Bile in the stomach (duodenogastric reflux)
Duodenogastric reflux is the reflux of the contents of the duodenum into the stomach cavity. Normally, after a certain period of time after food enters the stomach, a portion of bile is released into the lumen of the duodenum, aimed at further, more thorough digestion of the food bolus. The presence of bile creates an alkaline environment in the cavity of the duodenum. At the border of the stomach and duodenum there is a pyloric sphincter, which prevents the movement of food in the opposite direction and separates the acidic environment of the stomach from the alkaline environment of the duodenum. If the function of the sphincter is impaired, for example, if it is not fully closed, the alkaline contents of the duodenum enter the stomach. Burning has an irritating effect on the gastric mucosa, which, when exposed to it regularly, causes a chronic inflammatory process called reflux gastritis.
What is bile
Bile is a bitter-tasting liquid that can be of different shades of yellow depending on its location in the body. It is constantly produced by liver cells. There is a place in the body where this fluid accumulates.
To store bile reserves, humans have a gallbladder. In ancient times, doctors placed the role of bile in the human body on the same level as the importance of blood. Doctors claimed that there was a connection between bile and character and temperament. Later, scientists refuted this connection, but still a person with a bad character is called bilious.
The storage of bile reserves has a volume of 30-50 ml. On average, a person contains from 0.5 liters to 1.5 liters per day.
Composition of bile
| Name | hepatic | cystic |
| water | 97,5% | 86% |
| cholesterol | 0,15% | 0,6% |
| slime | No | a large number of |
| bile pigments | 0,5% | 4,1% |
| bile acids | 0,6% | 7% |
| dry residue | 2,5% | 14% |
When the liver produces fluid, it turns golden yellow. When the composition in the gallbladder changes, it turns dark brown. The amount of water in the bile storage decreases, so all substances are there in a more concentrated state. In addition, the walls of the organ secrete a large amount of mucus. These are the main differences between bladder fluid and liver fluid.
Treatment
Treatment should be comprehensive and include measures to normalize lifestyle, diet and diet, as well as drug therapy. If possible, eliminate physical and emotional stress that negatively affects the motility of the gastrointestinal tract. Long breaks in meals, consumption of fatty, extractive foods, marinades, smoked meats, and coffee are unacceptable. Avoid smoking, drinking alcohol and carbonated drinks. Drug therapy is selected by a gastroenterologist depending on the severity of symptoms and examination results.
Duodenogastric reflux, or the reflux of duodenal contents back into the stomach, is an extremely common digestive disorder. The symptoms that indicate this pathology are subjectively interpreted by many as “heartburn” or “indigestion,” which indicates their low specificity. An accurate diagnosis can only be made by a specialist after a thorough examination. If you experience discomfort associated with eating, we recommend that you contact Professor Gorbakov’s Clinic for specialized help.
Normally, food enters the oral cavity, moves down the esophagus into the stomach, and then enters the duodenum. Here it mixes with bile, which ensures the emulsification (breakdown) of fats and the absorption of most of the nutrients. The unilateral evacuation of food into the duodenum is supported by the reflexive opening and closing of the pyloric sphincter (pylorus). It also prevents retrograde (backward) flow of the bolus.
Improper functioning of the sphincter (its insufficient locking), as well as hypertension in the duodenum associated with chronic duodenitis, can cause bile to flow back into the stomach - duodenogastric reflux.
Often this disorder provokes the presence of inflammatory processes in the stomach (gastritis), duodenum (duodenitis), gallbladder (cholecystitis, biliary dyskinesia), pancreas (pancreatitis), and surgical interventions, namely:
- cholecystectomy;
- gastric resection;
- vagotomy;
- gastroenterostomy;
- enterostomy.
Place of choleretic drugs in clinical practice
Bile is an isosmotic fluid consisting of water, electrolytes, organic substances (bile acids and salts, cholesterol, conjugated bilirubin, cytokines, eicosanoids, etc.) and heavy metals, in particular copper. The total amount of bile produced by the liver per day averages 600 ml. The main organic components of bile are bile acids, which come from two sources.
- Primary bile acids (cholic, chenodeoxycholic) are synthesized from cholesterol in hepatocytes.
- Secondary bile acids (deoxycholic, lithocholic) are formed from primary bile acids in the intestine under the influence of bacteria.
Tertiary bile acids (sulfometacholic, ursodeoxycholic) can also be formed in the liver and intestines, which, like secondary ones, participate in the enterohepatic circulation.
Bile performs two important biological functions in the body:
- removal from the body of lipophilic components that cannot be utilized and excreted in the urine;
- secretion of bile acids, which are involved in the digestion of dietary fat and the absorption of its hydrolysis products.
The main components of bile as biliary secretion are presented in Table 1, and as biliary excretion in Table 2.
Biliary excretion is the only way to remove plant sterols such as sitosterol, as well as xenobiotics present in plants, from the body, preventing their accumulation in the body. All of them, as well as a number of lipophilic drugs - metabolites of fat-soluble vitamins and steroid hormones - in the hepatocyte are conjugated with glutathione, sulfates, glucuronic acid, and less often with glucose, xylose, glycine or taurine and are secreted into bile. These components of bile, and primarily plant sterols, due to conjugation with glutathione, increase the concentration of organic anions in the canaliculi and participate in the formation of a bile fraction independent of bile acids, and thus have a choleretic effect.
The formation of bile consists of the following stages:
- capture from the blood of a number of its components (bile acids, bilirubin, cholesterol, etc.) at the level of the basolateral membrane;
- metabolism, as well as the synthesis of new components and their transport in the cytoplasm of hepatocytes;
- their release through the canalicular (biliary) membrane into the bile canaliculi;
- entry of bile into the intrahepatic biliary system (bile ducts);
- its accumulation and concentration in the gallbladder;
- entry into the small intestine, absorption of its components and their entry into the enterohepatic circulation.
Through the basolateral membrane of hepatocytes from the blood plasma (from the spaces of Disse) bile acids, amino acids, unconjugated bilirubin, glucose and a number of endogenous and exogenous xenobiotics, including drugs, plant sterols and xenobiotics, enter the cytoplasm of hepatocytes. These processes are carried out due to the presence of Na+-K+-ATPase in the basolateral membranes, as well as specific and nonspecific carrier proteins for organic anions that have cross-reactivity. The functioning of Na+-K+-ATPase ensures the energy potential and ionic balance of the cell, as well as the normal fluidity (permeability) of cell membranes.
In the hepatocyte, two primary bile acids are synthesized from cholesterol: cholic and chenodeoxycholic, which are conjugated with amino acids - glycine or taurine. Conjugation ensures their solubility in water even at acidic pH values, makes them resistant to precipitation by calcium ions and reduces their permeability through cell membranes. Primary conjugated and deconjugated bile acids also enter the hepatocyte from the enterohepatic circulation. The former are unchanged, and the latter, after reconjugation, are again secreted into bile. Secondary bile acids - deoxycholic and lithocholic, which are products of microbial metabolism from cholic and chenodeoxycholic acids, respectively, enter the hepatocyte from the enterohepatic circulation and are conjugated. Deoxycholic acid binds to glycine or taurine and circulates along with primary bile acids.
Lithocholic acid, along with glycine and taurine, is also conjugated with sulfates, which sharply reduces its absorption and entry into the enterohepatic circulation. The latter is of great biological importance, namely: maintaining the integrity of hepatocytes and biliary epithelium. Less commonly, ursodeoxycholic acid, which is a product of microbial modification of primary bile acids, is included in the enterohepatic circulation. Its maximum content in the general pool of bile acids does not exceed 5%.
Intracellular transport of bile acids from the basolateral to the canalicular membrane of the hepatocyte is carried out by cytosolic proteins (3-α-hydroxysteroid dehydrogenase, etc.). The endoplasmic reticulum and Golgi apparatus are also involved in this process. Great importance is attached to the transcytosolic vesicular transport of bile acids, bilirubin and lipid-containing substances. The transit time of bile components from the basolateral to the canalicular membrane is about 10 minutes.
Canalicular secretion is the most important step in the formation of bile. Bile components enter the canaliculi in four ways:
- active transport of simple molecules with the participation of ATP-dependent pumps;
- exocytosis of lipid- and protein-containing vesicles;
- vesiculation of phospholipid molecules from the surface of canalicular membranes induced by bile acids;
- passive flow of fluid from the spaces of Disse through tight intercellular junctions.
Excretion of bile components from hepatocytes is carried out with the participation of ATP-dependent transport proteins that are capable of moving bile components from the cytoplasm into the lumen of the tubules against a concentration gradient.
As a result of their functioning, bile acids and their salts, as well as a number of other osmotically active substances (glutathione, bicarbonates), enter the tubules. The latter are involved in the formation of bile fractions dependent and independent of bile acids, each amounting to 225 ml/day. Water diffuses into the tubules along an osmotic gradient from the sinusoids through tight intercellular junctions, on average 150 ml/day.
Those compounds that are actively transported into the canaliculi from hepatocytes and participate in the formation of bile are designated as primary components of bile (conjugated bile acids, organic anions, etc.). They are not able to pass through the intercellular junctions of the tubules. The primary components of bile, and primarily bile acids, have choleretic activity. Molecules that enter the canaliculi passively through intercellular connections are designated as secondary components of bile. They contain water, electrolytes, glucose, and calcium ions.
Bile flow in the canaliculi is ensured by active canalicular secretion and contraction of pericanalicular actin filaments, which are induced by conjugated bile acids. From the canaliculi, bile through the intermediate canaliculi of Hering enters the extralobular bile ducts, which, connecting with each other, form the lobar and then the common bile duct.
During the passage of bile through the intrahepatic bile ducts, its composition changes: water diffuses into the lumen through the intercellular connections of the ductal epithelium; cholangiocytes absorb glucose and some organic acids; Glutathione is hydrolyzed to amino acids, which are partially absorbed. When unconjugated bile acids appear in bile, the latter are absorbed passively by cholangiocytes and enter the hepatocyte through the periductular capillaries (cholehepatic circulation of bile acids). Under the influence of secretin and glucagon, active secretion of bicarbonates occurs and an increase in the content of IgA and mucus is noted.
During the interdigestive period, the bulk of bile enters the gallbladder, where it is concentrated as a result of the absorption of water, electrolytes, including calcium ions. This absorption leads to activation of the Na+/H+ exchanger, as a result of which bicarbonates are replaced by CO2 and the pH level of bile decreases. Mixed micelles are stored in bile, which include a fairly large number of molecules, but they have the same osmotic potential as monomers.
As a result, gallbladder bile can contain anions in concentrations exceeding 200 mmol and remain isotonic.
During a meal, the gallbladder empties and remains contracted for 30–45 minutes, and the sphincter of Oddi remains in a relaxed state. During this period, the mucous membrane secretes water and electrolytes into the lumen of the gallbladder, which helps flush out all accumulated substances from it, and liver bile continuously flows into the duodenum. In the absence of a gallbladder, during the interdigestive period, hepatic bile is deposited in the proximal parts of the small intestine, mainly in the duodenum, and after eating it enters the distal parts. Excessive content of weakly concentrated bile in the duodenum with the development of duodenal hypertension is one of the mechanisms for the development of pain and dyspeptic disorders in patients who have undergone cholecystectomy.
Once bile enters the small intestine, the metabolism and transit rate of each of its components differ significantly. Thus, the transit rate of bile acids is significantly lower than that of other bile components. Only a small part of bile acids (no more than 5%) is lost in feces; the bulk of them is absorbed and enters the enterohepatic circulation.
In the proximal parts of the small intestine, part of the bile acids conjugated with glycine is absorbed passively. The bulk of bile acids is actively absorbed with the participation of a specific carrier protein (an ideal transporter for bile acids), which is localized on the apical surface of enterocytes.
In the distal small intestine and colon, bile acids undergo microbial deconjugation and are readily absorbed.
Entering the portal blood, the bulk of bile acids (70–90%) bind to albumin and return to the liver, where they are captured by hepatocytes, conjugated and transported again to the biliary system and intestine. As a result of the above enterohepatic circulation, a pool of bile acids is formed in the body, equal to approximately 5 mmol with a half-life of 2–3 days.
The leading role in the regulation of choleresis belongs to the gastrointestinal hormones - cholecystokinin and secretin. Cholecystokinin is secreted by hormonal cells of the duodenum. Its main effects are:
- to increase the flow of hepatic bile;
- contraction of the gallbladder;
- relaxation of the sphincter of Oddi;
- increased pancreatic secretion;
- decrease in pressure in the biliary system.
The production of cholecystokinin, and therefore the production of bile, is stimulated by fats, especially with the presence of long-chain fatty acids (fried foods), proteins, acids, constituent components of choleretic herbs (alkaloids, protopine, sanguinarine, essential oils, fats, etc.), cholinergic stimuli .
Secretin, produced in the duodenum, stimulates the secretion of water, electrolytes and bicarbonates by the epithelium of the biliary and pancreatic ducts and potentiates the effects of cholecystokinin. The main stimulators of secretin secretion are hydrochloric acid, fats, bile acids and, possibly, plant alkaloids and sterols.
In the regulation of bile formation and bile excretion, pressure in the bile ducts plays a certain role (normally 15–20 cm of water column). When the pressure in the ducts increases, the secretion of bile decreases, and when the level of 35 cm of water column is reached, the secretion of bilirubin, bile acids and water completely stops.
Drug correction of bile formation processes is possible at its various stages.
- Influence on the formation of bile acid-dependent and independent bile fractions. Stimulation of the production of the first of these is possible with the use of drugs containing bile acids (allochol, lyobil, cholenzyme, festal, panzinorm, etc.). An increase in the volume of the second of them can be achieved by prescribing drugs containing alkaloids, sterols, essential oils of plants, increasing the concentration of bound and free glutathione and other anions in the canaliculi (fumaria, immortelle flowers, corn silk, tansy flowers, St. John's wort, etc.) or chemical preparations synthesis, increasing osmotic pressure and promoting fluid flow into the canals (oxaphenamide, cyclone).
- Influence on the production of cholecystokinin and secretin in order to either increase or decrease the flow of bile into the intestine. Thus, the intake of fatty, fried, sour and dense foods, as well as preparations containing bile acids, vegetable fats and essential oils, alkaloids, bitterness, stimulate the production of cholecystokinin and secretin and, accordingly, bile and pancreatic secretions.
- Reducing pressure in the gallbladder and bile ducts is an important mechanism that activates bile formation. Consequently, drugs that stimulate the contractile function of the gallbladder and/or reduce the tone of the sphincter of Oddi have an indirect choleretic effect. Most drugs with the above properties realize their effect through an increase in the production of cholecystokinin (hymecromone, polyhydric alcohols, magnesium sulfate, hepabene, berberine bisulfate, coumarins, etc.).
- Influence on the content of bile salts in the small intestine, aimed at both reducing and increasing them in the enterohepatic circulation. Thus, the administration of drugs containing bile acids and excessive bacterial growth in the proximal small intestine increase the pool of bile acids in the enterohepatic circulation and reduce their synthesis in hepatocytes. The binding of bile acids in the intestine, for example, by cholestyramine or aluminum-containing antacids, and a decrease in their entry into the liver with portal blood, on the contrary, increases their synthesis from cholesterol.
In clinical practice, drugs that enhance the production of bile and its flow into the intestines are widely used. Choleretic drugs can have both positive and negative effects on the functions of the digestive tract if all indications and contraindications for their use are not taken into account.
The mechanism of action of choleretic drugs is:
- to improve digestive processes associated with the participation of bile acids in the hydrolysis of neutral fat and stimulation of the production of pancreatic secretions by cholecystokinin, secretin and bile acids;
- activation of intestinal motor function due to the direct action of bile salts, including their osmotic effect, leading to fluid flow into the intestinal lumen and an increase in intraluminal pressure, as well as the influence of intestinal hormones (cholecystokinin, etc.);
- prevention of excessive bacterial growth in the small intestine, which is ensured by the bactericidal effect of bile acids, prevention of intestinal stasis, normalization of digestive processes;
- increasing the circulation of bile in the gallbladder, which reduces its lithogenicity, ensures sterility, stimulates the contractile function of the gallbladder and coordinates the tone of the sphincter of Oddi;
- excretion from the body of endogenous and exogenous xenobiotics, cholesterol, maintaining the balance of microelements;
- normalizing the absorption of fat-soluble vitamins and preventing the development of osteoporosis.
When prescribing a choleretic agent, the following must be clearly understood:
- indications and contraindications for its use and expected therapeutic effect;
- what is the mechanism of action of the prescribed drug: it stimulates the production of a bile fraction dependent or independent of bile acids or it affects the contractile function of the gallbladder;
- Are hepatocytes in a particular patient capable of capturing, synthesizing and secreting bile components into the biliary system (canaliculi, ducts). The presence of dystrophy, necrosis, a decrease in the number of functioning hepatocytes, as well as hepatocellular cholestasis is taken into account;
- the patency of the intrahepatic and extrahepatic biliary system is preserved or impaired. Stimulation of bile formation in the presence of cholestasis leads to the accumulation of bile components in hepatocytes and their necrosis;
- how the functional state of the digestive organs will change, as well as the structure of the mucous membrane of the small and large intestines with the receipt of additional amounts of bile.
Depending on the leading mechanism of action, choleretic drugs are divided into drugs that enhance the production of bile - choleretics and ensure the flow of bile from the gallbladder into the intestine - cholekinetics. Choleretics include two groups of drugs:
- containing bile acids and their salts: components of bovine bile (allochol, cholenzyme, festal, etc.) or essential bile acids - chenodeoxycholic, ursodeoxycholic;
- products of plant origin and chemical synthesis: hepabene, sibektan, immortelle flowers, hymecromone, etc.
The group of cholekinetics includes drugs that stimulate the contractile function of the gallbladder and reduce the tone of the sphincter of Oddi: magnesium sulfate, polyhydric alcohols, nicodine, hymecromone, domperidone, and a number of herbal drugs (hepabene, berberine, sibektan, etc.). Myotropic antispasmodics, relaxing the tone of the sphincters of the biliary tract and improving the flow of bile into the duodenum, can also formally be considered as choleretic agents. A number of choleretic drugs have combined effects: choleretic, cholecystokinetic and antispasmodic in relation to the sphincter of Oddi.
The main indications for the use of choleretic drugs are:
- normalization of digestive processes in a number of physiological and pathological conditions (in the elderly, after previous infections, in the presence of diseases of other organs and systems with malnutrition), in chronic gastritis with secretory insufficiency, etc.;
- primary (as independent diseases) and secondary (as one of the symptoms of the disease) dyskinesia of the gallbladder;
- chronic non-calculous cholecystitis without exacerbation;
- sphincter of Oddi dysfunction;
- hypomotor dyskinesias of the small and large intestines (drugs containing bile acids);
- liver disease without signs of activity and cholestasis.
Choleretic preparations containing salts of bile acids, as well as synthetic and plant origin, significantly increase the functional load on hepatocytes, deplete their content of detoxifying substances and antioxidants (glutathione, sulfates, etc.). This is especially true for multicomponent compositions of medicinal herbs (choleretic, laxative, sedative herbs), as well as herbal remedies of Chinese and Tibetan origin. When prescribing choleretic drugs, it is necessary to ensure that there is no blockade of bile flow at the stages “liver cell–intra- and extrahepatic biliary system”.
Absolute contraindications to the prescription of choleretic drugs are all types of cholestasis: intrahepatic (hepatocellular, canalicular, ductular) and extrahepatic with and without jaundice. An exception is the use of ursodeoxycholic acid for intrahepatic cholestasis.
When prescribing drugs containing bile acids, with the exception of ursodeoxycholic acid, it should be taken into account that they are contraindicated in active hepatitis and liver cirrhosis of any etiology, peptic ulcers and erosions of the mucous membrane of the gastrointestinal tract, pancreatitis and diarrhea not associated with steatorrhea. Choleretic herbal remedies should not be used for pancreatitis, except parenchymal (painless forms), for hepatitis and cirrhosis of the liver with the presence of activity and signs of hepatic cellular failure, for irritable bowel syndrome with a predominance of diarrhea.
For chronic liver diseases, the use of choleretic drugs, which include a hepatoprotector, in particular silymarin, is relevant. Silymarin is part of the flavonoid group. Numerous experimental and clinical studies have made it possible to clarify the basic mechanisms of action of this drug.
- Protection of biological membranes from toxins as a result of:
- inhibition of toxin uptake by hepatocytes;
- stabilization of cell membranes as a result of inhibition of phosphodiesterase, inclusion of phospholipids in them (membrane repair).
- An increase in the neutralizing function of hepatocytes is associated with:
- with an increase in the glutathione pool in the hepatocyte;
- increased activity of enzymes involved in the oxidation of xenobiotics (in particular, superoxide dismutase).
- The antioxidant effect is due to:
- binding of free radicals;
- inhibition of reactions of excessive lipid peroxidation as a result of inhibition of the enzyme lipoxygenase, reduction of malondialdehyde content and reduction of glutathione consumption.
- The antifibrotic effect is provided by the effect on β-growth factor and the expression of matrix genes on stellate cells.
- Increased protein synthetic function of the liver.
- Inhibition of cholesterol synthesis as a result of decreased activity of microsomal hydroxymethyl-CoA reductase.
- Anti-inflammatory and immunomodulatory effects due to a decrease in the activity of macrophage cells involved in the presentation of antigens.
Thus, the simultaneous administration of silymarin and choleretic drugs can neutralize the negative effect of the latter on hepatocytes and opens up the possibility of their use in toxicometabolic and other liver lesions that occur without cholestasis and in the absence of high activity and autoimmune disorders.
The choice of drug is determined individually, and in each specific case it is necessary to decide whether to prescribe a drug containing bile or a herbal remedy in the form of monotherapy or in complex treatment. Below are indicative treatment regimens for diseases of the biliary system using choleretic agents.
I. Hypomotor dyskinesia of the gallbladder with normal motor function of the gastrointestinal tract or in combination with gastro- and/or duodenostasis:
- prokinetics: metoclopramide or domperidone: 5-10 mg 3 times a day 30 minutes before meals or magnesium sulfate solution 5-10%, 1 tablespoon 2-4 times a day 10-15 minutes before meals;
- choleretic drugs containing bile acids, or of plant origin: allochol - 2 tablets 3 times a day 20 minutes after the end of a meal, or cholenzyme - 1-2 tablets 2-3 times a day with meals, or hepabene - 1-2 capsules 3 times a day 1 hour before or 1 hour after meals.
If there are symptoms of bacterial contamination of the small intestine, use antibacterial agents: furazolidone or ersefuril, or intetrix, or ciprofloxacin, or sulgin and others in standard doses for 5–7 days.
II. Hypomotor dyskinesia of the gallbladder and colon:
- prokinetics: metoclopramide or domperidone - 5-10 mg 3 times a day in combination with lactulose - 15-45 ml/day;
- choleretic drugs containing bile acids (allochol, cholenzyme, lyobil, etc.) in generally accepted doses.
III. Hypomotor dyskinesia of the gallbladder in combination with hypermotor intestinal function (diarrhea):
- hepabene - 1-2 capsules 3 times a day with meals;
- intestinal adsorbents (smecta, phosphalugel 1 hour after meals) in standard doses for a short time, for the period of diarrhea;
- hilak forte - 30-60 drops 3 times a day with meals; in combination with a probiotic (bifiform, or bifidumbacterin forte, or probifor, etc.);
- if indicated, use intestinal antiseptics for 5-7 days, followed by the administration of probiotics.
IV. Hypermotor dyskinesia of the gallbladder:
- antispasmodics: for rapid relief of pain - phosphodiesterase inhibitors (drotaverine, papaverine) or M-anticholinergic blockers (atropine, platiphylline, etc.) in standard doses, including parenteral administration;
- for course treatment: mebeverine (duspatalin) - 200 mg 2 times a day or meteospasmil - 1 capsule 2-3 times a day 15-20 minutes before meals;
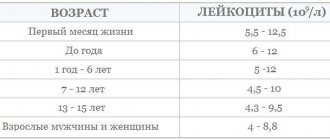
V. Chronic acalculous cholecystitis:
- exacerbation phase (pain, fever, leukocytosis): antibacterial drugs: ciprofloxacin - 500-1000 mg per day or doxycycline - 100-200 mg per day, etc.;
- antispasmodics;
- detoxification measures.
Duration of treatment - 7–10 days;
VI. Gallstone disease, stage I (presence of heterogeneous bile and/or biliary sludge in the gallbladder):
- hepabene - 1-2 capsules 3 times a day; 4 weeks as monotherapy. If there is no effect:
- ursodeoxycholic acid (ursosan, ursofalk) - 10-15 mg/kg/day, a single dose of the entire dose in the evening;
- antispasmodics in the presence of pain caused by dysfunction of the sphincter of Oddi.
VII. Sphincter of Oddi dysfunction (postcholecystectomy syndrome):
- antispasmodics (duspatalin, gimecromon, meteospasmil, etc.) in combination with therapeutic measures aimed at reducing intraduodenal pressure;
- a choleretic drug with a hepatoprotective effect, for example hepabene - 1 capsule 3 times a day for 2 weeks as monotherapy.
VIII. Toxic-metabolic liver damage without signs of intrahepatic cholestasis (fatty hepatosis, steatohepatitis in endocrine diseases, in pathology of the small intestine, chronic hepatitis of low activity of toxic origin, compensated cirrhosis of the liver). One of the components of complex therapy may be a combined choleretic drug with a hepatoprotective effect, prescribed for 2–4 weeks.
For all of the above disorders of the biliary system, along with the presented symptomatic therapy, etiological and pathogenetic treatment of the main and concomitant diseases is carried out, physiotherapeutic and balneological procedures are used, and a large role is given to dietary nutrition.
Thus, the problem of correcting bile formation and bile excretion is relevant. To solve it, a huge number of choleretic agents have been proposed, both with proven and insufficiently proven, as well as with unknown effectiveness. In addition to official drugs, a large number of herbs are used in clinical practice, including in the form of various herbs, which have not undergone serious controlled clinical testing of each of their components separately or in total for effectiveness and toxicity. In many literary sources, the choleretic effect of herbs is identified with the hepatoprotective effect and recommendations are given (which is unacceptable and dangerous) for their use in cholestasis, viral liver damage, chronic pancreatitis and other diseases for which choleretic drugs are contraindicated.
Literature
- Diseases of the liver and biliary tract: A guide for doctors / Ed. V. T. Ivashkina. — M.: LLC “Izdat. house "M-Vesti", 2002. - P. 416.
- Grigoriev P. Ya., Yakovenko A. V. Clinical gastroenterology. - M.: MIA, 2001. - P. 693.
- McNally P.R. Secrets of gastroenterology / Transl. from English - M.; St. Petersburg: ZAO Publishing House BINOM, Nevsky Dialect, 1998. - P. 1023.
- Mashkovsky M.D. Medicines: In 2 volumes - 14th ed., revised, corrected. and additional - M.: Novaya Volna Publishing House LLC, 2000. - T. 2. -P.540.
- Sherlock S., Dooley J. Diseases of the liver and biliary tract: Pract. hand: Per. from English / Ed. Z. T. Aprosina, N. A. Mukhina. - M.: Geotar Medicine, 1999. - P. 864.
- Yakovenko E. P. Intrahepatic cholestasis - from pathogenesis to treatment // Practitioner. - 1998. - T. 2. - No. 13. - P. 20-24.
- Hofmann AF Biliary secretion and excretion; The nepatobiliary component of the enteronepathic circulation of bile acids In Johnson L., Alpers D., Christensen I. et al. (eds).
- Physiology of the Gastrointestinal tract. - New York, Raven Press, 1994: 1556-1865.
- Johnson LR (ed) Gastrointestinal Physiology, 5th ed. - New York: Plenum Press, 1996: 720.
- Kuntz E., Kuntz HD. Hepatology, Principles and practice: history, morphology, biochemistry, diagnostics, clinic, therapy. - Berlin Heidelberg New York Springer - Verlag, 2000: 825.
- Rose S. (ed) Gastrointestinal and Hepatobiliary pathophysiology. - Fence Greek Publishing, LLC, Madison, Connecticut, 1998: 475.
E. P. Yakovenko, Doctor of Medical Sciences, Professor P. Ya. Grigoriev, Doctor of Medical Sciences, Professor N. A. Agafonova, Candidate of Medical Sciences, Associate Professor A. V. Yakovenko, Candidate of Medical Sciences, Associate Professor
RGMU, Moscow
Functions of bile
Not everyone knows what exactly the gallbladder does? What is the role of bile in the human body? What is it for?
Functions of bile:
- improves the functioning of pancreatic juice;
- dissolves fats entering the digestive system;
- helps the absorption of vitamins and nutrients;
- participates in intestinal function.
The main function of the liver is related to the breakdown of fats in the body. Without it, the body cannot process foods containing fat.
Structure of the liver
Liver and gallbladder
The performance of numerous functions is associated with the peculiarities of the internal structure of the liver. The dense membrane covering the liver under the peritoneum goes deep into the organ and divides it into prismatic lobules with a diameter of about 1.5 mm. The number of such hepatic lobules in humans reaches 500 thousand; they are the structural and functional unit of the liver (Fig. 2). In the lobule, liver cells (hepatocytes) are grouped in the form of radial plates, between which there are wide blood capillaries (sinusoidal), converging to the liver). Inside the radial plates, between two adjacent rows of hepatocytes, slits are formed, called bile ducts: bile produced by hepatocytes enters them.
Each liver cell is in contact with the wall of the blood capillary on one side, and with the lumen of the bile duct on the other. This structure allows hepatocytes to work in two directions: secrete bile into the bile ducts and send glucose, proteins, fats, vitamins, urea, etc. into the blood. Raw materials for the production of bile and numerous substances also enter through the capillaries with arterial and venous blood. As already mentioned, arterial blood arrives in the liver through the branches of the hepatic artery, and venous blood through the branches of the portal vein. In the wide capillaries of the hepatic lobules, arterial blood mixes with venous blood and flows very slowly, which promotes the exchange of substances between blood and hepatocytes. The capillary wall also contains special cells - stellate macrophages, which perform a protective function. They can capture from the blood and destroy various foreign particles, microorganisms, and damaged cells. Blood saturated with waste products of hepatocytes flows from the capillaries into the central vein of the lobule, and from there into larger veins, through which it is carried out of the liver and enters the inferior vena cava, i.e. returns to the general bloodstream.
Survey
When a patient complains of vomiting bile, a set of laboratory and instrumental methods is required to assess the condition of the gastrointestinal tract. An examination prescribed by a gastroenterologist is aimed at determining the pathological condition that caused the release of bile-colored vomit. The most valuable diagnostic methods are:
- Endoscopic examination
. FGDS is used to visualize the esophagus, stomach, and upper parts of the duodenum. The method effectively detects inflammatory changes in organs, ulcerative-destructive processes and dysfunction of muscle sphincters. Additionally, a biopsy of pathologically altered tissue areas is performed for histological analysis. - X-ray methods
. Taking X-rays of the gastrointestinal tract with oral contrast is aimed at studying the structure of all parts of the digestive tract, detecting nonspecific signs of inflammatory processes and peptic ulcers. For a detailed study of the hepatobiliary system, percutaneous or retrograde cholangiopancreatography is performed. - Duodenal sounding
. A study of the functional activity of the gallbladder with an assessment of the microscopic properties of bile is often decisive for making the correct diagnosis; it is carried out in all patients with vomiting with impurities of bile acids. If an infectious etiology of the disease is suspected, bacteriological culture is recommended. - Ultrasonography
. Survey ultrasound of the abdominal organs is used as a non-invasive express method that reveals signs of pathology in a specific part of the gastrointestinal tract. In case of biliary diseases, a targeted ultrasound of the gallbladder is performed to study its morphological features and detect possible stones in the lumen of the organ. - Stool analysis
. The appearance of bilious vomiting is often accompanied by various changes in the coprogram. By studying the macroscopic and microscopic properties of feces, the quality of food digestion is assessed, and signs of possible pathology of the biliary system are detected. If the patient has a general infectious syndrome, a bacterial culture of stool is performed.
Laboratory methods are used to clarify the diagnosis: an analysis is often prescribed to determine the content of free and bound bilirubin in the blood, determine the concentration of amylase and lipase, and search for specific antibodies. After excluding organic causes of the symptom, if the disorder is possibly functional, studies of the autonomic nervous system and the patient’s mental state can be carried out.
Ultrasound of the gallbladder
Bile ducts
The bile ducts, into which the bile produced by hepatocytes enters, begin blindly and are directed to the periphery of the hepatic lobule. Here they open into larger interlobular bile ducts, which, merging and gradually enlarging, form the common hepatic duct emerging from the porta hepatis (Fig. 3). Since bile is produced in the liver around the clock and enters the intestines only during digestion, a reservoir for storing bile is needed. The gallbladder serves as such a reservoir.
Location of the liver and gallbladder
Liver and gallbladder
The liver is located in the abdominal cavity, in the right hypochondrium, directly under the diaphragm (Fig. 1). The variety of functions leads to the fact that the weight of the liver in an adult reaches 1.5–2 kg (approximately 1/36 of body weight). In the fetus, the relative weight of the liver is twice as large (1/18 of body weight), and it occupies half of the abdominal cavity. The shape of the liver corresponds to the formations surrounding it: the upper surface is convex, like the dome of the diaphragm, and on the lower surface there are grooves and depressions from adjacent organs (right kidney, duodenum and colon). The surface of the liver is smooth and shiny from the peritoneum covering it, the color is red-brown (accumulations of fat give a yellowish tint). The ligaments of the liver fix it in a certain position and are folds of the peritoneum that passes to the liver from the diaphragm and neighboring organs. The ligaments divide the liver into lobes: the larger right one and the smaller left one.
On the lower surface of the right lobe of the liver, the gallbladder is located in a small depression (see Fig. 1). Nearby, in the transverse groove, there is the portal of the liver - the place where blood vessels, nerves enter the liver and where the bile ducts exit. The peculiarity of the liver is that it receives blood from two sources: like all organs, it is supplied with arterial blood (from the hepatic artery), and venous blood, flowing from the stomach, intestines, pancreas and spleen, comes from the portal vein. This blood contains nutrients from the gastrointestinal tract, which are neutralized in the liver and partially stored (as glycogen), insulin from the pancreas, which regulates sugar metabolism, and breakdown products of blood cells from the spleen, which are used to produce bile. Within 1 hour, all the blood passes through the vessels of the liver several times, “unloading” some substances here and being saturated with others. “The busiest harbor in the entire river of life” is called the liver.
Symptomatic therapy
You can reduce discomfort and the secretion of bile with the contents of the stomach by adjusting your diet. To reduce the frequency of vomiting, it is necessary to eat small portions 5-6 times a day, exclude fatty and smoked foods from the diet, which stimulate increased bile secretion. To relieve other dyspeptic disorders that accompany vomiting, it is recommended to consume more mucous soups and cereals, which protect the walls of the stomach from the aggressive effects of bile.
In order to reduce unpleasant symptoms until the causes of bile vomiting are established, you can use various herbal infusions (valerian, rose hips, mint) that eliminate nausea and vomiting. Among medications, prokinetics are often used to improve gastrointestinal motility, antispasmodics, and choleretics. You should avoid taking strong antiemetic drugs without a doctor's prescription, as this can be dangerous to your health.