Pneumonia is a serious disease, which in the absence of timely treatment can lead to a number of serious complications, and in advanced cases poses a danger to the patient’s life.
Therefore, at the first signs of the disease in the form of cough, fever, it is imperative to seek medical help. Doctors at the Yusupov Hospital will conduct an examination, a number of diagnostic procedures, make a diagnosis and prescribe an effective course of treatment.
Typically, pneumonia occurs as a complication of a cold. The first symptoms of pneumonia are very similar to the signs of acute respiratory infections. Weakness, cough and fever may indicate pneumonia. Initially, the temperature rises above 38 degrees only in the evening. In the morning it is within normal limits. In people with high immunity, this condition can occur for about two weeks. In this case, the patient is constantly bothered by a dry cough.
As the disease develops, the pulmonary temperature rises sharply to 40 degrees, the cough becomes wet, sometimes with blood, shortness of breath and pain in the chest area appear. Timely diagnosis of the disease and timely treatment can quickly relieve the patient from the pronounced symptoms of pneumonia and the disease itself.
Under no circumstances should you self-medicate and lower your temperature below 38 degrees. Very low temperatures, as well as too high temperatures, aggravate the course of the disease. Doctors at the Yusupov Hospital recommend lowering it to a certain norm.
How many days does a fever last for pneumonia?
With pneumonia, a temperature of up to 39 degrees can persist for up to three days until the antibiotics prescribed by the doctor begin to take effect. In case of development of bilateral pneumonia, a temperature of up to 38 degrees can persist for up to two weeks. Such patients should be under the close supervision of a physician.
In the inpatient conditions of the Yusupov Hospital, the patient’s condition is monitored by highly qualified doctors, which makes it possible to exclude the development of complications. Also, if necessary, the doctor can always adjust the course of treatment and prescribe the necessary procedures for a speedy recovery.
The atmosphere in the wards of the Yusupov Hospital bears little resemblance to the atmosphere of state hospitals. All conditions have been created here to make the patient feel as comfortable as possible. All rooms are equipped with modern furniture and equipment, and have access to WI-FI. Each room has a private bathroom. The patient can always call a medical professional into the room using the call button.
Sometimes pneumonia can occur in the body without an increase in body temperature. In this case, the patient may not even suspect a serious illness. As a rule, with this development of the disease, the temperature subsequently rises very rapidly and reaches high limits. In this situation, the patient needs the help of a specialist. It is almost impossible to stop the development of the disease on your own.
It is impossible to say for sure how long the temperature lasts during pneumonia. Everything is individual and depends on many factors.
Types of pneumonia
Pneumonia without fever
Quite a dangerous type - asymptomatic pneumonia
, not manifested by elevated temperature. There may be no symptoms other than weakness. The body may not signal a disease even by coughing. Often this situation is a consequence of a weak immune response and the body’s inability to fight the virus.
Doctors advise paying attention to a person’s complexion; often a characteristic spotted blush appears on the background of very pale skin. Human breathing occurs with a whistle. When moving, shortness of breath and rapid pulse appear. The body is weak, gets tired quickly, chest pain and difficulty breathing are possible.
Asymptomatic pneumonia is dangerous because there is no cough and excess sputum does not come out. The infectious process stagnates in the lungs. Often this is a consequence of untreated colds or bronchitis.
For diagnosis, a chest x-ray is taken in 2 projections. The main sign of pneumonia is limited darkening of the lung tissue.
Polysegmental pneumonia
Bilateral polysegmental pneumonia affects several segments of the tissue of both lungs. It often affects children under one year of age and people with reduced immunity. The first stage of the disease may be asymptomatic or similar to ARVI
.
The development of symptoms of bilateral pneumonia - cough with sputum, shortness of breath, moist rales in the lungs, chest pain. This clinical picture is accompanied by an increase in temperature to 39-40 degrees, fever, increased sweating, tachycardia, headaches and changes in consciousness. With polysegmental pneumonia, sputum stagnates in the bronchi, which is difficult to drain due to progressive edema.
Focal pneumonia
An acute form of the disease with an inflammatory process occurring in a limited area of lung tissue (lung lobe). Symptoms of this form of pneumonia are fever, dry cough or slight sputum production, chest pain, and general weakness.
Often focal pneumonia is a complication of acute respiratory infections and bronchitis. This diagnosis increases during seasonal ARVI and influenza.
Body temperature rises to 38-39 degrees, sometimes it can be normal or have subfebrile values. Breathing quickens to 25-30 units, tachycardia manifests itself up to 110 beats. per minute
Fever usually stops 3-5 days after the start of antibiotic therapy. The period for relieving symptoms of focal pneumonia is 3-4 weeks.
Atypical pneumonia
Atypical pneumonia is an infectious disease accompanied by inflammation. This lung damage is caused by uncharacteristic pathogens - viruses, mycoplasmas, chlamydia and other numerous infectious agents.
This type of disease differs from “typical” pneumonia caused by bacterial coccal flora. Symptoms of atypical pneumonia:
- weakness,
- headaches and muscle pain,
- dyspnea,
- sweating,
- fever,
- cough.
To diagnose atypical pneumonia, it is necessary to determine the causative agent, for which PCR, RIF, and culture methods are used. An X-ray of the lungs is necessary. After identifying the pathogen, drug treatment is prescribed.
Atypical pneumonia caused by coronavirus is called acute respiratory syndrome (SARS). It is difficult to identify the infectious agent, and therefore to treat, due to the rapid mutation of the virus.
SARS infection occurs through airborne droplets. The incubation period is from 3 to 10 days. Depending on the pathogen, atypical pneumonia is divided into:
- Q fever,
- chlamydial pneumonia,
- legionella pneumonia,
- severe acute respiratory syndrome,
- mycoplasma pneumonia, etc.
Among the drugs recommended for the treatment of atypical pneumonia, the main one is ribavirin, which is now widely used to treat pneumonia caused by coronavirus. After the start of treatment, corticosteroids are introduced into the protocol; in severe cases, blood plasma transfusion is used. Treatment includes oxygen therapy, diuretics to prevent pulmonary edema, infusion therapy to relieve intoxication, symptomatic treatment for cough and symptoms of respiratory syndrome.
Community-acquired pneumonia
Community-acquired pneumonia is not associated with the patient's hospital stay. This diagnosis is made when the patient was not hospitalized or contracted pneumonia no less than 14 days after discharge or no later than two days after hospitalization.
Community-acquired pneumonia develops due to the impact of pathogenic microorganisms on the respiratory tract. This occurs when the patient has a complicated history of cardiovascular or metabolic diseases, an unhealthy lifestyle, weak immunity, advanced age, or severe hypothermia.
Pneumococci, streptococci, Haemophilus influenzae, staphylococci, chlamydia, legionella, and adenoviruses enter the human body at home, in crowded places through airborne droplets, entering the air when coughing and sneezing from the patient’s respiratory tract.
With reduced immunity and other unfavorable factors, the drainage system of the lungs is disrupted, and pathogenic microorganisms remain in them, causing an inflammatory process.
For the treatment of community-acquired pneumonia, drug therapy is used according to a protocol associated with the pathogen identified by bacteriological analysis.
Viral pneumonia
Viral pneumonia is caused by respiratory viruses, often familiar to us. These are influenza viruses, parainfluenza, enteroviruses, adenoviruses. Therapy for viral pneumonia is the use of antiviral and symptomatic drugs.
Symptoms of viral pneumonia are acute:
- a sharp increase in temperature,
- intoxication syndrome,
- severe productive wet cough,
- pain in the lungs.
Diagnosis of viral pneumonia is based on laboratory data.
Often viral pneumonia develops against the background of acute respiratory viral infection, in which case the typical symptoms of a respiratory disease are aggravated for several days by high fever, cyanosis, cough with rusty-colored sputum, wheezing in the lungs and chest pain.
Viral pneumonia caused by the influenza virus is often bilateral, with focal lesions in the lungs. Moreover, among viral pneumonia there are often cases of a relatively mild form of the disease with moderate symptoms and rapid recovery.
In childhood, viral pneumonia accounts for 90% of all types of this disease. In severe cases, viral pneumonia is severe in children:
- with high temperature
- vomiting,
- intense symptoms of intoxication,
- lack of appetite or complete refusal to eat,
- severe cough.
In severe cases, hospital treatment is prescribed.
Adults suffer from viral pneumonia less often than children (the percentage of viral pneumonia among other types of disease does not exceed 35%). Viral pneumonia most often affects people over 65 years of age. The incidence of the disease increases in the autumn-winter period.
Lobar pneumonia
Lobar pneumonia is an acute infectious disease. This diagnosis is made when one or more lobes of the lung are affected when fibrinous effusion and fibrinous deposits on the pleura appear in the alveoli.
The most common causative agent of lobar pneumonia is pneumococcus, and the main cause of the disease is decreased immunity.
The disease begins acutely, with an increase in temperature to 39 degrees, chills, and chest pain. A dry cough is replaced by the production of “rusty” sputum. Shortness of breath is pronounced. Breathing is harsh, with wet and dry wheezing. Subsequently, vocal tremors are detected due to impaired breathing. Lobar pneumonia can be accompanied by irregular heart rhythms, a drop in blood pressure and severe headaches.
At the end of the acute phase of the disease, breathing returns to normal, although a rapid pulse and decreased blood pressure may still bother the patient.
Croupous pneumonia is a disease of adults, and it is treated in a hospital in the therapy department.
Pneumonia without cough
Pneumonia is most often accompanied by a characteristic set of symptoms, but it happens that the disease occurs in a latent form. Asymptomatic pneumonia is difficult to diagnose, since the patient cannot recognize the health problem based on obvious signs. Latent pneumonia can occur without fever and even without wheezing in the lungs.
Most often, people over 60 years of age suffer from latent pneumonia.
Immune system dysfunction is the main cause of asymptomatic pneumonia. It can also develop due to improper use of cough medications during a respiratory illness. If sputum is poorly excreted, it accumulates in the lungs and becomes a breeding ground for pathogenic flora.
A complication after influenza, bronchitis or ARVI is another cause of asymptomatic pneumonia.
If there is no cough, but there is a suspicion of illness, you need to listen to the following symptoms:
- increased weakness,
- decreased performance,
- severe headaches.
The patient exhibited severe sweating, rapid pulse, shortness of breath and chest pain. The temperature may rise.
To detect pneumonia with hidden symptoms, it is necessary to carry out in-depth diagnostics, which will help determine the stage and severity of the disease.
Interstitial pneumonia
Interstitial pneumonia is an inflammatory process in which the walls of the alveoli and the connective tissue of the parenchyma are affected. The disease is caused by infectious agents:
- mycoplasma,
- chlamydia,
- pneumocystis,
- legionella,
- respiratory viruses,
- herpes virus.
Interstitial pneumonia can also be a reaction to dust. Interstitial pneumonia is focal or diffuse and may involve a lobe or the entire lung.
Symptoms of the disease:
- dyspnea,
- dry cough,
- chest pain,
- temperature up to 38 degrees,
- cardiopulmonary failure.
The disease is determined using CT and laboratory diagnostics.
The disease can be severe, with a high probability of pulmonary fibrosis. At risk:
- smokers,
- HIV-infected,
- people with alcoholism.
Interstitial pneumonia can occur in a chronic form (more than 12 months), during which time the patient is limited in activity, suffers from severe shortness of breath and high fatigue. Severe weight loss is common.
Treatment includes oxygen therapy, corticosteroids, and cytostatics. Due to decreased respiratory function, mechanical ventilation is prescribed.
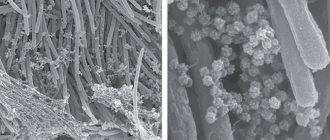
Pneumocystis pneumonia
Pneumocystis pneumonia is a type of atypical pneumonia. Its infectious agents are the protozoan microorganisms Pneumocystis. The disease is transmitted by airborne droplets and often develops in people with a compromised immune system.
At risk for PCP:
- aged people,
- HIV patients,
- tuberculosis,
- patients with blood diseases,
- patients taking immunosuppressants.
The disease may have relapses. In particular, in patients with HIV infection in the AIDS stage, the probability of recurrent disease is 25%.
Pneumocystis enter the body through the respiratory tract, actively multiply, and provoke the appearance of large amounts of mucus and metabolic products. Once in the blood, infectious agents provoke the formation of specific antibodies. The alveoli are affected, gas exchange is disrupted. In conditions of respiratory failure, pulmonary fibrosis develops, subsequently emphysema and pneumothorax.
Symptoms of the disease first look like signs of ARVI or laryngitis. The period of the first stage is up to 10 days. Weakness, severe cough, weight loss in the second stage of the disease are intensified by severe shortness of breath. The skin acquires a bluish tint. The cough becomes productive with sputum that is difficult to clear.
The third stage brings relief of symptoms, but wheezing in the lungs and symptoms of weakness may persist for a long time.
Treatment of Pneumocystis pneumonia occurs in a hospital and includes antibacterial and symptomatic treatment.
Mycoplasma pneumonia
Mycoplasma pneumonia is an atypical pulmonary infection. Infectious agent – Mycoplasma pneumoniae. This type of pneumonia is characterized by:
- obsessive cough,
- low-grade fever,
- chest pain and muscle pain,
- abdominal pain and disturbances in the gastrointestinal tract.
Mycoplasma pneumonia most often affects children, adolescents and adults under 35 years of age.
With a high prevalence of the disease, mycoplasmas are not very stable in external conditions. They respond to changes in temperature (in particular, heating) and do not grow in dry environments.
These microorganisms often cause bronchitis, bronchial asthma, and they can also cause non-respiratory pathologies (otitis, encephalitis, meningitis, anemia).
The incubation period for mycoplasma pneumonia is usually 12-14 days. The disease rarely begins acutely, more often it is the appearance of symptoms of laryngitis, less often - bronchitis. Weakness, sweating, and fever up to 38 degrees also accompany the onset of the disease.
Complications of mycoplasma pneumonia can include:
- Stevens-Johnson syndrome,
- Guillain-Barre syndrome,
- myelitis,
- encephalitis,
- meningitis.
If the disease is recognized at an early stage, it can be cured within two to three weeks. For treatment, macrolides, fluoroquinolones, bronchodilators, expectorants are prescribed; in the recovery stage, immunomodulators, physiotherapy, massage, and breathing exercises are prescribed.
What is the temperature for pneumonia in adults
With pneumonia, body temperature varies from 37 to 38 degrees. If it lasts longer than 5 days, the patient should definitely consult a doctor.
If the temperature exceeds 39-40 degrees, this indicates that inflammation is increasing and the body cannot cope with the pathogen on its own. If the temperature rises to 40 degrees, you should call an ambulance.
Focal inflammation, that is, when the infection does not affect the entire lung, but only parts of it, can manifest itself as low-grade fever. In patients with high immunity and in elderly patients, there may be no increase in temperature at all.
How to reduce fever with pneumonia
You can lower your body temperature only with medications that have been approved by your doctor. Only a doctor can determine the effectiveness of taking medications for pneumonia in each individual case. As a rule, mild antipyretic drugs are prescribed at temperatures above 38 degrees. To reduce fever in adult patients, the following medications are prescribed:
- ibuprofen;
- nurofen;
- paracetamol;
- aspirin;
- Citramon.
You can rub with a towel soaked in cool water or a water-vinegar solution, paying special attention to the temples, forehead, and bends of the arms and legs.
The patient can use folk remedies on his own. When it’s hot, a raspberry drink helps a lot; linden tea will increase sweating. Drinks made from honey, lemon, currants, rose hips, as well as citrus fruits contain large amounts of vitamin C, which improves immunity and serves as a good assistant in the fight against pneumonia.
Treatment of pneumonia
How many days does pneumonia take to be treated?
The duration of treatment depends on the underlying causes of pneumonia. Pneumococcal infection can be defeated in 7 days. Legionella or staphylococcus causes pneumonia, which must be treated for at least three weeks. Pseudomonas aeruginosa will force you to undergo therapy for up to forty-two days. Complicated pneumonia must be treated for up to two months.
Focal pneumonia is treated faster than lobar polysegmental pneumonia. In the first case, the clinical picture becomes favorable within ten days, in the second, treatment takes about a month.
Bilateral pneumonia in an adult. Duration of treatment
When predicting the treatment of bilateral pneumonia in an adult, one should always take into account chronic diseases, the state of immunity and the causes of the disease. Patients with severe metabolic damage, diabetes mellitus, high hypertension, and heart disease have a chance of longer treatment and long-term rehabilitation after pneumonia. The clinical picture can reveal symptoms of pneumonia up to two months from the start of therapy, while a strong body can recover in one month.
Clinical guidelines
The latest clinical recommendations for the treatment of pneumonia are contained in the letter of the Ministry of Health of the Russian Federation dated March 6, 2020 N 30-4/I2-2702 “On the algorithm for providing medical care to the adult population with community-acquired pneumonia.” The document is relevant and defines the procedure for diagnosis and treatment of all types of community-acquired pneumonia (those that developed outside the hospital, or those diagnosed in the first 48 hours from hospitalization). The letter defines the rules for hospitalization for pneumonia, the timing of the start of antibacterial therapy after diagnosis, the classification of forms of the disease by severity, based on symptoms.
Clinical guidelines provide as much detailed information as possible about the diagnosis and treatment of pneumonia, but they are addressed to doctors and medical personnel. Anyone can find them online and read them to raise awareness about the disease, but under no circumstances should you engage in self-diagnosis and self-medication according to prescribed antibacterial therapy protocols
. At the first signs of discomfort, you should consult a doctor.
Treating pneumonia at home
Clinical guidelines provide clear criteria for hospitalization of patients with pneumonia. Patients with a mild form of the disease and many of those suffering from moderate pneumonia without a significant medical history are treated at home.
The main rules for treating pneumonia at home:
- compliance with the antibacterial therapy protocol;
- keeping to bed for the first days and drinking plenty of fluids to relieve symptoms of intoxication;
- the need to get up every 5-6 hours and move slightly for up to 20 minutes;
- after normalization of the clinical picture, short walks are indicated;
- nutritious but light food;
- complete cessation of smoking;
- maintaining indoor air humidity within 60-70%.
Treatment with folk remedies
When treating pneumonia with medications, many also resort to folk remedies that support treatment. The most common of them are medicinal herbs. Herbal decoctions help with expectoration, reduce inflammation, and relieve bronchospasms.
Herbs reduce swelling and have a diuretic effect, activate the immune system, which well supports the therapeutic course.
It is useful to drink drinks rich in vitamin C: decoction of rose hips, cranberries, lingonberries, viburnum.
When treating pneumonia with folk remedies, garlic, honey are used, and various compresses and tinctures are made. With the abundance of folk recipes for the treatment of pneumonia, it is important to remember that consultation with a doctor is necessary in each case of their use
. Each folk remedy should be built into therapy and not interfere with its successful course. Therefore, if you want to resort to the help of traditional medicine, you should not overload the body and follow the principles of rationality and consistency with the main treatment protocol.
Temperature after pneumonia
After treatment for pneumonia, body temperature should return to normal. If it is elevated, this means that therapy was stopped prematurely and the focus of the pathogen continues to develop. The temperature often stays at around 37˚C. This may indicate a recurrence of pneumonia or an exacerbation of a chronic pathology.
The reason for the increase in temperature after pneumonia may also be immunodeficiency developed under the influence of antibacterial drugs. An elevated temperature may be evidence of viral, bacterial and fungal infections. The temperature rises to low-grade levels with tuberculosis, malignant neoplasms and HIV infection. The cause of elevated temperature may be intoxication or extrapulmonary complications of pneumonia.
In addition to fever, patients with pneumonia experience the following signs of illness:
- general weakness;
- decreased ability to work;
- fatigue and lethargy;
- chills;
- dry or wet cough;
- decreased appetite;
- breathing disorder.
These symptoms indicate that complete recovery has not occurred.
Examination at elevated temperature
If you have a fever after pneumonia, you should immediately consult a doctor at the Yusupov Hospital. Patients with elevated body temperature are examined by a therapist, prescribe an examination and organize a consultation with related specialists - otolaryngologist, cardiologist, nephrologist, neurologist, endocrinologist. The gynecologist also conducts an examination, because pneumonia can worsen chronic inflammatory diseases of the reproductive organs.
In order to determine whether there are residual effects of pneumonia, large-frame fluorography or lung radiography is performed at the Yusupov Hospital. If the clinical picture of the disease does not correspond to radiological data, computed multislice tomography is performed. During bronchoscopy, the doctor examines the bronchial mucosa, assesses the condition of the bronchial tree and performs a biopsy. The resulting tissue sections are sent for histological examination.
A clinical blood test allows you to establish laboratory signs of chronic inflammation or an allergic process. Using immunological and serological research methods, doctors at the Yusupov Hospital determine the presence of pathogens of atypical pneumonia. They can cause a temperature rise to 37 degrees or higher.
How to eliminate fever after pneumonia?
Until the cause of the increase in body temperature after pneumonia is determined, patients are not prescribed antipyretic drugs. They can mask the true clinical picture of the disease. Patients are advised to drink up to 2.5 liters of fluid per day. This helps remove toxins from the body. Preference should be given to purified water, raspberry and cranberry juice. Linden tea with honey has a good antipyretic effect.
Patients are advised to avoid contact with infectious patients and take walks in the fresh air. You should not overcool and avoid drafts. In most cases, after suffering from pneumonia, the temperature drops to normal levels on its own.
If the doctors at the Yusupov Hospital determine that the increase in temperature is a complication of pneumonia, they prescribe treatment for the corresponding pathology. To increase the overall reactivity of the body, immunomodulators are used:
- interferon;
- levamisole;
- zymosan;
- diuciphone;
- t-activin;
- Thymalin.
To prevent viral infections, it is recommended to inhale phytoncides. In order to restore the body's nonspecific resistance, vitamin and mineral complexes are prescribed, biogenic stimulants and adaptogenic agents are used (schizandra and ginseng tinctures, aloe juice, liquid extract of Eleutherococcus). Sometimes body temperature returns to normal after treatment of carious teeth or diseases of the ENT organs.
If you have a fever after pneumonia, call the Yusupov Hospital, where doctors will conduct an examination, identify the cause of the increase in body temperature and prescribe effective therapy. Pulmonologists take an individual approach to the treatment of each patient.
Acute respiratory viral infections
Date of publication: April 23, 2021. Category: Doctor's advice.
Four faces of the cold
It has long been an open secret for experienced doctors: even during a flu epidemic, its closest associates—respiratory viral infections—account for the lion’s share of cases. There are more than 300 species of such provocateurs that make us sneeze and cough.
At first glance, there is not much difference between them. And yet, there are some distinctive features in the behavior of “cold” viruses.
Provocateur No. 1 - parainfluenza
Its special features are a voice that is hoarse beyond recognition in a person who has it, and a “barking” cough. But in general, parainfluenza is milder than influenza, with a low temperature, which, if it rises, then gradually. True, if adequate measures are not taken in time, parainfluenza can develop into laryngitis, bronchitis and even pneumonia. Parainfluenza is especially dangerous for babies, in whom this virus can cause false croup, which can lead to the development of acute stenosis (edema) of the larynx. Therefore, it is so important to connect inhalation moisturizing respiratory tracts to traditional drug therapy in the treatment of parainfluenza. Parainfluenza lasts for about a week and a half.
Provocateur No. 2 - respiratory syncytial infection
Unlike parainfluenza, it manifests itself already when it affects the small bronchi and bronchioles. And this is the biggest insidiousness of a respiratory syncytial infection, which can drag on for two weeks or more. At the same time, the condition of the person who catches it often resembles an asthmatic one: the poor fellow suffers from suffocation (especially when exhaling), his lungs whistle in every possible way.
Those at risk include the elderly, young children (under three years old) and those with chronic illnesses.
Respiratory syncytial infection is especially dangerous for heart patients, allergy sufferers and people with pulmonary pathology. They carry this virus the hardest. Salvation lies in timely diagnosis, which in this case is best started with a chest x-ray.
Provocateur No. 3 - adenoviral infection
You have had a high fever for several days, your body is filled with lead, and you can feel enlarged lymph nodes on your neck and under your arms? Most likely, an adenovirus has “settled” in your body.
In addition to the symptoms listed above, a distinctive feature of this infection is the so-called “pharyngoconjunctival fever”, manifested by a feeling of pain in the eyes (first in one, then in the other), so strong that after a couple of days tears begin to flow like a river, and under the eyelids and noticeable white or grayish films appear in the corners of the eyes. Unlike influenza and parainfluenza, a cough with an adenovirus infection is usually wet. In young children, the disease is often accompanied by diarrhea (diarrhea).
Provocateur No. 4 - rhinoinfection
On its own, it does not pose any particular danger to the person who catches it, but by joining the flu or parainfluenza, for example, it becomes a champion in the production of snot. One of the most unpleasant complications of rhinoinfection is sinusitis. In order not to bring yourself to this state, it is important to start treating a runny nose as early as possible.
Fight according to the rules
Given the difficulty in diagnosing acute respiratory viral diseases, it is best to entrust it to a doctor. And, having started to follow his instructions, adhere to ten simple and effective rules for combating respiratory viral infections.
- One of the most important conditions is bed rest. Stay at home for at least a week. And the disease will pass faster, and you won’t “reward” those around you with it.
- Drink at least 2 liters of fluid per day. What it will be - tea, hot milk or mineral water - does not matter much. Intoxication products are removed from the body with fluid.
- During your illness, switch to a plant-based dairy diet. Such food will not require much energy from your body to digest it and will save energy to fight the scourge.
- If you have a fever, do not rush to bring it down. The rise in temperature itself is a natural phenomenon, a protective reaction to the introduction of foreign viruses and microbes into our body (the same as pain, vomiting, diarrhea). With the onset of a microbial attack in our head, special brain centers responsible for thermoregulation are irritated. This leads to an increase in temperature, which is uncomfortable not only for us, but also for the infection itself. Therefore, if the fever is tolerated normally and does not exceed 38 degrees, many doctors do not recommend bringing it down. By reducing it, we thereby reduce the body's defenses; In addition, aspirin, which is popular among people, can cause heartburn and stomach problems, and if you take effervescent tablets in the evening or at night, this can contribute to the formation of kidney stones.
- Don't forget about vitamins. Especially about vitamin C. It increases the production of interferon, stimulating the activity of the immune system. By the way, most of this vitamin is found in grapefruits. One grape a day - and your physiological norm of this vital vitamin is provided.
- Regularly moisten and ventilate the room. In a dry atmosphere, it is more difficult for the respiratory tract to resist infection.
- To avoid further spreading the infection, give up traditional cloth handkerchiefs, replacing them with disposable paper tissues or napkins, and also change towels and wash your hands more often. Especially after blowing your nose.
- Do not overuse vasoconstrictor drops. By pouring everything into their nose that can ease their pain, many become real drug addicts, not knowing the harm they are doing to themselves. The vessels very quickly get used to them and require an ever-increasing “dose”; the function of the cilia of the epithelium of the nasal mucosa, which removes mucus, is disrupted.
- Same with cough. In the first days of illness, when the cough is dry due to irritation of the respiratory tract, drinking and inhaling emollient and anti-inflammatory decoctions of chamomile, plantain, sage, marshmallow root, and linden blossom help. You can add a teaspoon of baking soda to a glass of the finished broth. When the cough “gets wetter”, it is better to use a decoction of herbs with a drying and expectorant effect - snakeweed, lingonberry and eucalyptus leaves, licorice and marshmallow roots, wild rosemary and yarrow.
- Do not take medications without consulting your doctor. Especially when it comes to antibiotics. They have no effect on viruses, and when used uncontrolled, they quickly develop drug resistance in pathogenic bacteria.
There are no children without snot
Both children and adults suffer from colds in the same way: the same runny nose, the same cough. But there are some peculiarities in treating children.
Dating time
In the first three years, children experience an average of 6–8 respiratory diseases per year. Children in large cities get sick up to 10 times a year. Children in nurseries and kindergartens get sick especially often. This is understandable - they encounter a lot of new infections brought from different families. But, since respiratory diseases leave behind immunity that lasts several years, by school time kindergarteners begin to get sick less often. And children at home in the first 7 years of life get sick less than “organized” ones, but in the first grades they get sick much more often.
Oh, temperature
Parents of a child with a cold are usually most concerned about fever. They want to bring her down at any cost.
There is no point in lowering the temperature if it has not reached 39 °C.
Firstly, most microbes and viruses stop reproducing at temperatures above 38°. In the past, some infections were even treated by artificially inducing fever.
Secondly, temperature is a valuable witness: with most viral infections that cause a cold, it lasts only 2-3 days, or even less, while with bacterial infections, such as otitis media or pneumonia, the high temperature will not subside even 4. and 5 days. And this symptom is a signal to the doctor that the child needs to be prescribed antibiotics. If you constantly lower your temperature, the doctor will not be able to make a correct diagnosis.
But there are exceptions to this rule. To reduce the temperature, starting from 38°, you need to:
- infants of the first two months;
- children who have previously experienced convulsions at high temperatures.
Home remedies
If you still need to lower the temperature:
- Give your child a diaphoretic drink: tea with honey or raspberries, with linden blossom. Offer to drink often, but little by little. Large amounts of liquid at one time may cause vomiting.
- Dry his body with a warm, damp towel. Water, evaporating, increases heat transfer. Do not use vinegar or vodka for wiping. After this procedure, the child will begin to tremble, trembling will again increase body temperature.
- The student can be put under a warm shower. But don't expect your temperature to return to normal right away. Both rubbing and showering will reduce it by 1–1.5 degrees.
- You need to remove the diaper from the baby and keep him naked for a couple of minutes.
Procedures for the panty
Treating a small patient is a real punishment. Either he won’t let it drop into his nose, or he doesn’t want to swallow the medicine. And you can do this:
Soak cotton wicks in cold drops or saline solution and insert them into your nostrils. What kind of tusks you got, just a sight for sore eyes.
Nobody wants to fight you? Does the baby want it? Then we'll make the same ones for him.
Mustard plasters are an unbearable torture for children: thin skin is burned before the chest has time to warm up. Boil the potatoes in their jackets, wrap them in plastic, and then in a towel. One potato on the chest, one on the back, the baby sits in his mother’s arms and listens to fairy tales - what a pleasant treatment. Inhalations will help with coughs and sore throats. Breathe over the steam of freshly boiled potatoes, covered with a towel, together, of course, head to head, imagining that you are hiding in a warm house from an evil wolf.
Colds in children are an inevitable phenomenon; there is no need to make a tragedy out of them; children who are not susceptible to colds have not yet been invented.
Important
Aspirin is contraindicated for children under 15 years of age with acute viral infections. Under no circumstances should you give it to them to reduce their temperature. Aspirin can cause Reye's syndrome - severe damage to the liver and brain. The fatal outcome of this disease exceeds 50%.
Caution won't hurt
Some of the most popular medications today are immune boosters.
Most people treat them like ordinary vitamins, believing that these drugs are absolutely safe and beneficial to everyone without exception. But is it?
Is your immune system fine?
Many knowledgeable doctors are sure: before prescribing immunomodulators to a patient, the doctor must:
- have on hand studies of the patient’s immune status;
- have a rationale for recommending the drug, confirmed by clinical and laboratory data;
- be familiar with the criteria for the effectiveness and safety of such drugs.
By the way, recently, after conducting a detailed examination of a group of frequently ill children, it turned out that only half of them have immune disorders. Bronchial asthma was found in 40%, and in 10% the diseases were associated with structural features of the respiratory system.
By the way
Most drugs used in immunology are only 10–15 years old, so long-term studies on their safety have not yet been conducted. But it is known that the production of several immunomodulators has already been closed abroad today, since it was discovered that they provoke the development of autoimmune diseases. Therefore, immunostimulating drugs should be used with caution and in no case should you prescribe them yourself.
Antibiotics: benefit or harm?
Antibiotics are completely powerless against viruses.
That is why these drugs are contraindicated for acute respiratory viral infections or influenza, hepatitis and some other acute infectious diseases. But, if ARVI is accompanied by a secondary infection, if there is a danger of bacterial pneumonia, antibiotics are necessary to protect the patient from complications.
However, the doctor must have serious reasons for this. Antibiotics may be prescribed if a high fever suddenly returns after it has been normal for several days.
Or the cough has intensified, shortness of breath has appeared - there are symptoms that indicate a bacterial infection.
What should I prescribe?
In case of an infectious disease, most often the doctor, having established a diagnosis, prescribes one of the drugs that are used to treat this particular disease. But in order to make a “targeted choice,” the doctor must know whether you are allergic (and to what exactly), chronic diseases, what antibiotics you were treated with before and when.
The fact is that bacteria quickly develop resistance to the drug, and after repeated use it is not able to cope with them. Therefore, in such situations, a second generation antibiotic is immediately prescribed, which has a wider spectrum of action. The effectiveness of the drug is assessed within three days from the start of treatment; if there is no change for the better, the antibiotic is canceled and another one is prescribed.
Important
Antibiotics should not be taken with milk - this interferes with the absorption of the drug in the intestines. To reduce possible adverse reactions, before taking the medicine you can drink half a glass of jelly; it envelops the intestinal mucosa, protects its beneficial microflora, but does not interfere with the absorption of the drug.
Autumn without colds
If you catch a cold at the very beginning, it is quite possible to cope with the disease with the help of folk remedies.
So that your throat doesn't hurt
- When discomfort in the throat begins, slowly chewing raw lemon, especially the zest, helps. So that essential oils and citric acid have time to act on inflamed mucous membranes, after chewing lemon, do not eat anything for an hour. Repeat the procedure two to three times a day.
- Fragrant violet is an excellent remedy for sore throat, pharyngitis and other inflammations of the mucous membrane of the upper respiratory tract. It is used in the form of a decoction or alcohol tincture. Decoction: pour 1 teaspoon of flowers with a glass of boiling water. Rinse and take 2 tbsp orally. spoons 4-5 times a day. Tincture: 1 tbsp. pour a spoonful of flowers with 100 ml of alcohol. Take 1 tbsp. spoon of tincture 3 times a day before meals. To prepare the rinse, dilute 10 ml of tincture with a glass of warm water.
- Spice lovers will love this warming cocktail: 4; cup cumin, pour 1.5 cups of hot water and bring to a boil. Strain, add 1 tbsp. a spoonful of cognac or vodka. Drink 1 tbsp. spoon of the mixture 3-4 times a day.
- Garlic inhalations. Crush a few cloves of garlic in a mug, lean over it and breathe for five minutes. First with the mouth, then with the nose.
- Gargling with freshly squeezed beet juice will help cope with inflammation of the mucous membrane of the throat.
- If your voice goes down, try anise infusion. Brew 1 teaspoon of anise seeds with a glass of boiling water and let it brew for 20 minutes. Drink a warm infusion of ¼ glass 3 times a day 30 minutes before meals.
Breathe deeper
- A runny nose that has just begun is treated with steam inhalations. Brew dry mint or eucalyptus leaves with boiling water and breathe over the steam for several minutes. These plants have a counterbalancing scorching effect and prevent the disease from developing.
- When your nose is stuffy and you don’t have drops on hand, you can make a medicine from what you can find in any home, namely, regular green tea.
The infusion is easy to prepare: pour 1 teaspoon of dry tea with a glass of boiling water. We wait for the tea leaves to brew and cool. We bury it in the nostrils so that the mucous membrane is washed abundantly with the solution. The procedure should be repeated 6–8 times a day.
Cough remedies
- Decoction of coltsfoot leaves: 1 tbsp. Brew a spoonful of coltsfoot leaves with a glass of boiling water, let it brew for 30 minutes and take 1 tbsp. spoon every hour.
- Apple tea: 2 tbsp. Pour a glass of water over spoons of chopped dried apples and boil for 10–15 minutes. Drink warm.
- Aloe with honey: Cut a few aloe leaves, chop and squeeze out the juice. Mix juice with honey in a 1:1 ratio. Take the mixture 1 teaspoon 3 times a day.
This remedy has an expectorant effect and relieves inflammation of the upper respiratory tract.
- Sage infusion: 2 tbsp. Pour a glass of boiling water over spoons of dry sage herb and leave for an hour. Take ½ glass of warm infusion 2-3 times a day.
- Lemon oil: Scald the lemon in hot water, then pass it together with the zest through a meat grinder, mix with 100 g of butter and 1 tbsp. spoon of honey. Lemon oil is a wonderful preventative that will protect you from colds.
- Milk with poppy seeds: If a cough prevents you from falling asleep, drink a glass of warm milk before bed, to which add 2 teaspoons of poppy seeds.
- Radish juice: Take a large radish, peel it, grate it and squeeze out the juice. Mix juice with 1 tbsp. spoon of honey and take 2 tbsp. spoons 2-3 times a day.
Increasing protection
During the cold season, all efforts should be directed toward strengthening the body’s defenses, which will help not get sick. These remedies are simple. Among them: Vitamins Drink a glass of orange or grapefruit juice on an empty stomach in the morning, and eat a salad with onions in the evening. This will help you strengthen your immune system and fight viruses that have entered your body. But this method of prevention is not suitable for people with a number of chronic diseases of the gastrointestinal tract. Additional sleep Lack of sleep reduces immune defense several times. Therefore, to reduce the risk of infection, increase your sleep time by 1-2 hours. Sometimes it is difficult, but it is better to refuse to watch your favorite TV series or go to the theater, where there is a high probability of contracting an infection. Acupressure Massaging active points in a clockwise direction provides toning of the body, while massaging in the opposite direction provides relaxation. Find the point at the intersection of the lines drawn from the thumb and index finger, in the recess of the hand. When you press on it, you should feel a slight pain. Make 50–100 massaging movements: clockwise in the morning, counterclockwise in the evening to quickly fall asleep. Herbs American scientists over the past ten years have studied several dozen plants that can affect the immune system and provide protection against ARVI. It turned out that only one thing has maximum and proven effectiveness: Echinacea purpurea. Taking an aqueous tincture of this plant for two weeks reduces the likelihood of getting the flu by 30%, and drinking it during illness reduces the duration of the illness by half. To ensure your protection, take Echinacea as a preventive measure - 20 drops morning and evening. Massive intake of echinacea in an emergency situation also produces results - 40 drops with an interval of 1-2 hours. Garlic therapy At the height of the cold season, you can’t do without garlic. Whether you like it in its natural form or prefer to make do with garlic oil capsules does not matter. Allicin, contained in garlic, works effectively in any company and is excellent at dealing with microbes. Homeopathy and adaptogens An excellent way to prevent influenza is homeopathic complexes. Taking eleutherococcus, ginseng, pantocrine and other adaptogens that increase the tone of the body's defenses also works well. Proper food Put off the idea of losing weight until spring. If during the cold season you deprive your body of necessary fat deposits, your immunity suffers first of all. Low-fat diets are especially harmful because the walls of lymphocytes and macrophages - our protective cells - are made of lipids. Including cholesterol, which many supporters of a healthy lifestyle are so terribly afraid of. Remember: your winter diet should contain enough protein of both plant and animal origin.
After all, immunoglobulins, which ensure the body’s resistance to diseases, are proteins whose synthesis requires the entire set of essential amino acids. But you shouldn’t overeat either. Excess fat suppresses the immune system. A large amount of proteins overloads the gastrointestinal tract and kidneys. Excess sugars are a direct path to obesity, which is an even greater enemy of the immune system than excessive thinness. Return
Temperature with pneumonia in children
At the onset of the inflammatory process, the child’s body temperature can be from 37.1˚C to 38˚C; in this case, low-grade fever is observed, the child experiences weakness, apathy, and refuses to eat. At the same time, in the morning the temperature in children with pneumonia can remain at around 36.6˚C.
This condition can persist for a week with strong immunity. However, parents with a slight rise in temperature may mistakenly begin treatment for acute respiratory infections without contacting a general practitioner. If a child’s fever persists for more than 4 days, you should immediately consult a specialist, since early diagnosis is the key to successful treatment.
Pneumonia in children can occur without fever, so if other symptoms of pneumonia appear, medical attention is required. In some cases, the temperature during pneumonia in children rises to 39˚С - 40˚С. If pneumonia is detected in a child during research, a long course of treatment is prescribed.
Under no circumstances should parents of a child adjust the course of treatment on their own, believing that prolonged use of certain medications can harm their child. Changing treatment without consultation with a doctor can lead to the disease developing into a chronic form.
Each patient - adult or child - should undergo a full comprehensive course of treatment prescribed by a doctor, which averages about two weeks. This will help you get rid of the disease and the complications it causes.
Is pneumonia contagious?
Whether pneumonia is contagious or not depends on its type and the causes of the disease. At the same time, it is impossible to become infected with pneumonia directly, but pathogenic microflora, having penetrated the body of another person, can become a source of the inflammatory process, including pneumonia.
Pneumonia can be caused by bacteria, viruses, fungi, and protozoa. A person poses the greatest danger to others at the initial stage of the disease, when he coughs and releases infectious agents with his cough.
But it is important to remember that even with infection, the development of the inflammatory process may not occur. Strong immunity prevents pneumonia from developing, and all the fight against the infectious agent occurs in the upper respiratory tract. In other words, the same infectious agent can cause different reactions in different people: from mild ARVI to severe pneumonia.
The risk of developing pneumonia is greater:
- in children under 1.5 years old,
- old people,
- for those who suffer from immunodeficiency,
- suffering from chronic pathologies of the cardiovascular system, bronchi and lungs, kidneys,
- in diabetics,
- allergy sufferers,
- smokers.
It is important to remember that some types of pneumonia are not contagious. These are those types of disease that are not associated with infection. For example, pneumonia caused by stagnation of fluid in the respiratory tract.
Treatment at the Yusupov Hospital
Pneumonia is a rather complex and unpredictable disease that requires compliance with all doctor’s instructions, thanks to which it is possible to prevent a sharp deterioration in the patient’s well-being and aggravation of the disease.
Yusupov Hospital in Moscow offers high-quality diagnostics and effective treatment of pneumonia. The specialists of our clinic, whose competence is confirmed by international certificates, will provide comprehensive support until the patient’s complete recovery.
Thanks to the clinic being equipped with modern diagnostic and treatment equipment, our doctors have the opportunity to obtain the most reliable research results and select a treatment method for pneumonia that is most effective for a particular type of disease.
The Yusupov Hospital has its own hospital, where patients can expect comfortable rooms, good nutrition, round-the-clock staff assistance and an individual approach. You can make an appointment with a doctor by calling the clinic.
Drugs for the treatment of pneumonia
Antibiotics for pneumonia
Patients with mild pneumonia are treated at home. It can usually be cured with tablets or suspensions. The doctor prescribes β-lactam antibiotics (amoxicillin, amoxin, flemoxin solutab). For older patients or with severe chronic diseases, protected penicillins and fluoroquinolones (amoxiclav, flemoclav solutab, avelox) are prescribed.
To treat patients with severe and extremely severe pneumonia, drugs of the 3rd and 4th generations are used, which have a bactericidal effect that completely destroys the pathogen cells. Among the representatives of the third generation cephalosporins are oral and parenteral forms. In the first subgroup, suprax in capsules and suspensions, cedex in capsules and specracef in capsules, cefditoren, ceftazidime, cefoperazone,
To destroy mycoplasmas in pneumonia, macrolide antibiotics that are active against atypical flora, tetracyclines - reserve drugs, doxycycline (Unidox Solutab) are suitable.
Adequate treatment of pneumonia cannot do without antibiotics. This is the only modern and effective measure to eliminate the cause of the disease - microorganisms. All drug prescriptions must be supervised by a doctor; self-medication is fraught with aggravation of the disease and the development of bacterial cell immunity to the effects of antibiotics.