Author:
Chekaldina Elena Vladimirovna otorhinolaryngologist, Ph.D.
Quick Transition Treatment of Peritonsillar Abscess
A peritonsillar abscess (PTA) is a collection of pus between the tonsil capsule and the pharyngeal muscles.
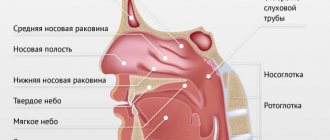
The anterior PTA is most often diagnosed; it is localized between the upper pole of the tonsil and the anterior palatine arch. They also distinguish between the posterior PTA - between the tonsil and the posterior palatine arch, the lower PTA - at the lower pole of the tonsil, the external PTA - outside the tonsil.
Peritonsillitis is an infectious inflammatory disease of the tissue surrounding the palatine tonsil, without the formation of an abscess (cavity with pus).
Paratonsillitis or PTA is usually preceded by acute tonsillopharyngitis, but in some cases the disease can develop without a previous infection of the pharynx, which is associated with blockage of the salivary glands.
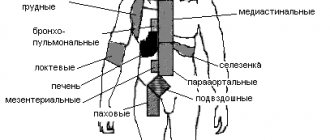
Peritonsillar abscess is the most common infection of the deep tissues of the neck in children and adolescents, accounting for at least 50% of cases. The annual incidence of PTA is 30-40 cases per 100,000 people aged 5 to 59 years.
The main causative agents of PTA are Streptococcus pyogenes (beta-hemolytic streptococcus group A, GABHS), Streptococcus anginosus (angios streptococcus), Staphylococcus aureus (Staphylococcus aureus, including methicillin-resistant strains - MRSA) and respiratory anaerobes (including Fusobacteria, Prevotella and Veillon).
Symptoms of paratonsillar abscess
The typical clinical manifestation of PTA is severe sore throat (usually unilateral), fever, and muffled voice. Patients may also complain of drooling and difficulty swallowing.
Trismus (spasm of the masticatory muscles), associated with irritation and reflex spasm of the internal pterygoid muscle, occurs in almost 2/3 of patients and is an important distinguishing feature of PTA in comparison with severe acute tonsillopharyngitis. Patients may also complain of neck swelling and ear pain on the affected side.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0 | 0 | 10 | 2 | 2 | 2 | 2 | 0 | 0 | 10 | 2 | 2 | 2 | 2 |
Diagnostics
In the vast majority of cases, the diagnosis of PTA is made clinically, based on the results of pharyngoscopy (examination of the pharynx). It is confirmed by obtaining purulent discharge during drainage of the abscess or by instrumental studies (most often ultrasound).
Pharyngoscopy reveals a swollen and/or fluctuating tonsil with deviation of the uvula in the direction opposite to the lesion, hyperemia (redness) and swelling of the soft palate. In some cases, there is plaque or liquid discharge in the palatine tonsil. There is an increase and tenderness of the cervical and submandibular lymph nodes.
Bilateral PTA is extremely rare and its diagnosis is more difficult due to the lack of asymmetry in the pharynx, as well as the rarely present spasm of the masticatory muscles.
Laboratory tests are not required to make a diagnosis; they are additionally prescribed to determine the severity of the disease and select a treatment method.
Laboratory tests may include:
- general blood test with leukocyte formula;
- study of electrolytes (potassium, sodium, chlorine) for signs of dehydration;
- strepta test to exclude GABHS;
- culture for aerobic and anaerobic bacteria if the abscess was drained (culture is recommended only for complicated PTA, recurrent PTA, or in patients with immunodeficiency conditions).
Instrumental examination methods - ultrasound, computed tomography, lateral neck x-ray, magnetic resonance imaging or angiography - are not necessary and are performed to exclude other diseases if the diagnosis of PTA is not obvious.
Differential diagnosis
Severe course of acute tonsillopharyngitis . Frequent pathogens are Epstein-Barr virus, herpes simplex virus, Coxsackie virus (herpangina), adenovirus, diphtheria, GABHS, gonorrhea. It manifests itself as bilateral swelling in the throat, hyperemia, and plaque may be present on the tonsils.
Epiglottitis . An inflammatory disease of the epiglottis, usually caused by Haemophilus influenzae. More common in young children who have not been vaccinated against Haemophilus influenzae type b. Progresses faster than PTA. Manifested by sore throat, drooling, difficulty swallowing, respiratory failure.
Retropharyngeal abscess (retropharyngeal abscess) . Purulent inflammation of the lymph nodes and tissue of the retropharyngeal space. Most often observed in children aged 2 to 4 years. During pharyngoscopy, minimal changes are noted. Main complaints: stiff neck, pain on movement, especially when extending the neck (as opposed to the increased pain on flexion seen with meningitis), swelling and tenderness of the neck, chest pain, difficulty swallowing, drooling, muffled voice, spasm of the masticatory muscles ( present in only 20% of cases).
Causes of the disease
Peritonsillitis occurs when pathogens enter the tissues around the tonsils.
The causative agents of the disease are streptococci, staphylococci, and fungi.
How do pathogenic microorganisms get into the paramygdaloid tissue? There may be several reasons for the start of the inflammatory process:
- untreated tonsillitis, when bacteria from the tonsils penetrate into nearby tissues;
- exacerbation of chronic tonsillitis, when pathogenic microflora also penetrates from the tonsils;
- dental diseases - for example, caries (infection comes from the oral cavity), although it is not necessary that the tonsils themselves become inflamed;
- injury to the tissue around the tonsils, during which infection occurs;
- infection through the bloodstream;
- chronic accumulations of infection in the body (for example, chronic sinusitis);
- diabetes;
- reduced immunity;
- smoking.
Typically, purulent inflammation acts as a complication of chronic or acute tonsillitis (tonsillitis) - this is the most common cause of the disease.
Treatment of peritonsillar abscess
In case of a complicated course, children (especially young children) are indicated for hospitalization and treatment in a hospital setting.
The main treatment method for PTA is systemic antibacterial therapy. In severe cases, severe intoxication, difficulty swallowing, nausea, antibacterial therapy is prescribed parenterally (bypassing the gastrointestinal tract) with subsequent transfer to oral forms of drugs - until the completion of the 14-day course of treatment. Courses of antibiotic therapy for less than 10 days increase the likelihood of disease relapse.
After prescribing systemic antibiotic therapy, dynamic observation for 24 hours is recommended. It is acceptable in patients with suspected paratonsillitis, without obvious signs of PTA, without signs of airway obstruction, sepsis, severe spasm of the masticatory muscles, or other signs of a complicated course of the disease. And also in children under 7 years of age with small abscesses and rare episodes of acute tonsillopharyngitis in history.
Studies have shown that systemic antibiotic therapy is effective even without draining the abscess. According to available data, 50% of children responded to systemic antibiotic therapy and did not require abscess drainage or tonsillectomy.
Systemic antibacterial therapy should include antibiotics active against GABHS, Staphylococcus aureus and respiratory anaerobes. For PTA, amoxicillin-clavulanate, ampicillin-sulbactam, and clindamycin are most often prescribed. If there is no or severe response, vancomycin or linezolid is added to treatment to ensure optimal coverage of potentially resistant Gram-positive cocci.
There are 3 methods of PTA drainage:
- PTA puncture - purulent discharge is removed through an aspiration needle;
- drainage of the PTA through the incision;
- tonsillectomy.
Draining an abscess never precludes the use of systemic antibiotic therapy.
All 3 methods of abscess drainage are comparable in effectiveness. The choice of procedure depends on the patient's condition, severity of the disease, presence of complications, age and the patient's ability to cooperate with the doctor.
For patients without spasm of the masticatory muscles or a history of recurrent acute tonsillopharyngitis, puncture drainage of the PTA or drainage of the abscess through an incision is recommended, which can be performed on an outpatient basis under local anesthesia.
Tonsillectomy is preferred in the following cases:
- presence of previous episodes of PTA or recurrent tonsillopharyngitis;
- significant upper airway obstruction or other complications;
- ineffective abscess drainage;
- presence of other indications for tonsillectomy (for example, obstruction of the upper respiratory tract and snoring due to the large size of the tonsils).
Randomized trials comparing puncture RTA drainage with incisional RTA drainage have shown comparable abscess resolution in more than 90% of cases.
Data on the benefits of systemic hormonal therapy (glucocorticoids) in the treatment of PTA are conflicting. Some studies show that the use of glucocorticoids (dexamethasone) can reduce the duration of symptoms of the disease, as well as reduce pain after drainage of the PTA. Other studies have reported no clear benefits of glucocorticoids in adults or children. Because the number of patients in these studies was small (ranging from 40 to 250 cases), further study of the effectiveness of routine use of glucocorticoids in the treatment of PTA is necessary.
Relapses of PTA occur in 10-15% of cases, more often in patients with a history of recurrent acute tonsillitis.
A risk factor for PTA is smoking.
Indications for autopsy
Drug therapy is possible only at the stage of paratonsillitis, when there is inflammation, but there is no abscess yet. If antibiotic therapy was not carried out in the first two to three days, the abscess will need to be opened. At the stage of purulent inflammation, conservative treatment will not give a positive result.
In 25% of cases, the abscess opens on its own without surgical intervention. At the same time, the temperature drops sharply, the pain goes away and recovery occurs. But if this does not happen, then the patient is shown opening the abscess cavity with a scalpel.
If the operation is not performed, then the purulent inflammation can go further, which poses a danger to life.
Types and forms of PTA
Depending on the location of inflammation, there are:
- anterior paratonsillar abscess. In most clinical cases, pus accumulates near the upper pole of the tonsil, behind the anterior arch and soft palate;
- lateral paratonsillar abscess. Exudate forms between the pharyngeal fascia and the tonsil capsule. There are right-sided and left-sided PTA;
- posterior abscess. Pus accumulates in the posterior arch area. Pathology can provoke swelling of the larynx with subsequent stenosis;
- lower PTA. Rarely seen. In this case, the anterior palatal arch is displaced downwards from the front due to infiltration of the lower part.
Peritonsillar abscess has the following clinical and morphological forms:
- edematous. It occurs without significant inflammation without significant manifestations of symptoms. Because of this, the form of the disease is rarely diagnosed;
- infiltration Hyperemia occurs. Manifested by pain, fever;
- abscessing. Forms 4-7 days after the development of infiltration changes.
Preparing for surgery
Surgery is performed only when the abscess is “ripe,” that is, a purulent pocket is completely formed. This usually occurs on the 5th day after tonsil swelling occurs.
Checking the readiness of the cavity for opening is carried out by a diagnostic puncture. Using a large needle, a puncture is made in the place that sticks out the most. All manipulations are controlled by an ultrasound machine or endoscopic observation. If pus is detected in the sample, it means that the abscess is ripe for surgery.
If necessary, a blood test is prescribed, as well as a culture to determine the pathogen and check for resistance to antibacterial drugs.
After the examination, the patient is sent to the operating room, where the abscess will be surgically opened.
Rehabilitation
The recovery process takes 1-2 weeks. You can eat almost immediately, but the food must be liquid. For several days after the procedure of opening the abscess, the wound will hurt while swallowing food.
After the operation, you should adhere to the following rules:
- do not warm your neck;
- do not drink very hot or cold drinks;
- the menu should include liquid food without acid and spices (they will irritate the wound);
- exclude alcohol, preferably not smoke;
- avoid hypothermia;
- take medications prescribed by your doctor (vitamins, antibiotics).
It is important to sanitize all possible foci of infections in the oral cavity and nasopharynx. It is necessary to remove caries, treat chronic throat diseases and strengthen the immune system.