Prevalence
In the International Classification, the disease is recorded under code K29.6 in the group “Other gastritis”. Since separate records of the disease are not kept, we can rely on data on postoperative complications and studies on attendance at clinics.
It has been shown that duodenogastric reflux occurs in 52.6% of cases as a consequence of operations on the duodenum, and in connection with removal of the gallbladder - in 15.5%. Symptoms similar to biliary reflux gastritis are detected in 25–40% of adults.
Surgical treatment of GHD
If conservative correction is ineffective, surgical intervention is indicated; the purpose of the operation is to strengthen the pyloric valve, as well as reduce the volume of bile thrown into the stomach. The operation is carried out in several directions:
- elimination of the causes that led to duodeno-gastric reflux;
- pyloroplication – performed to reduce symptoms of pyloric dehiscence;
- in the presence of hiatal hernia and calculous cholecystitis, fundoplication with crurorrhaphy and cholecystectomy is indicated.
In our clinic, laparoscopic access is used for surgical treatment of patients with GHD - all surgeon actions are performed through 3-4 punctures on the abdominal wall, and the length of the incision does not exceed 10 mm. Moreover, the operation itself is low-traumatic and painless; during its implementation, the likelihood of complications and blood loss are excluded. As a rule, the patient can go home within 2-3 days; work capacity is restored 2-3 weeks after surgery.
Causes and provoking factors
To understand why bile enters the stomach, which should be no higher than the duodenum, is necessary to determine the causes of the pathology. The greatest importance is attached to functional disorders of motility (peristalsis) of the stomach, its muscle tone, especially the sphincters. They manifest themselves as accelerated content release or delay. Accordingly, a distinction is made between hyper- and hypokinesia, hyper- and hypotension.
The most common is spastic contraction of the pylorus. In addition to inflammatory diseases of the stomach and duodenum, it is observed in neuroses, mental stress, in people with hysteria, and occupational intoxication. In case of decompensation, the stomach cavity expands. In differential diagnosis it is difficult to distinguish from cicatricial pyloric stenosis.
Hypotension and gastric hypokinesia accompany habitual overeating, drinking too much, and eating fatty foods. Similar disorders are observed with gastritis, enteritis, colitis, cholecystitis, and accompany many serious diseases of other organs, the nervous system (toxic paralysis), and postoperative complications.
Weakened peristalsis and gastric tone (paresis) lead to a gaping of the pylorus, through which contents can be thrown back from the duodenum
Dyskinesia is a group of disorders in the coordination of contraction of the gastric sphincters. They cause reflux of gastric contents into the esophagus, which provokes reflux esophagitis, and from the duodenum into the stomach. In the first case, gastroesophageal reflux disease of the esophagus develops. In this case, the main damaging substance is gastric acid.
Duodenogastric reflux is typical for hiatal hernia, peptic ulcer, duodenitis, pancreatitis, cholecystitis and inflammation of the biliary tract. Here the stomach suffers due to the action of irritating components of bile.
In a healthy person, contents from the underlying sections cannot reach higher levels due to the work of special stomach muscles (sphincters) located at the borders of the organ. They compress sufficiently after the passage of food and do not allow backflow.
Biliary or bile reflux gastritis is caused by the combined influence of several factors:
- impaired contractile function of the pylorus;
- decreased sphincter tone at the border of the stomach and duodenum;
- impaired motility of the digestive organs;
- chronic stagnation of duodenal secretions;
- consequences of surgical intervention on the digestive organs (gastric resection, pyloroplasty, gastroenterostomy, cholecystectomy);
- irritable bowel syndrome;
- prolapse of the stomach (gastroptosis);
- chronic hepatitis;
- peptic ulcers;
- taking non-hormonal anti-inflammatory drugs, antibiotics, painkillers, drugs containing iron and potassium, the action of the drugs causes blocking of the synthesis of prostaglandins, then mucus in the stomach;
- alcohol abuse;
- systemic disorders of nervous and endocrine regulation.
Some medical scientists disagree with the leading role of duodenogastric reflux in the development of biliary inflammation of the stomach. Their position is based on the fact that the gastric epithelium is considered quite resistant to the action of bile. They attribute the process to a physiological protective reaction that allows one to regulate acidity with alkaline contents in response to increased synthesis of hydrochloric acid.
Smoking is one of the provoking factors of pathology
The following factors can complement the listed factors: food excesses, wearing tight clothes, smoking, stressful situations. Biliary reflux occurs temporarily during pregnancy.
Approaches to the diagnosis and treatment of gastritis associated with bile reflux
The wide distribution of reflux gastritis in clinical practice in the absence of a single term [2] (synonyms: gastritis type C, alkaline gastritis, reactive gastropathy), as well as an understanding of the mechanisms of formation, standards of diagnosis and therapy make it relevant to analyze and highlight the existing ideas about this variant of gastritis .
Gastritis associated with biliary reflux (Latin refluo - to flow backwards) is rarely primary in nature [2, 3], mainly developing secondary to anatomical changes associated with surgery: gastric resection, gastroenterostomy, enterostomy, vagotomy, cholecystectomy. Failure of the sphincter apparatus, antroduodenal discoordination (impaired coordination between the antral, pyloric parts of the stomach and the duodenum), as well as resection of part of the stomach, leading to the elimination of the natural anti-reflux barrier, are the cause of the formation of recurrent reflux of duodenal contents containing bile into the stomach with damage to it mucous membrane.
Any diagnostic process begins with a survey and medical history. In the presence of symptoms of dyspepsia, which are not specific in nature and in some cases of reflux gastritis may be absent, as well as in diseases and conditions that have a high risk of biliary reflux (cholelithiasis, conditions after gastric resection, vagotomy, etc.), It is necessary to conduct an endoscopic examination with a biopsy of the gastric mucosa to determine the presence, degree and stage of gastritis, as well as Helicobacter pylori (HP) infection.
The endoscopic picture of reflux gastritis is characterized by hyperemia and swelling of the mucous membrane, which spread circularly from the pylorus in the proximal direction. At the same time, bile stains are often found on it, there is a visible reflux of bile from the duodenum into the stomach or a high content of bile in the lumen of the stomach.
There is no “gold standard” for diagnosing duodenogastric reflux yet. As a method of functional diagnostics, 24-hour pH-metry, fluoroscopy and ultrasound examination of the stomach are used. The main method for diagnosing biliary reflux is currently the pH-monitoring system Bilitec 2000, which quite qualitatively assesses bile reflux and pH in the stomach. Barrett MW et al [4] showed the high sensitivity of this device for monitoring bile reflux in vivo, but somewhat lower in vitro, with a false-negative rate of about 23%. In acidic conditions, the amount of bilirubin absorption determined by this device decreases, which can lead to an increase in false negative results and, accordingly, a decrease in false positive results. Although this method cannot be classified as the “gold standard” for duodenogastric reflux, it is the most convenient and usable for dynamic monitoring of bile reflux [5].
Why is reflux of duodenal contents into the stomach dangerous, what structural changes occur in the gastric mucosa under the influence of duodenal refluxate?
It is known that bile acids, which have detergent properties, promote the solubilization of lipids in the membranes of the surface epithelium, while their negative effect on the epithelium depends on their concentration, conjugation and pH of the environment, as well as on the length of time during which the mucous membrane is exposed to bile [6]. At low pH values, only taurine conjugates damage the mucous membrane, and at high pH values (for example, in the gastric stump after surgery), it is unconjugated bile acids that have a negative effect. In addition to the bile acids themselves, lysolecithin, formed under the influence of pancreatic phospholipase A from lecithin, has a damaging effect, with an increase in the reverse diffusion of hydrogen ions, as well as an increase in the release of histamine and gastrin. In recent years, the possible interaction of bile acids with a certain subtype of muscarinic receptors localized on chief cells has been discussed, as a result of which active inflammation, gland atrophy, intestinal metaplasia and focal hyperplasia develop in the gastric mucosa [7].
In addition, bile reflux, changing the chemical composition of the surface of the mucous membrane, can potentiate the action of other pathogenic factors: infections of HP and gastric juice [8, 9]. Chen SL et al [10], assessing the effect of biliary reflux on the severity of damage to the gastric mucosa in 49 patients with dyspepsia and chronic gastritis, did not establish a relationship between the duration of duodenal reflux and pH in the gastric cavity, which indicates the presence of complex feedback mechanisms, including regulation of the secretory and evacuation functions of the stomach. At the same time, the degree of changes in the mucous membrane, as well as colonization with HP infection, correlated with the duration of biliary reflux. Moreover, the data obtained clearly demonstrated the relationship between biliary reflux and the severity of damage to the gastric mucosa. Thus, severe reflux correlated with active inflammation (r = 0.3949, P < 0.05), chronic inflammation (r = 0.8938, P = 0.0001), mucosal atrophy (r = 0.4619, P < 0.005 ) and HP colonization in the body of the stomach (r = 0.8938, P = 0.0001). In this work, as in some others [11], the cumulative pathogenic effect of HP infection and biliary reflux on the gastric mucosa was demonstrated. One can assume a complex mechanism for this effect. Thus, the absorption of bile refluxant on the surface of the gastric mucosa has a direct damaging effect, and also enhances the effect of pepsin and hydrochloric acid; damage to the mucous membrane, in turn, contributes to the colonization of HP from the antrum to the body of the stomach. In the absence of infection of HP due to the reflux of alkaline contents from the duodenum and changes in pH, bacterial contamination by the microflora of the underlying parts of the digestive tract is possible, which also leads to more pronounced damage to the gastric mucosa.
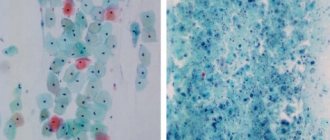
The characteristic morphological signs of this variant of gastric damage include the phenomenon of foveal hyperplasia, proliferation of smooth muscle cells in the lamina propria, as well as changes in the production of mucins by mucocytes, which play an important role in the protection of the mucous membrane [12] (Fig.). Modification of secreted mucins, detected immunohistochemically, leads to reactive/regenerative changes similar to the manifestations of gastropathy caused by nonsteroidal anti-inflammatory drugs (NSAID gastropathy) [13]: the expression of membrane mucin (MUC1), which is involved in the processes of adhesion and polarity, and secretory mucins (MUC5AC and MUC6). The detected changes differ from HP-associated gastritis, in which the expression of MUC5AC on the surface epithelium decreases, and the MUC6 mucin spreads to the surface of mucocytes [14].
In prognostic terms, another aspect of changes in the gastric mucosa associated with biliary reflux is also extremely important. Persistence of inflammation with hyperproduction of free radicals, impaired microcirculation and, as a consequence, impaired cellular renewal processes leads to a more frequent occurrence of atrophy and intestinal metaplasia of the gastric mucosa compared to a similar age population. It is appropriate here to recall the higher risk of developing intestinal cancer in the gastric stump, which has been demonstrated in both experimental and epidemiological studies [15, 16].
Of course, the presence and severity of the inflammatory infiltrate, as well as atrophy of the gastric mucosa, do not determine whether the patient has clinical symptoms of dyspepsia resulting from disorders of gastric secretion, gastroduodenal motility, and visceral sensitivity. Why, then, is it so important for a clinician to adequately interpret the pathologist’s findings? The answer lies in the goals of the gastritis classification system - to assess the condition of the mucous membrane, characterize the inflammatory process for prognosis and personalize the patient’s observation program, primarily to prevent the progression of inflammatory changes and the development of atrophy, intestinal metaplasia, dys/neoplasia.
A thorough analysis of the dyspepsia syndrome, data from endoscopic, biopsy and functional studies, carried out by the clinician, creates the basis for the formation of treatment goals for the patient:
- relieve manifestations of dyspepsia (if any) to improve the patient’s quality of life;
- reduce changes in the mucous membrane to prevent the formation of atrophy with intestinal metaplasia, and if they are present, stop the progression of changes in the mucous membrane to prevent stomach cancer.
An important component of the treatment program should be the modification of the patient’s lifestyle and diet. Timely intake of food, the absence of excess animal fats and sweet carbonated drinks in the diet, cessation of smoking and alcohol intake contribute to positive changes in the course of gastritis with dyspepsia syndrome.
If HP infection is present, eradication therapy should be planned to eliminate an additional factor that damages the gastric mucosa and increases the risk of recurrence of dyspepsia syndrome.
Since motor disorders occupy a key position in the formation of reflux gastritis, it is advisable to prescribe prokinetics (Ganaton, Trimedat) as one of the means of pathogenetic therapy. However, only by prescribing drugs of this group it is impossible to achieve all the goals of therapy for reflux gastritis.
The next group of pathogenetic therapy agents, rational for a number of patients with cholelithiasis, functional disorders of the biliary tract, and concomitant chronic diffuse liver diseases, are ursodeoxycholic acid preparations (Ursosan, Ursofalk, Urdoxa, Ursodex), which are prescribed in a daily dose of 10–13 mcg /kg of weight in courses of 6-8 weeks, and if necessary - for a longer period.
The classic conservative approach to the treatment of gastritis associated with biliary reflux is the administration of antacids and bismuth salts. In one well-designed study, the use of sucralfate and rabeprazole in patients with biliary reflux after cholecystectomy demonstrated its effectiveness on both clinical manifestations and the severity of macroscopic signs of inflammation diagnosed by endoscopic examination [17].
Thus, the appointment of a course of therapy with prokinetics, antisecretory agents and mucocytoprotectors makes it possible to relieve the symptoms of dyspepsia. It is also possible to reduce changes in the mucous membrane in order to prevent the development of atrophy with intestinal metaplasia, and if they are present, to stop the progression of changes in the mucous membrane for the prevention of stomach cancer as a result of including muco/cytoprotectors in therapy.
The group of muco/cytoprotectors includes several drugs (table), among which the therapeutic capabilities of bismuth salts, including De-Nol, should be separately highlighted. Numerous studies have shown that bismuth preparations form a protective layer on the affected areas of the mucous membrane, protecting it from the effects of aggressive factors, stimulate the secretion of mucus and bicarbonate, inhibit the activity of pepsin, protect epithelial growth factors from decay, promoting the regeneration of epithelial cells, improve microcirculation, stimulate secretion of gastroprotective prostaglandins. Along with the cytoprotective effects listed above, two factors should be mentioned separately. This is the bactericidal effect of De-Nol against Helicobacter and the ability of De-Nol to bind bile acids [26]. Helicobacter eradication using a four-component regimen, including De-Nol, significantly reduces the severity of duodenogastric reflux, which was convincingly shown in a study by SD Ladas et al. [27]. Neutralization of bile acids and their salts is also extremely important in terms of eliminating one of the leading pathogenetic factors of reflux gastritis. Considering the above, the use of De-Nol for gastritis caused by duodenogastric reflux is absolutely justified from a pathogenetic point of view.
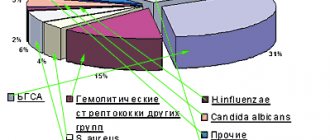
Under conditions of contamination of the gastric mucosa with non-NR microorganisms [18], including Helicobacter spp. [19], Proteus mirabilis, Citrobacter freundii, Klebsiella pneumoniae, Enterobacter cloacae, Staphylococcus aureus, with an additional stimulus for the persistence of the inflammatory infiltrate, activation of lipid peroxidation processes and the production of nitrosamines by bacteria, which have pro-carcinogenic potential [20], it is also important for the clinician to use the effects of salts bismuth. Firstly, not being an antibiotic, De-Nol suppresses the activity of bacterial flora without the risk of developing resistance, which has been successfully used for many years in standard eradication therapy. Secondly, in conditions of persistent inflammation, the properties of De-Nol that affect the activity of the inflammatory process become necessary, namely a decrease in the content of pro-inflammatory cytokines and the presence of an antioxidant effect. It should be noted that these properties of the drug are successfully used in the treatment of other diseases, including intestines. Thirdly, patients with reflux gastritis, especially with atrophy, especially need mucocytoprotective therapy with increased production of mucus, prostaglandins, and improved microcirculation in the gastric mucosa [25].
Finally, attempts are being made to correct the negative impact of reflux using surgical methods [21] (entero-enteroanastomosis according to Brown, Roux-en-Y), especially after gastrectomy as a “reserve” if all other methods of therapy have been ineffective.
Thus, gastritis associated with bile reflux, despite the lack of diagnostic and treatment standards, can be detected in a timely manner using an integrated approach and there are quite reliable, safe and effective drugs for its treatment.
Literature
- Kawiorski W., Herman RM, Legutko J. Current diagnosis of gastroduodenal reflux and biliary gastritis // Przegl Lek. 2001; 58:90–94.
- Hermans D., Sokal EM, Collard JM, Romagnoli R., Buts JP Primary duodenogastric reflux in children and adolescents // Eur J Pediatr. 2003, Sep; 162(9):598–602. Epub 2003, Jun 26.
- Lin JK, Hu PJ, Li CJ, Zeng ZR, Zhang XG A study of diagnosis of primary biliary reflux gastritis // Zhonghua Neike Zazhi. 2003; 42:81–83.
- Barrett MW, Myers JC, Watson DI, Jamieson GG Detection of bile reflux: in vivo validation of the Bilitec fibreoptic system // Dis Esophagus. 2000; 13:44–45.
- Barrett MW, Myers JC, Watson DI, Jamieson GG Dietary interference with the use of Bilitec to assess bile reflux // Dis Esophagus. 1999; 12:60–64.
- Stathopoulos P., Zundt B., Spelsberg FW, Kolligs L., Diebold J., Goke B., Jungst D. Relation of gallbladder function and Helicobacter pylori infection to gastric mucosa inflammation in patients with symptomatic cholecystolithiasis // Digestion. 2006; 73 (2–3): 69–74.
- Raufman JP, Cheng K., Zimniak P. Activation of muscarinic receptor signaling by bile acids: physiological and medical implications // Dig Dis Sci. 2003; 48:1431–1444.
- Chen SL, Mo JZ, Chen XY, Xiao SD The influence of bile reflux, gastric acid and Helicobacter pylori infection on gastric mucosal injury: Severity and localization // Weichang Bingxue. 2002; 7: 280–285x.
- Johannesson KA, Hammar E., Stael von Holstein C. Mucosal changes in the gastric remnant: long-term effects of bile reflux diversion and Helicobacter pylori infection // Eur. J Gastroenterol Hepatol. 2003; 15:35–40.
- Chen SL, Mo JZ, Cao ZJ, Chen XY, Xiao SD Effects of bile reflux on gastric mucosal lesions in patients with dyspepsia or chronic gastritis // World J Gastroenterol. 2005. May 14; 11(18):2834–2847.
- Abe H., Murakami K., Satoh S., Sato R., Kodama M., Arita T., Fujioka T. Influence of bile reflux and Helicobacter pylori infection on gastritis in the remnant gastric mucosa after distal gastrectomy // J Gastroenterol. 2005, Jun; 40(6):563–569.
- Mino-Kenudson M., Tomita S., Lauwers GY Mucin expression in reactive gastropathy: an immunohistochemical analysis // Arch Pathol Lab Med. 2007, Jan; 131(1):86–90.
- Mino-Kenudson M., Tomita S., Lauwers GY Mucin expression in reactive gastropathy: an immunohistochemical analysis // Arch Pathol Lab Med. 2007, Jan; 131(1):86–90.
- Corfield AP, Myerscough N., Longman R., Sylvester P., Arul S., Pignatelli M. Mucins and mucosal protection in the gastrointestinal tract: new prospects for mucins in the pathology of gastrointestinal disease // Gut. 2000. 47: 589–594.
- Ma Z., Wang Z., Zhang J. Carcinogenicity of duodenogastric reflux juice in patients undergoing gastrectomy // Zhonghua Wai Ke Za Zhi. 2001, Oct; 39(10):764–766.
- Oba M., Miwa K., Fujimura T., Harada S., Sasaki S., Hattori T. Chemoprevention of glandular stomach carcinogenesis through duodenogastric reflux in rats by a COX-2 inhibitor // Int J Cancer. 2008, Oct 1; 123(7):1491–1498.
- Santarelli L., Gabrielli M., Candelli M., Cremonini F., Nista EC, Cammarota G., Gasbarrini G., Gasbarrini A. Post-cholecystectomy alkaline reactive gastritis: a randomized trial comparing sucralfate versus rabeprazole or no treatment // Eur J Gastroenterol Hepatol. 2003, Sep; 15(9):975–979.
- Takako Osaki, Katsuhiro Mabe, Tomoko Hanawa, Shigeru Kamiya. Urease-positive bacteria in the stomach induce a false-positive reaction in a urea breath test for diagnosis of Helicobacter pylori infection // Journal of Medical Microbiology. 2008, 57, 814–819.
- Cinthia G. Goldman and Hazel M. Mitchell. Helicobacter spp. other than Helicobacter pylori 2010 Blackwell Publishing Ltd, Helicobacter 15(Suppl. 1): 69–75.
- Correa P. A human model of gastric carcinogenesis // Cancer Res. 1988; 48:3554–3560.
- Madura JA Primary bile reflux gastritis: diagnosis and surgical treatment // Am J Surg. 2003, Sep; 186(3):269–273.
- Slomiany V. L., Nishikawa H., BHski J., Slomiany A. Colloidal bismuth subcitrate inhibits peptic degradation of gastric mucosa_epidermal grown factor in vitro // Amer. J. Gastroenterol. 1990. V. 85. P. 390–393.
- Lambert JR, McLean. Pharmacology of colloidal bismuth subcitrate (De-Nol) and use in non ulcer dyspepsia / Helicobacter pylori in peptic ulceration and gastritis; eds. B. J. Marshall, R. W. McCallum, R. L. Guerrant. Oxford, London, Edinburgh, Melbourne: Blackwell Scientific Publications, 1991, pp. 201–209.
- Kononov A.V. Cytoprotection of the gastric mucosa: molecular cellular mechanisms // Russian Journal of Gastroenterology, Hepatology and Coloproctology. 2006. No. 3. pp. 12–16.
- O'Connor A., Gisbert JP, McNamara, O'Morain C. Treatment Of Helicobacter pylori Infection 2011 // Helicobacter. 2011. Sep. 16:53–58.
- Wagstaff AJ, Benfield P, Monk JP Colloidal bismuth subcitrate. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic use in peptic ulcer disease // Drugs. 1988; 36: 132–157.ha
- Ladas SD, Katsogridakis J., Malamou H. et al. Helicobacter pylori may induce bile reflux: link between H. pylori and bile induced injury to gastric epithelium // Gut. 1996; 38: 15–18.
M. F. Osipenko*, Doctor of Medical Sciences, Professor M. A. Livzan**, Doctor of Medical Sciences
* State Educational Institution of Higher Professional Education "Novosibirsk State Medical University of the Ministry of Health and Social Development of Russia", Novosibirsk ** State Educational Institution of Higher Professional Education "Omsk State Medical Academy of the Ministry of Health and Social Development of Russia", Omsk
Contact information for authors for correspondence
How does the surface of the stomach change?
Morphological changes often occur years later. In the section closest to the intestine—the antrum—epithelial cells grow rapidly, and the mucous goblet glands disappear.
The surface becomes swollen, and an accumulation of basophilic leukocytes saturated with nucleic acids is observed. They cause mild inflammation. A long process leads to cell degeneration and then to necrobiosis. Erosion forms and the production of protective mucus stops.
First, a focal process develops. It is possible that areas of mixed inflammation may coexist, alternating with normal mucosa. Subsequently, areas of atrophy grow. If left untreated, the epithelium may transform into malignant with the development of a tumor.
Diagnosis and treatment
To diagnose this disease, you will need to consult a competent specialist. Even during the examination, the doctor pays attention to pain in the abdomen, carefully examines the patient’s skin and listens to all complaints that worry the patient. Then the patient is prescribed a series of examinations that can more accurately determine the form of the disease and the degree of damage to the stomach:
- X-ray of the stomach with contrast;
- measuring the concentration of gastric juice in the esophagus throughout the day;
- research of its composition;
- general blood analysis;
- stool analysis for the presence of blood impurities;
- breath test for the presence of the bacterium Helicobacter pylori (Helicobacter pylori);
- sampling material for biopsy.
After the diagnosis is confirmed, the doctor prescribes drug therapy. In this case, medications help normalize the functioning of the gastrointestinal tract and bind bile acids. Treatment is mainly with proton pump inhibitors and prokinetics. Also, in order to neutralize bile acids, which have a detrimental effect on the gastric mucosa, ursodeoxycholic acid is used. To eliminate other unpleasant symptoms, painkillers and drugs that reduce bile secretion are used.
Kinds
Based on the nature of the lesion and the localization of inflammation in the stomach, the following forms of biliary reflux gastritis are distinguished:
- superficial - epithelial dystrophy is typical;
- catarrhal - swelling and inflammation of the inner membrane are associated;
- erosive - deep layers are affected, necrobiosis of cells forms erosions, and symptoms such as bleeding appear;
- antral - indicates the development of gastritis in the lower part of the organ (pyloric canal, antrum, pyloric sphincter), this zone is the first to be affected and suffers the most.
Since there is no single classification, some authors highlight:
- acute biliary reflux gastritis;
- fibrinous with the release of fibrinous-purulent exudate;
- necrotic;
- purulent.
Recommendations for diet and regimen
Regardless of the stage and severity of GERD, treatment involves constant adherence to certain rules:
- Do not lie down or lean forward after eating.
- Do not wear tight clothes, corsets, tight belts, bandages - this leads to an increase in intra-abdominal pressure.
- Sleep on a bed in which the part where the head is located is raised.
- Do not eat at night, avoid large meals, do not eat too hot food.
- Quit alcohol and smoking.
- Limit consumption of fats, chocolate, coffee and citrus fruits, as they are irritating and reduce LES pressure.
- Lose weight if you are obese.
- Stop taking medications that cause reflux. These include antispasmodics, β-blockers, prostaglandins, anticholinergic drugs, tranquilizers, nitrates, sedatives, calcium channel inhibitors.
Symptoms
The disease develops gradually and has a chronic course. The most common symptoms:
Signs of atrophic gastritis of the stomach
- pain in the epigastric region on an empty stomach, of varying nature and intensity (acute or constant aching);
- feeling of heaviness in the upper abdomen;
- bloating (flatulence);
- belching of eaten food and air;
- heartburn;
- nausea;
- periodic vomiting of bile;
- unstable stool (alternating diarrhea and constipation);
- decreased appetite;
- weight loss
Digestive disorders cause anemia and hypovitaminosis. They are manifested by increased fatigue, dizziness, dry skin, cracks in the corners of the lips.
The bitter taste in the mouth increases the nervousness of patients
Chronic reflux gastritis is characterized by a wave-like course. There are asymptomatic cases that are detected by fibrogastroscopy. The severity of the symptom is always parallel to the degree of damage to the mucous membrane.
Doctor's comment
If you are worried about heartburn and nausea, and your usual medications and strict adherence to a diet do not bring relief, if you often experience abdominal pain that gets worse after eating, perhaps the cause of this condition is duodenogastric reflux. You can determine its presence in our clinic, where for a high-quality examination you can undergo all the necessary diagnostic procedures - at any time convenient for you. Treatment tactics depend on the degree of the disease. This may be drug therapy or surgical treatment, which is indicated when conservative methods are ineffective. Our patients have the option of treatment in a day hospital. The operation in the clinic is carried out using laparoscopy: all actions are carried out through 3-4 punctures on the abdomen, which subsequently become invisible. During the operation, which is painless and bloodless, the likelihood of complications is virtually eliminated. After 1-3 days, our patients are discharged from the clinic; in the future, there is no need to take medications or strictly follow a diet. Therefore, do not delay treatment, because with advanced duodeno-gastric reflux, treatment will be more difficult and longer.
Head of the surgical service at SwissClinic Konstantin Viktorovich Puchkov
Diagnostics
The doctor becomes suspicious of the disease after careful questioning and clarification of the patient’s complaints, when the cause is identified. Special attitude towards persons who have undergone surgery. They are additionally examined by a surgeon. Indirect confirmation of digestive disorders is possible through blood and stool tests (scatology + occult blood).
The basis of diagnostics is hardware research. Fibrogastroduodenoscopy reveals foci of inflammation in the antrum, swelling of the epithelium, and widening of the sphincter opening between the duodenum and the pyloric part of the stomach.
Modern interpretation of gastritis requires assessment of the condition of the mucosa using a biopsy taken during fibrogastroduodenoscopy. In this way, the form of the disease is confirmed and the presence of epithelial metaplasia during the transition to cancer is checked.
To study the motility and contractility of the gastroduodenal zone, antroduodenal manometry or gastrography is used.
If necessary, daily pH measurements are carried out using the Gastroscan apparatus.
Acidity measurements using pH measurements and the use of a histamine test make it possible to study the influence of the level of acid formation in the stomach. X-ray of the stomach and intestines using a barium suspension helps to trace the movement of stomach contents, record violations of the contraction of the pyloric sphincter and reflux in the images. To check the participation of other organs of the digestive tract in the pathogenesis, an ultrasound of the abdominal cavity is performed.
Conservative treatment of duodenogastric reflux
The goal of conservative therapy is to neutralize the aggressive effect of duodenal contents on the mucous membrane of the stomach and esophagus, improve the evacuation capacity of the stomach and antroduodenal coordination. For this purpose, drugs are prescribed that normalize the motility of the upper gastrointestinal tract, prokinetics, enhancing the peristalsis of the stomach and duodenum and improving the evacuation of their contents, antacids, etc.
In addition, since duodenogastric reflux is often combined with other diseases of the digestive system, drugs are also needed to treat the underlying pathology. In addition, great importance is given to following a diet and giving up bad habits. Conservative treatment is difficult, and although the clinical manifestations of reflux decrease with medication, this is only a temporary improvement. It is possible to achieve good results with conservative therapy only in case of functional disorders that cause reflux.
Treatment of biliary reflux gastritis
Therapy of the disease requires the patient to quit smoking, drinking alcohol, fatty, spicy and fried foods. Much more attention will have to be paid to proper nutrition and adherence to the regime. Intense exercise on the abdominals is not recommended. Muscle tension increases intraperitoneal pressure and promotes reflux movements.
To relieve the negative effects of acidity, drugs and folk remedies with an enveloping effect are used: Maalox, Almagel, decoction of flax seeds, oatmeal jelly. Almagel A also contains Anestezin, so it provides good pain relief to the inflammatory zone. For high acidity, drugs that block the secretion of gastric juice (Omeprazole, Rabeprazole) and histamine receptor blockers are indicated.
Hydrotalcite - contains combined minerals (magnesium, aluminum) that suppress acid secretion
A group of prokinetics is prescribed to improve the tone of the pyloric sphincter and the muscular layer of the stomach (Primer, Motilium, Motilak). Domperidone and Metoclopramide prevent reflux into the stomach. In order to bind bile acids and improve the outflow of bile, ursodeoxycholic acid preparations (Ursofalk, Ursosan, Ursachol, Holacid) are used.
In case of a long course of the disease, vitamins A, E, group B are certainly prescribed. If the examination excludes suspicion of an erosive form and oncology, then courses of physiotherapy are effectively used:
- amplipulse therapy is a method of restoring gastric motility and normalizing secretory function;
- exposure to decimeter waves and ultra-high frequency - relieves swelling of the mucous membrane, pain, stimulates healing.
Indications for acupuncture are considered individually.
Folk remedies
Traditional medicine recipes are popular among patients with moderate biliary reflux gastritis. The decoctions must be taken over a long period of time. Recommended:
- combined use of chamomile, St. John's wort and yarrow;
- dandelion and mint flower syrup.
Typically, chamomile, plantain, calendula, and dandelion are used for low acidity, but their anti-inflammatory properties are needed to treat gastritis. Therefore, use in combination and mixtures is permitted.
Surgical treatment
Surgical intervention for biliary gastritis is rarely used. Usually they operate on emergency indications (bleeding), or routinely when non-healing ulcers, erosions, and tumor formations are detected.
To prevent reflux gastritis, it is necessary to exclude factors that provoke the disease. Monitoring your health after surgery allows you to start preventive treatment earlier and identify complications. Therefore, patients should be examined at least once a year.
Treatment
Treatment should be comprehensive and include measures to normalize lifestyle, diet and diet, as well as drug therapy. If possible, eliminate physical and emotional stress that negatively affects the motility of the gastrointestinal tract. Long breaks in meals, consumption of fatty, extractive foods, marinades, smoked meats, and coffee are unacceptable. Avoid smoking, drinking alcohol and carbonated drinks. Drug therapy is selected by a gastroenterologist depending on the severity of symptoms and examination results.
Duodenogastric reflux, or the reflux of duodenal contents back into the stomach, is an extremely common digestive disorder. The symptoms that indicate this pathology are subjectively interpreted by many as “heartburn” or “indigestion,” which indicates their low specificity. An accurate diagnosis can only be made by a specialist after a thorough examination. If you experience discomfort associated with eating, we recommend that you contact Professor Gorbakov’s Clinic for specialized help.
Normally, food enters the oral cavity, moves down the esophagus into the stomach, and then enters the duodenum. Here it mixes with bile, which ensures the emulsification (breakdown) of fats and the absorption of most of the nutrients. The unilateral evacuation of food into the duodenum is supported by the reflexive opening and closing of the pyloric sphincter (pylorus). It also prevents retrograde (backward) flow of the bolus.
Improper functioning of the sphincter (its insufficient locking), as well as hypertension in the duodenum associated with chronic duodenitis, can cause bile to flow back into the stomach - duodenogastric reflux.
Often this disorder provokes the presence of inflammatory processes in the stomach (gastritis), duodenum (duodenitis), gallbladder (cholecystitis, biliary dyskinesia), pancreas (pancreatitis), and surgical interventions, namely:
- cholecystectomy;
- gastric resection;
- vagotomy;
- gastroenterostomy;
- enterostomy.
Therapy in older children
Correcting the child’s lifestyle is of great importance in the treatment of reflux disease.
- The end of the bed, where the head is located, should be raised by at least fifteen centimeters. This simple measure can reduce the duration of acidification of the esophagus.
- It is necessary to introduce dietary restrictions for the child: reduce the fat content in the diet and increase the protein content, reduce the amount of food consumed, exclude irritating foods (citrus juices, chocolate, tomatoes).
- It is necessary to develop the habit of not eating at night and not lying down after eating.
- It is necessary to ensure that the child does not wear tight clothes or sit bent over for a long time.
As a drug treatment, as in adults, antacid drugs are used, usually in the form of a suspension or gel (Almagel, Phosphalugel, Maalox, Gaviscon), prokinetic agents (Motilak, Motilium) , "Cerucal"). The choice of a specific medication and determination of the dosage is carried out by the attending physician.