Intrauterine pneumonia is an acute inflammation of the pulmonary parenchyma of infectious origin, diagnosed on the basis of typical radiographic and clinical symptoms in the first 72 hours of a baby’s life. In the structure of infant mortality from infectious pathologies, neonatal pneumonia consistently ranks second after sepsis, which is due to late verification (confirmation of diagnosis) and the lack of timely treatment aimed at eliminating the cause of the disease. The traditional treatment regimen for pneumonia in a newborn child includes intensive antibacterial treatment taking into account the identified pathogen, artificial ventilation (for health reasons) and restoration of the water and electrolyte balance of the baby’s body.
Features of the bronchi and lungs in the newborn and fetus
The fetal lungs do not contain air, but it begins to carry out pulmonary movements already at the 23rd week of pregnancy. Before this period, due to the functional and anatomical immaturity of the lungs, gas exchange does not occur in them. At the time of birth, the baby's lungs are filled with amniotic fluid, which, with the first breath, is absorbed into the space between the alveoli and blood. In premature infants, the realization of the first breath is difficult, since the immaturity of the respiratory system is accompanied by metabolic disorders and an incompletely formed heart and blood vessels.
Reasons for the tendency of newborn children to pneumonia:
- immaturity of the nervous system and pulmonary components; poor functioning of the ciliated epithelium of the bronchi;
- narrowness of the airways, complicating the process of air passage;
- decreased cough reflex;
- poor development of the intercostal muscles, which leads to a decrease in the excursion (difference in circumference between exhalation and inhalation) of the chest.
Obstetric risk factors for congenital pneumonia: prolonged fetal hypoxia, resuscitation measures during labor, infectious diseases of the woman in labor, premature rupture of amniotic fluid, long anhydrous period.
Perinatal risk factors: asphyxia at birth, low weight, morphological and functional immaturity of the infant due to prematurity.
Types of disease
There are several classification signs of pneumonia in an infant:
- the causative agents of the disease are viral, fungal and bacterial pneumonia, which requires treatment with antibiotics;
- according to the degree of tissue damage in the lungs, they are divided into focal (small areas), total (one whole lung) and bilateral (both lungs at once), while the process from focal to bilateral develops very quickly;
- According to the method of infection, they distinguish intrauterine, acquired, aspiration (entry of amniotic fluid into the child’s respiratory system) and birth (passage of the infected birth canal).
The type of disease is determined in order to select the appropriate treatment.
Etiology and pathogenesis
The etiological spectrum of pneumonia in newborns in 70% of cases is interconnected with the nature of infection:
- transplacentally . Pneumonia in newborns infected in utero through the placenta manifests itself after the introduction of rubella virus, chickenpox, herpes simplex, CMV, tuberculosis microbacteria or pallid spirochete;
- perinatal _ Intrauterine pneumonia, which develops in the fetus 2-3 weeks before birth, is caused by chlamydia, mycoplasmas, anaerobes, Haemophilus influenzae, intestinal bacteria or herpes simplex virus;
- postnatally . Pneumonia in newborns during the postpartum period occurs due to infection with respiratory viruses, Staphylococcus aureus, candida, and intestinal bacteria. Influenza and parainfluenza viruses can only provoke bronchitis or an infection of the respiratory tract (upper), however, against the background of these diseases, in 40-45% of cases, unilateral pneumonia or a more severe pathology – bilateral pneumonia “starts”.
Pneumonia in premature infants is classified as a special group. Intrauterine pneumonia in such newborns is caused by class B streptococci. Early infection in them is characterized by an extremely severe course, leading to death in 40% of cases, 3 times higher than the same indicators in premature infants in the absence of infection.
Clinical picture
Intrauterine pneumonia manifests itself as cyanosis, depression or excitability of the central nervous system, and failure of temperature control. Possible swelling of the wings of the nose, shallow rapid or “grunting” breathing, symptoms of respiratory failure, cough with foamy discharge, hemorrhagic signs, hemodynamic disorders, jaundice. Moist rales are heard against the background of weak breathing. All these clinical symptoms are nonspecific and can be observed in infants who are born with low birth weight, so if a woman gave birth to a premature baby and observes similar symptoms, it is necessary first of all to exclude respiratory distress syndrome in the baby.
Intrauterine infection - symptoms and treatment
The manifestation of infection directly depends on the timing of infection. For all intrauterine infections there are a number of common symptoms [1][6]:
- The first 2 weeks after conception are spontaneous early abortions.
- From 2 to 10 weeks - gross malformations incompatible with life (severe heart defects, brain defects, etc.), as a result, spontaneous abortion (miscarriage) or frozen pregnancy.
- From 10 to 28 weeks - early fetopathies (diseases and malformations of the fetus). A miscarriage or frozen pregnancy is possible.
- From 28 to 40 weeks - late fetopathies. Development of inflammation in different organs.
- During childbirth - inflammation in organs (myocarditis, pneumonia, etc.).
The presence of an intrauterine infection in a child can be suspected during childbirth. Infection may be indicated by the discharge of cloudy amniotic fluid with an unpleasant odor or meconium (newborn feces). Children with intrauterine infection are often born prematurely and develop asphyxia (oxygen starvation). From the first days, such children also experience:
- jaundice;
- low birth weight (less than 2.5 kg);
- various skin rashes;
- respiratory disorders (pneumonia, respiratory distress syndrome);
- lethargy;
- pale skin;
- febrile conditions or hypothermia (body temperature below 36.0 °C);
- cardiovascular failure;
- neurological disorders (decreased muscle tone, convulsions, bulging large fontanel, high-pitched scream, increased excitability);
- decreased appetite, delayed weight gain;
- gastrointestinal symptoms (regurgitation, vomiting, bloating, enlarged liver and spleen).
Herpes
Herpes infection in a newborn is caused by herpes simplex virus types 1 and 2 (herpes simplex and genital). The highest risk of infection of the fetus is when the mother becomes infected during pregnancy. With an exacerbation of a pre-existing infection, the probability of infection is no more than 5% [1].
Congenital defects are rare and may include hypoplasia (underdevelopment) of the limbs, microcephaly (significant reduction in the size of the skull), retinopathy (damage to the retina), and skin scars.
Clinical manifestations of herpes types 1 and 2 in newborns:
- prematurity;
- pneumonia;
- chorioretinitis (inflammation of the choroid and retina);
- rashes on the skin and mucous membranes;
- jaundice;
- meningoencephalitis (damage to the membranes and substance of the brain).
The most severe herpetic infection occurs when generalized forms occur (disruption of all organs and systems) and when the central nervous system (CNS) is affected. In case of infection during childbirth, the infection appears after 4-20 days (incubation period).
Late complications in children who have had a herpetic infection in utero: recurrent herpetic lesions of the skin and mucous membranes, central nervous system disorders, retardation in psychomotor development, encephalopathy (brain damage).
Chicken pox
If a woman had chickenpox during the period from 8 to 20 weeks of pregnancy, in 30% of cases a miscarriage or stillbirth occurs. Most children who survive develop skeletal malformations and neurological abnormalities [1]. The later the signs of congenital chickenpox appear, the more severe the course: skin rashes, hepatitis, pneumonia, myocarditis, intestinal ulcers. When a rash appears in the first 4 days of life, the disease is not severe.
Late complications in children who have had chickenpox in utero: developmental delay, diabetes mellitus, loss of vision, increased incidence of malignant tumors.
Cytomegalovirus infection
Intrauterine infection with cytomegalovirus is possible if a woman is infected for the first time, as well as if reactivation of a cytomegalovirus infection occurs (transformation of an inactive form of the virus into an active one). Infection during childbirth and breastfeeding is possible.
Congenital defects (if a pregnant woman is infected in the early stages): microcephaly, atresia (absence) of the biliary tract, paraventricular cysts (near the ventricles of the brain), polycystic kidney disease, heart defects, inguinal hernia.
Clinical manifestations of congenital cytomegalovirus infection:
- low birth weight;
- jaundice;
- enlarged liver and spleen;
- rash in the form of hemorrhages on the skin;
- pneumonia;
- chorioretinitis, keratoconjunctivitis (inflammation of the cornea and conjunctiva);
- neurological disorders (meningoencephalitis, cerebral calcifications around the ventricles);
- blood in stool;
- thrombocytopenia (decreased platelet count), anemia;
- severe bacterial infections [14].
Late complications develop, as a rule, after the neonatal period: cerebral palsy, delayed psychomotor development and speech development, difficulties in school, damage to the kidneys, visual and hearing organs [1].
Measles
If you are infected with measles in the early stages of pregnancy, birth defects and miscarriages may develop.
Clinical manifestations in newborns:
- rash - occurs in 30% of children if the woman was sick during childbirth;
- prolonged jaundice;
- increased incidence of pneumonia if immunoglobulin G is not administered.
Parvovirus infection
Congenital defects are not common, but there is a high risk of fetal death if the mother becomes ill in the first half of pregnancy.
Clinical manifestations in newborns:
- fetal edema with severe anemia;
- thrombocytopenia.
ARVI
The most common causes of intrauterine infections are the following infections: adenovirus, influenza, parainfluenza, RS virus.
Congenital defects occur, but there are no characteristic ones.
Clinical manifestations are noted from the first days of life:
- catarrhal phenomena (swelling, inflammation and redness of the mucous membranes): rhinitis, pharyngitis, conjunctivitis, bronchitis, pneumonia;
- possible increase in body temperature (above 38 °C);
- poor weight gain;
- possible jaundice;
- Bacterial infections are often associated.
Late complications of past infection:
- hydrocephalus (dropsy of the brain) - accumulation of cerebrospinal fluid in the intracranial spaces, manifested by an increase in the size of the head;
- delayed psychomotor development;
- frequent ARVI;
- glomerulonephritis - damage to the glomeruli of the kidneys (after parainfluenza) [1].
Coxsackie virus
Congenital defects (if infected early): heart and kidney defects.
Clinical manifestations in newborns:
- low birth weight;
- diarrhea;
- rash;
- fever;
- signs of ARVI (nasopharyngitis);
- pneumonia.
Possible late complications of the infection: encephalopathy, myocardial dystrophy (damage to the heart muscle), chronic pyelonephritis [1].
Viral hepatitis B
Congenital defects and diseases: atresia (absence) of the biliary tract, hepatitis.
Clinical manifestations in newborns:
- prematurity;
- low birth weight;
- weight loss;
- diarrhea;
- enlarged belly;
- dark urine;
- discolored stool;
- acute, subacute and chronic hepatitis.
Possible late complications of the infection: delayed psychomotor development, cirrhosis of the liver, liver tumors.
Syphilis
One of the negative trends in recent years is the predominance of cases of congenital syphilis in women diagnosed with early syphilis. Congenital syphilis can be prevented by identifying and treating those infected during pregnancy. Therefore, pregnant women are repeatedly examined for this disease (blood on RW). Early congenital syphilis appears at 2-4 weeks of life, often even later.
Congenital defects: not typical.
Clinical manifestations in newborns:
- A typical triad is: rhinitis (runny nose), pemphigus (rash on the body), enlarged liver and spleen.
- Characterized by poor weight gain, anxiety, causeless shuddering, and central nervous system damage.
Possible late complications: hydrocephalus, encephalopathy [1].
Toxoplasmosis
There is a high probability of infection of the fetus if the infection is “fresh”. If infected in the 1st trimester, the probability is 15%, in the 2nd trimester - 30%, in the last trimester - more than 50%.
Congenital defects: malformations of the eyes (microphthalmia), brain (microcephaly, hydrocephalus), skeleton, heart.
Clinical manifestations in newborns. Three flow options are possible:
- Acute - increased body temperature, enlarged lymph nodes, enlarged liver and spleen, edema, jaundice, diarrhea, skin rash.
- Subacute - the main signs of encephalitis.
- Chronic - hydrocephalus, calcifications in the brain, seizures, blurred vision.
Late complications: encephalopathy with oligophrenia (mental retardation), intracranial hypertension, epilepsy, eye and hearing damage (up to deafness and blindness) [1][3].
Chlamydia
The risk of transmission of infection to an infant at birth from an infected mother is 60-70%. The disease does not appear immediately, but after 5-14 days.
Congenital defects are not common.
Clinical manifestations in newborns:
- purulent conjunctivitis with severe edema;
- nasopharyngitis;
- otitis;
- pneumonia;
- urethritis.
Late complications of a previous infection: frequent and prolonged acute respiratory viral infections.
Rubella
If the mother is infected in the early stages, the pregnancy must be terminated [7]. Infection of a pregnant woman in the first months, especially before 14-16 weeks, leads to spontaneous abortion, stillbirth, and the development of multiple and gross defects in the fetus. Before planning a pregnancy, it is necessary to be examined: if a woman does not have antibodies, then she must be vaccinated against rubella.
Congenital defects: heart defects, eye defects, deafness. These are the main signs of congenital rubella. When infected with rubella during a long period of pregnancy, there may be no congenital heart defect, only damage to the organs of hearing and vision is possible.
Other clinical manifestations:
- prematurity;
- dropsy of the brain (hydrocephalus);
- enlarged liver, spleen;
- thrombocytopenic purpura, etc.
Possible late complications: disability, hydrocephalus, deafness, blindness, retardation in psychomotor and speech development, mental retardation.
Mycoplasmosis
Mycoplasma infection occurs more often during childbirth. When mycoplasmosis is detected in pregnant women, therapy is carried out after the 16th week of pregnancy, which reduces the incidence of morbidity in newborns.
Congenital defects are possible, but there are no characteristic defects for mycoplasma infection.
Clinical manifestations in newborns:
- prematurity;
- pneumonia;
- pale skin;
- respiratory distress syndrome;
- skin rashes (like small hemorrhages);
- meningoencephalitis.
Late complications of the infection: hydrocephalus, encephalopathy [1].
Additional symptoms of the disease in children with intrauterine pneumonia:
- regular regurgitation, refusal to eat;
- fatigue during breastfeeding;
- fever, pronounced shortness of breath;
- increased bleeding, sclerema;
- enanthema/exanthema (rash on mucous membranes);
- symptoms of toxicosis, cardiovascular abnormalities.
The consequences of pneumonia in newborns can be extremely severe. Some infectious agents (staphylococci, Pseudomonas aeruginosa) provoke early decaying infiltrates with destructive cavities in the lungs and purulent pleurisy. The prognosis is worsened by decreased immunity and poor efficiency of bronchial cleansing due to aspiration of food or cystic fibrosis. Toxic complications (disorders of the heart muscle and central nervous system, microcirculation) depend on the severity of the pathological process and the adequacy of the treatment. After pneumonia, abscesses, pneumothorax, atelectasis, otitis media, sepsis, sinusitis, and blood clots may occur.
Consequences of congenital pneumonia
If the causative agent of pneumonia quickly causes destruction of lung tissue, then complications in the form of abscess and gangrene of the lung are possible. Microorganisms entering the child’s blood cause sepsis. Systemic complications such as hemorrhagic syndrome, hemodynamic disorders, disseminated internal coagulation syndrome, and acute cardiovascular failure may develop. Complications from the respiratory system also develop - pleurisy, atelectasis, pneumothorax. After congenital pneumonia, a child may develop heart defects, develop a chronic form of infection and intellectual impairment.
Diagnostic measures
Diagnosis is based on the results of laboratory, clinical, anamnestic and radiological data. Radiography is of priority, since the symptoms of pneumonia in newborns are nonspecific. It is very important to correctly assess the medical history, highlighting the infectious causes of the disease.
Diagnostic criteria:
Basic:
- seeding the child and the woman in labor with the same pathogenic microflora in the first 24 hours of life;
- the presence of infiltrative shadows on the radiograph;
- development of pneumonia against the background of aspiration syndrome during the first 72 hours of life.
Auxiliary:
- the presence of fluid in the pleural cavity from the first day of life;
- signs of inflammation identified during histology of the placenta;
- increased concentration of immunoglobulin M in blood serum;
- enlarged liver and spleen;
- the presence of sputum mixed with pus during tracheal intubation in the first 72 hours of the baby’s life;
- confirmed infections in the mother;
- increased bronchovascular pattern on the x-ray in combination with reduced transparency of the pulmonary field;
- negative dynamics in the blood test on days 2-3 of life;
- leukocytosis against the background of a shift to the left of the leukocyte formula on the first day of life.
The diagnosis of “congenital pneumonia” is made when at least one main diagnostic sign or three auxiliary signs are identified.
Diagnosis of congenital pneumonia
The main methods for diagnosing congenital pneumonia are laboratory and instrumental research methods. They can be taken at partner clinics.
Changes in laboratory data that may indicate congenital pneumonia are not specific. In newborns, the number of blood cells normally increases to ensure normal cellular respiration, and on the fifth day a physiological leukocyte crossover occurs. Congenital pneumonia may be supported by an increase in the number of leukocytes over time and the absence of leukocyte crossover on the fifth day of the baby’s life. This indicates the bacterial nature of pneumonia and allows us to exclude the viral etiology of pneumonia.
Since the main source of infection is the mother, doctors at the Yusupov Hospital prescribe an examination to determine the type of pneumonia causative agent in the child. To do this, a serological study of maternal blood is carried out to determine antibodies to certain infections. The level of antibodies of the immunoglobulin class G and M is determined. At the Yusupov Hospital, laboratory assistants use special reagents that make it possible to determine the level of these antibodies. If the level of immunoglobulin G is elevated, this means that the virus cannot be involved in the development of pneumonia in a child, since it only indicates an old infection. If immunoglobulins M, which are markers of an acute infectious process, are detected, there is a high probability that the fetus is also infected. Women also undergo a bacteriological examination of a vaginal smear
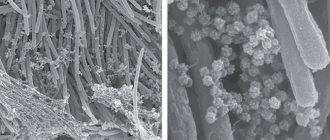
X-ray signs of congenital pneumonia in the initial stages of the disease are collapse (atelectasis) of the lungs and increased vascular pattern. Over time, inflammatory and infiltrative changes of a confluent nature appear. Differential diagnosis of congenital pneumonia is carried out with hyaline membrane disease and aspiration syndrome, diaphragmatic hernia, congenital malformations of the lungs, heart pathology and injuries of the central nervous system, which are accompanied by respiratory failure.
Treatment
The therapeutic regimen includes symptomatic, etiotropic and pathogenetic treatment, organization of appropriate nutrition and care.
Stages:
- antibacterial therapy . Antibiotics are prescribed immediately, taking into account previous experience with drugs of this class. Treatment usually begins with drugs that have a broad spectrum of action. At the second stage, therapy is carried out with drugs of a directed spectrum of influence. Starting medications for antibiotic therapy of early infection are a combination of Ampicillin and Cephalosporin. If a pathogen is identified, antibiotic treatment is carried out in accordance with the antibiogram data;
- immunocorrective therapy . Indicated in the presence of immunological abnormalities, human immunoglobulin is used intravenously;
- respiratory therapy . With its help, the necessary alveolar ventilation and adequate gas exchange are maintained, the risks of barotrauma are minimized, and desynchronization is eliminated;
- infusion therapy . Provides the required level of water and electrolyte balance with mandatory monitoring of postnatal maturation of the child’s renal function.
Complex treatment is implemented taking into account the individual characteristics of the baby’s health condition, which allows you to quickly stop inflammation in the respiratory tract, reduce the time of artificial ventilation, and prevent the development of life-threatening complications. A sick child must be provided with constant care: feed formula or breast milk from a tube until respiratory problems disappear completely, carefully care for the skin, create comfortable indoor conditions that prevent the baby from overheating or hypothermia. Treatment is carried out in a hospital under the supervision of doctors, rehabilitation after an illness is carried out within 12 months - during this entire period the child must be registered with a pediatrician.
Prevention:
- eliminating, if possible, all provoking and predisposing risk factors;
- thorough examination and health improvement of women planning pregnancy, relief of inflammatory foci before conception;
- monitoring the course of pregnancy and fetal development, excluding factors potentially dangerous for the intrauterine development of the child, screening studies, competent management of childbirth;
- prevention of birth injuries;
- implementation of epidemiological and sanitary measures in the maternity hospital, compliance with the incubation regime (for premature babies);
- limiting contact of a newborn with infectious patients.
Pneumonia is a dangerous disease that can subsequently lead to bronchopulmonary dysplasia, frequent respiratory and cold infections, bronchitis, and a decreased immune response. Considering the high mortality rate from pneumonia and its complications among newborns, treatment should be timely and rational - this allows to achieve a positive result of therapy and improves the prognosis of the disease.