All complications were studied and described by national health authorities.
Also during these two major outbreaks, a link was identified between the Zika virus and the birth of infants with microencephaly, a disorder of brain development in which the brain mass and skull size are smaller than normal. Microencephaly is a cause of mental retardation, which affects the length and quality of life of the patient. It is impossible to prevent the development of this disorder, just as there is no treatment (only symptomatic).
Now virologists, neurologists and perinatologists continue to study the true impact of the Zika virus on the development of intrauterine fetal disorders, and also study possible other consequences of the disease caused by the Zika virus.