Human African trypanosomiasis, also known as sleeping sickness, is a vector-borne parasitic disease. Its causative agents are parasitic protozoa belonging to the genus Trypanosoma. They are transmitted to humans by the bite of a tsetse fly (genus Glossina), infected from humans or animals that act as hosts of these parasites that are pathogenic to humans.
The tsetse fly is found only in sub-Saharan Africa, and only a few species can transmit the disease. For currently unknown reasons, cases of sleeping sickness are not reported in many areas of the tsetse fly's habitat. Residents of endemic rural areas engaged in agriculture, fishing, livestock raising and hunting are most susceptible to tsetse fly bites and, consequently, to this disease. Cases of the disease can occur both in individual villages and in the entire region. Within a single infected area, the intensity of the spread of the disease can vary greatly from one rural settlement to another.
General information
Trypanosomiasis is a tropical vector-borne disease caused by protozoan microorganisms of the flagellate class - trypanosomes .
There are African trypanosomiasis (synonyms - sleeping sickness, African sleeping sickness) and American trypanosomiasis (synonyms - Chagas disease, morbus Shagasy, colloquially incorrectly pronounced Chagas disease and Chagas syndrome). Each of these species has its own geographical distribution, which is determined by the habitat of the disease carriers. African sleeping sickness is the habitat of tsetse flies of the species Glossina palpalis (about 36 countries of tropical Africa - the Congo River bed, Gambia, Uganda, Nigeria, Rwanda, Burkina Faso, Cameroon, Gabon, Kenya, Mozambique, Zambia, Equatorial Guinea, Zimbabwe, Ghana and others), on the territory of which about 50-60 million people live who are at high risk of infection with trypanosomiasis. The habitat (“fly belt”) is about 4 million square meters. km.
American trypanosomiasis is found primarily in endemic areas of 23 Latin American countries, in the habitat of kissing (cone/triatomine) bugs, the names of which vary depending on the geographic area. Currently, according to WHO, Chagas disease kills about 10,000 people every year, about 7-8 million people are infected, and about 25 million people live in a high-risk group. At the same time, this disease has become increasingly common in recent years in the countries of the Western Pacific Ocean, the USA, Canada and even European countries, which is due to the ever-increasing migration processes in various directions. If treatment for Chagas disease is started immediately after infection, a complete recovery can be achieved. With advanced disease, 30% of infected individuals develop changes in the cardiac system, and 10% of individuals develop changes in the nervous/digestive system or a mixed nature that require special treatment.
Major epidemics
Several epidemics have occurred in Africa over the past century:
- the epidemic of 1896-1906, mainly affecting Uganda and the Congo River basin;
- the 1920 epidemic that affected a number of African countries; And
- the most recent epidemic, which began in 1970 and continued until the end of the 1990s.
In 1920, the epidemic was fought with mobile teams that screened millions of people living in high-risk areas. By the mid-1960s. the spread of the disease was brought under control, with fewer than 5,000 cases reported throughout the continent. Following this success, surveillance was relaxed, causing the disease to return, and by 1970, outbreaks had grown to epidemic levels in several regions. In the 1990s. and at the beginning of the 21st century, thanks to the efforts of WHO, the implementation of national programs to combat the disease, bilateral cooperation and the activities of non-governmental organizations (NGOs), the upward trend in incidence was stopped.
As the number of new cases of human African trypanosomiasis decreased significantly between 2000 and 2012 as a result of international coordinated efforts, the WHO Roadmap for Control of Neglected Tropical Diseases set a goal for its elimination as a public health problem by 2021 and elimination transmission (reducing the number of cases to zero) by 2030.
Pathogenesis
African sleeping sickness
Trypanosomes in their metacyclic forms enter the human body after the bite of an infected tsetse fly and begin to actively multiply in the subcutaneous tissue. chancre (local inflammatory focus) often forms at the site of the bite As they multiply over several days, trypanosomes penetrate the lymphatic/blood vessels, thereby promoting the dissemination of the pathogen and the generalization of the pathological process. This process is caused by predominant damage to the lymphatic system, central nervous system and heart ( pancarditis ). In the initial stages of the process an enlargement of the lymph nodes and spleen occurs; later, fibrous changes in the tissues of these organs, perivasculitis and endarteritis with pronounced proliferation of the endothelium of small blood vessels may develop.
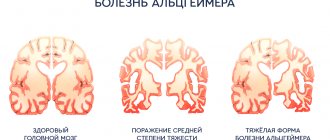
After trypanosomes penetrate into the cerebrospinal fluid and the brain, meningoencephalitis /meningomyelitis develops with pronounced neuroglial proliferation and perivascular infiltration in the pia mater of the spinal cord/brain with the development of edema, hemorrhage and thrombosis in the brain structures, with the formation of granulomas. With the further development of the pathological process, perivasculitis of cerebral vessels develops, proliferation of astrocytes and microglia develops with the development of obliteration of cerebral vessels with severe multiple hemorrhages .
A characteristic feature of sleeping sickness is alternating periods of exacerbation and remission, which is accompanied by fluctuations in the level of parasitemia, increased levels of serum IgM and changes in antigenic variants of trypanosomes. It has been proven that part of the multiplied subpopulation of trypanosomes is eliminated after entering the blood, which is due to the protective effect of the humoral/cellular mechanisms of human immunity.
The survival of the pathogen is achieved by changing the amino acid sequence of the glycoprotein , which covers the parasite's shell with a continuous layer. At the same time, antigenic variability in the structure of the glycoprotein molecule can occur repeatedly and in many variants. Accordingly, in the pathogenesis of trypanosomiasis, such immunopathological processes contribute to the formation of immune complexes circulating in the blood with deposition in the internal organs. In addition, trypanosomes in the human body have an immunosuppressive effect, which helps to weaken the body’s resistance and the development of secondary infectious complications in the later stages of the disease. In fact, pathogenesis can be reduced to mechanical destruction of cells/tissues of the affected organs and toxic-allergic effects on the human body.
American trypanosomiasis
After a bug bite, parasites penetrate into the histiocytes of the surrounding tissue, multiply there and spread through the blood throughout the body. trypomastigotes into amastigotes occurs , which intensively multiply and pseudocysts are formed, which are dead cells that are filled with amastigotes .
Further, the development of the infectious process can occur in different ways. In the acute stage, intensive reproduction and hematogenous dissemination of trypanosomes occurs. Pseudocysts surrounded by plasma cells and lymphocytes are found in the cells of a wide variety of tissues, but their localization predominates in the myocardium and intestinal smooth muscles. Subsequently, as the disease progresses, infiltration by immunocompetent cells increases, but the parasites remain alive throughout a person’s life. The pathogenesis of the acute stage is based on both the processes of destruction of tissue cells and toxic-allergic reactions.
Trypanosome cruzi is a parasite with pronounced immunogenic properties, and the evoked immune response is not only protective in nature, but also causes damage to human tissue (deposition of immune complexes), leading to changes in the walls of blood vessels. Also, already in the acute stage, along with damage to muscle cells, damage to the ganglia of the parasympathetic nervous system is observed.
When Chagas disease is chronic, the pathological process is limited to predominant damage to the tissues of the heart and intestines. It is based on pathological changes in the endocardium and changes in the conduction system. As a consequence of the inflammatory process, selective damage to the pathways is observed. In the myocardium, focal/diffuse infiltrates and multiple hemorrhages develop. myocarditis progresses, heart failure develops in most cases. Structural changes in the endocardium and the formation of aneurysms lead to the formation of parietal thrombi, which is the cause of thromboembolism in the systemic/pulmonary circulation.
In the pathogenesis of the chronic phases, degeneration of the autonomous intramural ganglia of intestinal smooth muscles is of significant importance, which causes dilation of the esophagus and large intestine and disruption of their function, and less commonly, the gallbladder/bladder and stomach. The vast majority of individuals who are infected with T. cruzi do not immediately develop clinical manifestations and this condition is considered as an intermediate stage between the acute stage/infection and the chronic one. And the chronic, clinically pronounced stage develops only after 10-20 years.
Treatment
The type of treatment depends on the form and stage of the disease. Early detection of the disease increases the chances of successful treatment. Because the parasite can remain viable for a long time and cause relapses many months after the end of therapy, patients should remain under observation for up to 24 months to evaluate the results of treatment, during which clinical examination of patients and laboratory tests should be performed. examination of bodily fluids, including, in some cases, cerebrospinal fluid obtained by lumbar puncture.
To successfully treat the disease at the second stage, it is necessary to use drugs that can overcome the blood-brain barrier and neutralize the parasite in the central nervous system.
In 2021, WHO published new treatment guidelines for the Gambian form of human African trypanosomiasis. A total of six drugs are registered for the treatment of sleeping sickness. These drugs are provided to WHO by manufacturers free of charge and supplied free of charge to endemic countries.
Drugs for the treatment of the disease at the first stage:
- Pentamidine: first developed in 1940, used to treat sleeping sickness caused by Tb gambiense in the first stage. Despite the presence of serious side effects, the drug is generally well tolerated.
- Suramin: first obtained in 1920, used to treat Tb rhodesiense disease in the first stage. The drug has a number of undesirable side effects, including nephrotoxicity and allergic reactions.
Drugs for the treatment of the disease in the second stage:
- Melarsoprol: first introduced in 1949, used to treat infections caused by both pathogens. It is an arsenic derivative and causes numerous unwanted side effects, the most severe of which is reactive encephalopathy (encephalopathic syndrome), which can be fatal (in 3%–10% of cases). It is currently recommended as a first-line treatment for the Rhodesian form of the disease, but is rarely prescribed for the Gambian form of infection.
- Eflornithine: registered in 1990, much less toxic than melasoprol, effective only against Tb gambiense. It is usually used in combination with nifurtimox (as part of combination nifurtimox-eflornithine therapy), although it can also be used as monotherapy. The treatment regimen is complex and inconvenient.
- Nifurtimox: Nifurtimox-eflornithine combination therapy was proposed in 2009. It simplifies the use of eflornithine by reducing the duration of treatment and the number of intravenous perfusions, but unfortunately its effectiveness against Tb rhodesiense has not yet been studied. Nifurtimox is registered for the treatment of American but not African human trypanosomiasis. WHO supplies both drugs to endemic countries free of charge, complete with all consumables necessary for their use.
Drugs to treat the disease at both stages:
Fexinidazole is an oral drug for the treatment of the Gambian form of human African trypanosomiasis. In 2021, the drug was included in the WHO Essential Medicines List and recommended in WHO guidelines for the treatment of human African trypanomosis. The drug is indicated as first-line therapy in the first and mild second stages of the disease. Treatment should be carried out under the supervision of qualified medical personnel; The drug is taken 30 minutes after eating solid food. Clinical trials of this drug are currently underway for the treatment of the Rhodesian form of trepanosomiasis.
Causes
African trypanosomiasis
Etiology. Sleeping sickness is caused by two subspecies of trypanosomes: Trypanosoma brucei gambiense, which causes the Gambian form, and Trypanosoma brucei rhodesiense, which causes the Rhodesian clinical and epidemiological form of the disease. Both types of parasites that cause African sleeping sickness are identical in morphological characteristics, however, as the invasion develops, the antigenic structure of the pathogen changes.
Morphological structure of trypanosome
Trypanosome is a unicellular microorganism of the class of flagellated protozoa with body dimensions of 15-40 x 1.4-2 microns, the morphological structure of which contains a membrane and cytoplasm in which the cell nucleus and mitochondria are immersed.
Morphologically, the pathogen may vary depending on its host: intermediate hosts have predominantly flagellated invasive forms, which provide them with the ability to actively move, and final hosts have flagellated forms.
Capable of existing exclusively as a parasitic life form. They can actively reproduce through longitudinal mitosis in the body of both an intermediate and permanent host. The life cycle of trypanosomes includes 2 stages: the epimastigote in the carrier’s body and the trypomastigote in the human body. The development process involves the change of two hosts - vertebrates and invertebrates.
Epidemiology
For Gambian trypanosome, the main host is humans. The carrier of sleeping sickness and intermediate host is the tsetse fly of the family Glossina (species G. Tachinoides), the main habitats of which are thickets along the banks of water bodies (rivers and lakes). Refers to anthroponoses (infections that are transmitted from person to person). The peak incidence occurs during the dry season of the year and can manifest as sporadic incidence or take on the character of epidemic outbreaks. It is found (map below) mainly in the countries of the Central/West African continent (Uganda, Nigeria, Zaire, Gambia, Cameroon, Angola), recorded mainly in residential areas located near water bodies.
Sick persons make up only 2-3% of all actually infected persons. The chronic course of the disease contributes to the long-term presence of infected individuals among the healthy population, which increases the risk of transmission of the pathogen by flies.
The main natural reservoir of the Rhodesian trypanosome is the forest antelope; cattle, various wild animals and humans act as additional reservoirs. The Rhodesian (synonymous with East African) form of African trypanosomiasis is a natural focal zoonotic invasion. The carrier is the tsetse fly of the species Glossinamorsitans and Glossinapallidipes. Infection of people occurs mainly during their stay in natural foci. It is found (map below) in the countries of Southern/Eastern Africa (Tanzania, Zimbabwe, Ethiopia, Botswana, Uganda, Kenya).
Mechanism of transmission of the pathogen, routes of infection
The main mechanism of transmission: obligate-transmissible, in which the pathogen is transmitted through a bite (inoculation) by a vector. The blood transfusion route of transmission (during the transfusion of infected blood, the use of non-sterile medical instruments) is much less common.
Trypanosomes in the form of trypomastigotes , when a fly absorbs the blood of an infected person, enter the stomach of the insect, where they multiply, turn into epimastigotes and migrate to the salivary glands. The development cycle of trypanosomes in the body of a fly takes from 15 to 35 days. The infection rate of the wild population of tsetse flies is 1-1.5%, and only in 10-12% of flies the pathogen completes its development cycle.
Tsetse fly
When a healthy person is bitten, the parasites are introduced into the body with the saliva of a fly, where trypanosomes first multiply in the subcutaneous tissue at the site of the bite, and then the pathogen enters the lymphatic vessels/blood and spreads throughout the body, penetrating the heart, liver, cerebrospinal fluid, brain, kidneys , spleen, bone marrow. The stages of development of trypanosomes in the body of flies and humans are shown schematically in the figure.
A sick person becomes infectious approximately 10-12 days after an insect bite and remains so throughout the entire period of illness.
Stages of trypanosome development in the tsetse fly/human body
American trypanosomiasis
Etiology. Chagas disease, named after its discoverer K. Chagas, is caused by trypanosoma cruzi, which is morphologically indistinguishable from the causative agents of African sleeping sickness. However, Trypanosoma cruzi has a different development cycle, including several successively changing morphological stages of the parasite: trypomastigote , epimastigote , promastigote and amastigote . In fact, T. cruzi undergoes two development cycles: one of them in the intestines of the triatomine bug, and the second in the body of vertebrates. The reproduction process of this species occurs only at the amastigote stage (cordless rounded formations) primarily at the site of penetration in the skin cells/under the mucous membranes, then in the macrophages of the lymph nodes adjacent to the bite site, and at later stages in the cells of the histiophagocytic system of the spleen and intestines , lymph nodes, skeletal muscles, heart muscle, neuroglia. Trypomastigotes are found in the blood of humans/animals and can be transmitted to bedbug vectors when they attack an infected/sick person.
Epidemiology. Shigas disease belongs to anthropozoonoses (a group of diseases with natural/synanthropic focality). The source of infection in natural foci are various kinds of wild animals: monkeys, armadillos, bats, marsupial rodents and others. Synanthropic foci include domestic animals (pigs, dogs, cats) and humans. The carrier of Chagas syndrome is various species of triatomine bugs, in particular, the families Reduviidae and Dimidiata (Wikipedia, Fig. 4.).
Triatomine bugs (a, b)
The causative agent of American trypanosomiasis is transmitted mainly through the bites/feces of bedbugs, which live both in bird nests/animal burrows and in human settlements, mainly in poorly maintained buildings made of straw and clay. Bedbugs attack people at night, and the bite sites are located mainly near the lips/eyes, hence their name “kissing bugs.”
The bite of an infected bug with damage to the skin and the subsequent frequent entry of bug excrement into the bite wound when scratching it ensures the penetration of a sufficient infectious dose (metacyclic form of trypanosome) for the development of the disease. Much less often, infection occurs directly from a sick person to a healthy person during blood transfusions in utero, during organ transplantation, with mother's milk or through the nutritional route, through food contaminated with bug feces.
Metacyclic forms of trypanosomes, which are an invasive stage for the human body, once in the macrophages of the skin/subcutaneous fat are transformed into leishmanial (amastigote forms), which multiply intensively. Then, after cell destruction, trypanosomes are first transformed into critidial (epimastigote), and then into trypanosome (trypomastigote) forms that circulate but do not multiply in the blood. Trypanosomes enter the bloodstream and infect the tissues of various organs, where the flagellated forms undergo intensive reproduction.
The development cycle of trypanosome Cruzi in the body of the bug and humans
Geographical distribution - the disease occurs primarily in the countries of south-central America (Mexico, Argentina, Brazil, Paraguay, Guatemala, Venezuela, Costa Rica, Uruguay, Honduras, Bolivia, and Panama).
Experienced trypanosomiasis does not leave behind lasting immunity. The main reason preventing the development of specific immunity is the antigenic variability of trypanosomes. The resulting antibodies, being specific to a certain antigenic variant of trypanosome, suppress its number, however, they do not act on the new variant.
Animal trypanosomiasis
Other species and subspecies of parasites of the genus Trypanosoma are pathogenic for animals and cause trypanosomiasis in some species of wild and domestic animals. Trypanosomiasis in cattle is called Nagana. Trypanosomiasis in domestic animals, especially cattle, seriously undermines the economic development of infected rural areas.
Animals can harbor parasites pathogenic to humans, especially Tb rhodesiense, with domestic and wild animals being important reservoirs for the latter. Animals can also be infected with Tb gambiense and may also act as reservoirs, although to a lesser extent. However, the actual role of the animal reservoir in the epidemiology of the Gambian form of the disease is still not well understood.
Symptoms
Sleeping sickness symptoms
The incubation period for Gambian sleeping sickness is 2-3 weeks, for Rhodesian sleeping sickness it is 1-2 weeks. Clinical manifestations of African sleeping sickness are characterized by a variety of symptoms and their nonspecificity, since in different endemic foci they vary significantly in the frequency of occurrence and severity of their manifestations.
Rhodesian trypanosomiasis is characterized by a more acute course with no clearly defined differences between the acute and chronic stages. Accompanied by fever , early damage to the central nervous system (3-4 weeks from the onset of the disease), severe heart damage, and fairly quickly occurring death (within several weeks).
Gambian trypanosomiasis is characterized by later damage to the central nervous system (2-4 months after infection), a long-term chronic progressive course, and severe damage to the lymph nodes.
Over the course of 7-15 days, trypanosomal chancroid can develop on the skin (at the site of the tsetse fly bite), mainly in non-indigenous Africans who are infected with Tb rhodesiense: a dark red papule, elastic, painful, with a diameter of 2 to 5 cm, which disappears spontaneously after 2-3 weeks.
Trypanosomal chancroid
There are 2 stages of the disease:
Early (hemolymphatic) stage
Manifested by fever , the duration of which varies from 2 to 7 days. Acute onset is more common with Tb rhodesiense infection in non-indigenous Africans. For people living in West Africa, the onset of the disease is usually gradual, and it may take several years before the first clinical symptoms appear. At an early stage, attacks of fever often alternate with periods of remission, lasting from 2-3 weeks to several months, during which patients feel satisfactorily. At this stage, neuropsychological changes appear - insomnia , headache, excitability, and less often drowsiness .
In some cases, an erythematous rash appears on the skin, having an oval shape with a diameter of 7-10 cm with a predominant localization in the area of the shoulders and hips, and the torso. Non-indigenous residents may experience hyperesthesia (Kerandell's symptom) - painful skin when squeezed. As the disease progresses, enlargement of the lymph nodes appears, mainly in the posterior cervical region/above the collarbone). At the same time, the lymph nodes are elastic, mobile, painless. In the early stage, skin itching, weight loss, weakness, swelling/pain in the joints of the extremities, tachycardia, hepatosplenomegaly, and periorbital edema may be noted.
Chronic (meningoencephalitic) stage
Clinical symptoms are caused by the development of diffuse meningoencephalitis with damage predominantly to the structures of the base of the brain. Characterized by an increase in neurological symptoms - disturbances in muscle tone, sleep, motor function, and reflexes of oral automatism. Neuropsychological changes appear imperceptibly and progressively increase, manifested by the development of depressive /manic states.
Initially, changes in personality and behavior are noted - fatigue, indifference and indifference to the environment, drowsiness during the day and insomnia . A number of individuals exhibit extrapyramidal disorders (tremor of the tongue/fingers, stiff neck, fibrillary muscle twitching). Speech is slurred, symptoms of cerebellar ataxia , leading to gait disturbances. With cerebral edema - swelling of the optic nerve head, severe headache. As the disease progresses, euphoria, epileptiform convulsions, a manic state, and severe drowsiness . When the hypothalamic-pituitary zone is involved in the pathological process, the feeling of hunger, thirst, libido is disrupted, and endocrine disorders appear ( impotence , amenorrhea , obesity ).
In the terminal stage, patients lie motionless in bed and refuse food. The most common causes of death are the development of cerebral coma , cachexia , and the addition of a secondary infection ( pneumonia , malaria , dysentery ). In African trypanosomiasis, the symptoms of sleeping sickness are accompanied by hemolytic anemia, thrombocytopenia, and also a bleeding disorder.
Rhodesian sleeping sickness has a more transient and severe course. Intoxication/fever is more pronounced, exhaustion occurs faster, and heart damage is more common. Death can occur even before the disease transitions to the meningoencephalitic stage, already in the first year of the disease.
American trypanosomiasis
There are several forms of clinical course.
Acute form - recorded in endemic foci mainly in children under 10 years of age. The duration of the acute stage varies between 1-1.5 months, while the symptoms of the acute stage may be mild and even go unnoticed. The incubation period for the acute clinically manifest form lasts 10-12 days. The onset is acute with chills and increased body temperature. Characterized by eye pain, anorexia, malaise, headache and muscle pain, and dyspeptic disorders.
At the site of introduction of trypanosome Cruzi through the skin, in most cases, a primary affect develops - shamoma (local inflammatory reaction), which is a red-violet infiltration on the skin, reminiscent of a moderately painful boil . Shagoma is often accompanied by regional lymphangitis / lymphadenitis . When infected through the conjunctiva of the eyes, the primary affect is represented by severe periorbital edema, conjunctivitis on the affected side with scanty discharge, and enlarged regional lymph nodes (Romagna symptom complex).
The disease is accompanied by a remitting fever, with temperature rises in the evening to 39-40°C, but with a benign course the febrile reaction is insignificant. In patients in the acute period of the disease, the lymph nodes of almost all groups are enlarged - axillary, cervical, inguinal, and hepatosplenomegaly . Changes in the heart are expressed - the boundaries are expanded to the left, systolic murmur, tachycardia , dullness of tones.
In severe cases, heart failure progresses rapidly and is one of the main causes of death. Also, the severe course of the disease is often complicated by meningoencephalitis , which occurs with a pronounced clinical picture of neurological disorders.
Indeterminate form - there are no clinically significant signs of the disease, except for the presence of positive serological reactions. The duration of this phase of the infectious process can last for many years, and in approximately 2/3 of infected individuals, until the end of life. In the remaining 1/3 of people, after 10-20 years, clinical symptoms of a chronic form of trypanosomiasis develop, caused by damage to the heart, gastrointestinal tract, and peripheral nervous system.
Chronic form - the leading symptom is myocardiopathy , dilatation of the ventricles of the heart and cardiomegaly are noted. As the disease progresses, circulatory failure, cardiac arrhythmias, and thromboembolism , particularly in the pulmonary arteries. Dysfunction of the endocrine, central/autonomic nervous system is also characteristic.
The ECG shows conduction and excitability disturbances (blockades and extrasystoles). Along with myocardiopathy, important clinical syndromes include “megacolon”, which is dilatation (expansion) of internal organs, mainly the esophagus and segments of the large intestine (sigmoid colon), which leads to constipation , difficulty swallowing and the development of intestinal obstruction . With sharp progression of the disease, cachexia .
Current distribution of the disease
Prevalence rates of the disease vary between countries, as well as between areas within a given country.
- Over the past 10 years, more than 70% of cases have been reported in the Democratic Republic of the Congo.
- Angola, Cameroon, Central African Republic, Chad, Congo, Guinea, Malawi, South Sudan and Zambia reported between 10 and 100 new cases in 2021, while Côte d'Ivoire, Equatorial Guinea, Gabon, Uganda, United The Republic of Tanzania and Zimbabwe – from 1 to 10 new cases.
- Over the past 10 years, isolated cases have been reported in countries such as Burkina Faso, Ghana and Nigeria.
- Benin, Botswana, Burundi, Ethiopia, Gambia, Guinea-Bissau, Liberia, Mali, Mozambique, Namibia, Niger, Rwanda, Senegal, Sierra Leone, Eswatini and Toga have reported no new cases in the past 10 years. In some of these countries, transmission appears to have stopped, but it is difficult to accurately assess the real situation in some areas because surveillance and diagnosis are hampered by social instability and/or difficulties in accessing the population.
Tests and diagnostics
The diagnosis is established on the basis of epidemiological history, clinical symptoms and laboratory tests, including:
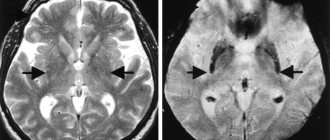
- microscopy of a blood smear, cerebrospinal fluid, punctate/biopsy specimen of the spleen, affected lymph nodes or bone marrow to detect trypanosomes in smears stained according to Romanovsky-Giemsa;
- immunological reactions (detection of IgM class antibodies in the blood serum of patients in diagnostic titers);
- biological method (infection of laboratory rats and mice by intraperitoneal injection of the patient’s blood).
Microbiological examination of cerebrospinal fluid/blood
Disease management: making a diagnosis
Disease management is carried out in three stages:
- Screening for possible infection. This includes serological testing (only available for Tb gambiense) and testing for clinical signs, particularly enlarged cervical lymph nodes.
- Search for parasites in biological fluids.
- Determining the stage of the disease. This involves a clinical examination of the patient and, in some cases, examination of cerebrospinal fluid obtained by lumbar puncture.
To avoid the need for complex and difficult treatment methods, diagnosis should be performed as early as possible before the development of the neurological stage of the disease.
Due to the long and asymptomatic course of the first stage of sleeping sickness caused by T. b. gambiense, careful and active screening of risk groups is recommended in order to identify patients at an early stage of the disease and limit further spread of infection through their treatment, after which they cease to act as a reservoir. Comprehensive population screening requires significant financial investment in human and material resources. In Africa, especially in remote areas where the disease is most prevalent, these resources are often in short supply. As a result, some infected people die before being diagnosed and receiving treatment.
Prevention
There is no specific prevention. Preventive measures are aimed at breaking the epidemic process and, above all,:
- to combat vectors, which involves burning/cutting down/treating with insecticides coastal shrubs, breeding sites and habitats of tsetse flies, as well as spraying insecticides in the cracks of agricultural buildings/in residential buildings to destroy kissing bugs;
- the use of various personal protective equipment: netting living quarters, using various traps, using bed nets, wearing special thick clothing treated with repellents;
- timely identification of patients;
- maintaining hygiene during transportation, storage, preparation and consumption of food;
- donor screening.
Public-private partnerships
In 2000 and 2001 WHO established a public-private partnership with Aventis Pharma (now Sanofi) and Bayer HealthCare, resulting in a WHO-led disease surveillance and control program that provides control support to endemic countries at no cost to medicines are supplied.
The partnership has been renewed several times in 2006, 2011, 2021 and 2021. Progress in reducing the incidence of sleeping sickness and the prospect of its elimination has prompted a number of other private sector partners to support the WHO initiative to eliminate the disease as a public health problem and ensure the elimination of transmission by 2030 G.
List of sources
- Lectures on tropical diseases: textbook / Compiled by: D.A. Valishin, D.Kh. Khunafina, A.N. Burganova, O.I. Kutuev, A.T. Galieva, L.R. Shaikhullina, V.I. Starostina, G.R. Syrtlanova - Ufa: Publishing house of the Federal State Budgetary Educational Institution of Higher Education BSMU of the Ministry of Health of Russia, 2021 - 239 p.
- Khojayan A.B. PROTOZOAL DISEASES OF HUMAN: a textbook for first-year students of the medical, pediatric, and dental faculties of St. State Medical University / A.B. Khojayan, E.N. Makarenko, A.K. Mikhailenko, N.N. Fedorenko, M.G. Gevandova, M.A. Kolomeitseva, N.N. Gromova. – Stavropol: Publishing house of St. State Medical University. –2013 –75s.
- Medical parasitology - G.I. Myandina, E.V. Tarasenko. Training manual, 2013
- "Guide to infectious diseases with an atlas of infectious pathology." Ed. Yu.V. Lobzina, S.S. Kozlova, A.N. Uskova, 2000
- Tropical diseases / Ed. Yu. A. Ilyinsky, V. M. Luchshev. - M.: Medicine, 1984. - 272 p.
Burden of disease
Sleeping sickness threatens the health of millions of people in 36 countries in sub-Saharan Africa. Many of them live in remote areas with limited access to necessary medical care, making surveillance and therefore difficult to diagnose and treat patients. In addition, population displacement, armed conflict and poverty are important factors facilitating transmission.
- In 1998, there were almost 40,000 cases of the disease, but the estimated number of undiagnosed patients who did not receive treatment was about 300,000.
- During the most recent epidemic, disease prevalence reached 50% in some rural communities in Angola, the Democratic Republic of the Congo and South Sudan. In these communities, sleeping sickness was the first or second leading cause of death, surpassing even HIV/AIDS.
- In 2009, systematic efforts to control the disease brought the number of reported cases to below 10,000 (9,878 cases) for the first time in 50 years. The decline in incidence continued in subsequent years, with 992 new cases reported in 2021, the lowest number in 80 years of systematic global collection of incidence data. The population at risk of the disease is estimated to be 65 million.