1.What is idiopathic thrombocytopenic purpura?
Idiopathic thrombocytopenic purpura (Werlhof's disease)
is the first disease that was identified and described from the group of human hemorrhagic diseases. The main symptom of ITP is increased bleeding. It is caused either by pathological changes in blood cells - platelets - or by a deficiency of their content in the blood. Most often (80% of cases) there is a quantitative deficiency.
Platelets
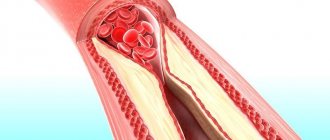
- These are the smallest blood cells. Each platelet lives from 2 to 10 days. Platelets are produced by the bone marrow, but they die in the spleen and liver. During the process of blood clotting, platelets become lumpy and increase in size unevenly. This promotes aggregation (sticking together) and adhesion (attachment to the walls of blood vessels), which causes the formation of a blood clot. The vessel closes, stopping the bleeding.
When the German physician Paul Gottlieb Werlhof described the disease that today we call idiopathic thrombocytopenic purpura, the composition of the blood had not yet been sufficiently studied. Only 150 years later, the disease was associated with a lack of platelets in the blood.
In a number of diseases characterized by thrombocytopenia, the term “idiopathic”
means the cause of this pathology is unknown.
The term “purpura”
in the name of the disease indicates the external manifestations of the disease: skin pinpoint and spotty hemorrhages, capillary hemorrhages, ecchymoses. On the surface of the skin they have a dark burgundy color.
Idiopathic thrombocytopenic purpura can occur acutely (up to six months) or have a chronic course.
The highest incidence occurs in school and preschool age. For children over 10 years of age, idiopathic thrombocytopenic purpura is diagnosed twice as often in girls than in boys.
A must read! Help with treatment and hospitalization!
Thrombocytopenic purpura (Werlhof's disease) is a disease characterized by a tendency to bleeding caused by thrombocytopenia (a decrease in platelet content in the blood to 150 × 109/l) with a normal or increased number of megakaryocytes in the red bone marrow.
Thrombocytopenic purpura is the most common disease from the group of hemorrhagic diathesis. The incidence of new cases of thrombocytopenic purpura ranges from 10 to 125 per 1 million population per year. The disease usually manifests itself in childhood. Before the age of 10, the disease occurs with equal frequency in boys and girls, and after 10 years and in adults - 2-3 times more often in females.
Etiology and pathogenesis
In thrombocytopenic purpura, thrombocytopenia develops due to the destruction of platelets through immune mechanisms. Antibodies to one’s own platelets may appear 1-3 weeks after viral or bacterial infections, preventive vaccinations, taking medications if they are individually intolerant, hypothermia or insolation, after surgery, or injuries. In some cases, no specific cause can be identified. Antigens that enter the body (for example, viruses, drugs, including vaccines) settle on the patient’s platelets and induce an immune response. Antiplatelet antibodies are classified predominantly as IgG. The Ag-AT reaction occurs on the surface of platelets. The lifespan of platelets loaded with antibodies in thrombocytopenic purpura is reduced to several hours instead of 7-10 days normally. Premature platelet death occurs in the spleen. Bleeding in thrombocytopenic purpura is caused by a decrease in the number of platelets, secondary damage to the vascular wall due to loss of angiotrophic function of platelets, impaired vascular contractility due to a decrease in the concentration of serotonin in the blood, and the inability to retract a blood clot.
Clinical picture
The disease begins gradually or acutely with the appearance of hemorrhagic syndrome. The type of bleeding in thrombocytopenic purpura is petechial-spotted (bruised). According to clinical manifestations, two variants of thrombocytopenic purpura are distinguished: “dry” - the patient experiences only cutaneous hemorrhagic syndrome; “wet” - hemorrhages combined with bleeding. Pathognomonic symptoms of thrombocytopenic purpura are hemorrhages in the skin, mucous membranes and bleeding. The absence of these signs raises doubts about the correctness of the diagnosis.
- Cutaneous hemorrhagic syndrome occurs in 100% of patients. The number of ecchymoses varies from single to multiple. The main characteristics of cutaneous hemorrhagic syndrome in thrombocytopenic purpura are as follows. Discrepancy between the severity of hemorrhage and the degree of traumatic exposure; their spontaneous appearance is possible (mainly at night).
- Polymorphism of hemorrhagic rashes (from petechiae to large hemorrhages).
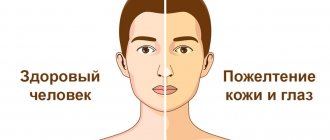
- Polychrome skin hemorrhages (color from purple to blue-greenish and yellow, depending on how long ago they appeared), which is associated with the gradual conversion of hemoglobin through intermediate stages of decomposition into bilirubin.
- Asymmetry (no favorite localization) of hemorrhagic elements.
- Painless.
- Hemorrhages often occur in the mucous membranes, most often the tonsils, soft and hard palate. Hemorrhages into the eardrum, sclera, vitreous body, and fundus are possible.
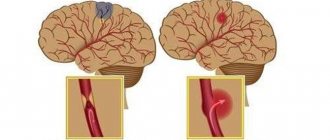
- Hemorrhage in the sclera may indicate a threat of the most severe and dangerous complication of thrombocytopenic purpura - hemorrhage in the brain. As a rule, it occurs suddenly and progresses rapidly. Clinically, cerebral hemorrhage is manifested by headache, dizziness, convulsions, vomiting, and focal neurological symptoms. The outcome of cerebral hemorrhage depends on the volume, localization of the pathological process, timely diagnosis and adequate therapy.
- Thrombocytopenic purpura is characterized by bleeding from the mucous membranes. They are often profuse in nature, causing severe posthemorrhagic anemia, which threatens the patient’s life. In children, bleeding most often occurs from the nasal mucosa. Bleeding from the gums is usually less profuse, but it can also become dangerous during tooth extraction, especially in patients with an undiagnosed disease. Bleeding after tooth extraction in thrombocytopenic purpura occurs immediately after the intervention and does not resume after its cessation, unlike late, delayed bleeding in hemophilia. In girls of puberty, severe menorrhagia and metrorrhagia are possible. Gastrointestinal and renal bleeding occur less frequently.
- Hemorrhagic crisis is characterized by severe bleeding syndrome and significant changes in laboratory parameters.
- During clinical remission, hemorrhagic syndrome disappears, bleeding time is reduced, secondary changes in the blood coagulation system are reduced, but thrombocytopenia persists, although it is less pronounced than during a hemorrhagic crisis.
- Clinical and hematological remission implies not only the absence of bleeding, but also the normalization of laboratory parameters.
- In hypo- and aplastic conditions, blood tests reveal pancytopenia. Red bone marrow punctate is poor in cellular elements.
- Extensive metaplasia in the red bone marrow is the main criterion for acute leukemia.
- Thrombocytopenic purpura can be a manifestation of diffuse connective tissue diseases, most often systemic lupus erythematosus. In this case, it is necessary to rely on the results of an immunological study. A high titer of antinuclear factor and the presence of LE cells indicate systemic lupus erythematosus.
- The main difference between thrombocytopenic purpura and thrombocytopathies is a decrease in platelet content.
- Prednisolone is prescribed at a dose of 2 mg/kg/day for 2-3 weeks, followed by a dose reduction and complete discontinuation of the drug. Prednisolone in higher doses (3 mg/kg/day) is prescribed in short courses of 7 days with a break of 5 days (no more than three courses). In cases of severe hemorrhagic syndrome and the threat of cerebral hemorrhage, “pulse therapy” with methylprednisolone (30 mg/kg/day intravenously for 3 days) is possible. In most cases, this therapy is quite effective. First, the hemorrhagic syndrome disappears, then the platelet count begins to increase. Some patients experience a relapse after stopping hormones.
- In recent years, in the treatment of thrombocytopenic purpura, intravenous administration of normal human Ig at a dose of 0.4 or 1 g/kg for 5 or 2 days, respectively (course dose of 2 g/kg) has been used with good effect as monotherapy or in combination with glucocorticoids.
- Splenectomy or thromboembolization of the vessels of the spleen is carried out in the absence or instability of the effect of conservative treatment, repeated heavy prolonged bleeding leading to severe posthemorrhagic anemia, severe bleeding that threatens the patient's life. The operation is usually performed against the background of glucocorticoid therapy in children over 5 years of age, since at an earlier age there is a high risk of developing post-splenectomy sepsis. In 70-80% of patients, surgery leads to almost complete recovery. The remaining children need continued treatment even after splenectomy.
- Immunosuppressants (cytostatics) for the treatment of thrombocytopenic purpura in children are used only if there is no effect from other types of therapy, since the effectiveness of their use is much less than splenectomy. Vincristine is used at a dose of 1.5-2 mg/m2 of body surface orally, cyclophosphamide at a dose of 10 mg/kg - 5-10 injections, azathioprine at a dose of 2-3 mg/kg/day in 2-3 doses for 1-2 months
There are no characteristic changes in internal organs with thrombocytopenic purpura. Body temperature is usually normal. Sometimes tachycardia is detected, during auscultation of the heart - systolic murmur at the apex and at Botkin's point, weakening of the first tone, caused by anemia. An enlarged spleen is uncharacteristic and rather excludes the diagnosis of thrombocytopenic purpura.
According to the course, acute (lasting up to 6 months) and chronic (lasting more than 6 months) forms of the disease are distinguished. During the initial examination, it is impossible to determine the nature of the course of the disease. Depending on the degree of manifestation of the hemorrhagic syndrome and blood parameters during the disease, three periods are distinguished: hemorrhagic crisis, clinical remission and clinical-hematological remission.
Laboratory research
Characterized by a decrease in the content of platelets in the blood, up to single ones in the drug, and an increase in bleeding time. The duration of bleeding does not always correspond to the degree of thrombocytopenia, since it depends not only on the number of platelets, but also on their qualitative characteristics. Retraction of the blood clot is significantly reduced or does not occur at all. Secondarily (as a result of thrombocytopenia), the plasma-coagulation properties of the blood change, which is manifested by insufficient thromboplastin formation due to a deficiency of the 3rd platelet factor. Impaired thromboplastin formation leads to a decrease in prothrombin consumption during blood coagulation. In some cases, with thrombocytopenic purpura during a crisis, activation of the fibrinolytic system and an increase in anticoagulant activity (antithrombins, heparin) are noted. All patients with thrombocytopenia have a reduced concentration of serotonin in the blood. Endothelial tests (tourniquet, pinch, hammer, prick) during a hematological crisis are positive. No changes are found in the red blood and leukogram (in the absence of blood loss). Examination of red bone marrow usually reveals normal or increased levels of megakaryocytes.
Diagnosis and differential diagnosis
Diagnosis of thrombocytopenic purpura is based on the characteristic clinical picture and laboratory data.
| Laboratory | Thrombocytopenia Increased bleeding time Reducing the degree of blood clot retraction |
Thrombocytopenic purpura must be differentiated from acute leukemia, hypo- or aplasia of the red bone marrow, systemic lupus erythematosus, and thrombocytopathies.
Treatment
During a hemorrhagic crisis, the child is prescribed bed rest with its gradual expansion as the hemorrhagic phenomena subside. No special diet is prescribed, however, if the oral mucosa is bleeding, children should receive chilled food.
Pathogenetic therapy for autoimmune thrombocytopenic purpura includes the administration of glucocorticoids, splenectomy and the use of immunosuppressants.
Recently, danazol (a synthetic androgenic drug), interferon preparations (reaferon, intron-A, roferon-A), anti-D-Ig (anti-D) have also been used to treat thrombocytopenic purpura. However, the positive effect of their use is unstable, side effects are possible, which makes it necessary to further study the mechanism of their action and determine their place in the complex therapy of this disease.
To reduce the severity of hemorrhagic syndrome during periods of increased bleeding, aminocaproic acid is prescribed intravenously or orally at the rate of 0.1 g/kg (contraindicated in hematuria). The drug is a fibrinolysis inhibitor and also enhances platelet aggregation. The hemostatic agent etamsylate is also used at a dose of 5 mg/kg/day orally or intravenously. The drug also has angioprotective and proaggregant effects. To stop nosebleeds, tampons with hydrogen peroxide, adrenaline, and aminocaproic acid are used; hemostatic sponge, fibrin, gelatin films.
When treating posthemorrhagic anemia in children with thrombocytopenic purpura, agents that stimulate hematopoiesis are used, since the regenerative abilities of the hematopoietic system are not impaired in this disease. Transfusion of washed red blood cells, selected individually, is carried out only in cases of severe acute anemia.
Prevention
Primary prevention has not been developed. Secondary prevention comes down to preventing relapses of the disease. When vaccinating children with thrombocytopenic purpura, an individual approach and special caution are required. Schoolchildren are exempt from physical education classes; Sun exposure should be avoided. In order to prevent hemorrhagic syndrome, patients should not be prescribed drugs that inhibit platelet aggregation (for example, salicylates, indomethacin, barbiturates, caffeine, carbenicillin, nitrofurans, etc.). After discharge from the hospital, children are subject to dispensary observation for 5 years. A blood test with platelet count is indicated once every 7 days, and then monthly (if remission is maintained). A blood test is required after every illness.
Forecast
The outcome of thrombocytopenic purpura can be recovery, clinical remission without normalization of laboratory parameters, a chronic relapsing course with hemorrhagic crises, and in rare cases, death as a result of hemorrhage in the brain (1-2%). With modern treatment methods, the prognosis for life is favorable in most cases.
Original article www.eurolab.ua Illustrations from the site: © 2011 Thinkstock.
Source: Children's diseases. Baranov A.A. // 2002.
2. Causes of Werlhoff's disease
Causes of ITP
not clearly established.
A third of patients before the onset of the disease do not receive any influences that could affect their health. The rest have a number of factors that can theoretically be considered etiological,
but the real cause-and-effect relationship with the disease has not yet been proven for them:
- viral and bacterial diseases;
- taking medications;
- excessive insolation;
- hypothermia;
- operations;
- injuries;
- vaccinations.
The normal content of platelets in the blood is ensured by the balance of two constantly occurring processes: the formation of new platelets and their destruction in the peripheral bloodstream. Patients with idiopathic thrombocytopenic purpura have an increased rate of platelet destruction.
Although the reasons for this disorder remain not entirely clear, it can now definitely be said that the mechanism that provokes chronic
intensive destruction of platelets, is immunological in nature. The lifespan of platelets is reduced from several days to several hours. Their production in the bone marrow remains at the same level. Sometimes reproduction increases (as a reaction to an imbalance), but this does not sufficiently compensate for the platelet deficiency. The further course of complex physiological compensatory immune processes often only intensifies thrombocytopenia, since platelet deficiency is added to their inferiority, which, in turn, leads to the inability of even existing cells to perform blood clotting functions. Chronic idiopathic thrombocytopenic purpura is autoimmune in nature. In this case, a lifelong disorder of blood composition with periods of remissions and exacerbations is predicted.
If a decrease in platelet content in the blood is caused by the action of any known factor, then when it is eliminated, thrombocytopenia stops and blood clotting is restored. This form of the disease is considered acute
and has a favorable prognosis.
The primary manifestation of the disease in the form of skin hemorrhages occurs when the platelet count decreases to 30–50 x 109/l. Bleeding from the nose and mucous membranes begins at 20–30 x 109/l. If platelet counts drop to 10 x 109/L or less, there is a serious risk of hemorrhagic stroke and spontaneous gastric bleeding.
Visit our Therapy page
3. Symptoms of the disease
The symptoms of ITP are divided into two types of the disease: dry and wet.
In the first case, only subcutaneous capillary hemorrhages are observed. With wet thrombocytopenic purpura, external bleeding from the nose and mucous membranes also occurs. In both cases, bleeding begins for no apparent reason. More often, spots appear at night, when a person is practically motionless and the likelihood of mechanical damage is excluded. In patients with idiopathic thrombocytopenic purpura, the disease does not affect the internal organs. The body temperature is normal, the lymph nodes are not enlarged, there are no symptoms of intoxication or inflammation.
Hemorrhages on the skin occur mainly on the front surface of the body, on the forehead and extremities. There is never any subcutaneous bleeding on the palms or soles. External bleeding - from the nose, gums, tonsils, eyes, as well as uterine and stomach.
About our clinic Chistye Prudy metro station Medintercom page!
4.Diagnostics and treatment
Diagnosis of ITP
is based on thrombocytopenia, which can be easily detected by a clinical blood test or a coagulogram - a clotting test. It is more difficult (and more important) to differentiate this disease from other diseases with thrombocytopenic symptoms.
During the period of exacerbation of ITP, a positive reaction to a number of tests is observed:
- tourniquet test (positive if, when applying a tourniquet to the shoulder, small hemorrhages form on the skin of the shoulder and forearm),
- hammer test (positive if bruises occur when moderately tapping the skin with a hammer),
- pinch test (positive if pinching the skin under the collarbone within 24 hours produces petichiae or bruising),
- prick test (positive if, after an injection with a scarifier, the wound bleeds for more than 4 minutes).
Treatment of idiopathic thrombocytopenic purpura
most often symptomatic. If blood clotting rates are low, the patient is hospitalized. Bed rest is indicated. For anemia and prolonged bleeding, appropriate therapy is used. As the severity of the condition decreases, you are gradually allowed to get up and move.
Typically, the disease of idiopathic thrombocytopenic purpura sooner or later ends in spontaneous self-healing or long-term remission. Only in 1-2% of cases the disease leads to cerebral hemorrhage with a fatal outcome, and that is why secondary prevention includes reducing physical activity, gentle activity, and special monitoring during vaccinations, surgical treatment, and dental procedures. It is necessary to know the factors that reduce platelet production and avoid exposure to them.
Treatment of pathology
Treatment of thrombocytopenic purpura is aimed at:
- restoration of normal platelet levels and adequate bone marrow activity;
- prevention of bleeding;
- removal of autoimmune complexes from the bloodstream.
The treatment regimen is developed for each patient individually and depends on the severity of the patient’s condition and the degree of progression of TP.
Pharmacotherapy
Treatment with corticosteroids, thrombopoietin receptor agonists (stimulation of hematopoiesis), immunosuppressive drugs, and intravenous immunoglobulins is used.