Midriaz
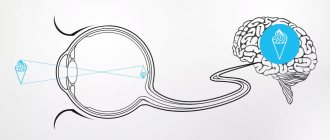
Mydriasis is the dilation of the pupil under the influence of irritants. The process is ensured by relaxation of the optic sphincter - the circular muscle responsible for narrowing the pupil. Physiological mydriasis occurs reflexively, for example, when the lighting becomes worse, or if a person looks into the distance. Mydriasis is characteristic of states of stress and fear (remember the proverb “Fear has big eyes”?), as well as surprise, joy, and euphoria.
The main difference between physiological mydriasis and other varieties is that the dilation of the pupil is always temporary. As soon as the stimulus disappears (the lighting becomes brighter, the person calms down), the pupil diameter again approaches normal - 2-4 mm. Another symptom of pathological mydriasis is uneven pupil dilation.
Large (wide) pupils - causes and treatment
In a healthy state, the pupils change in size depending on the lighting: in bright light they narrow to protect the eyes from excess light, and in the dark they dilate so that even in dim lighting they allow as many rays of light as possible into the eye.
At the same time, the pupils dilate and contract synchronously: they remain the same size in comparison with each other.
But it happens that pupil dilation occurs regardless of lighting. Most often this is a sign of pathology, and not always related to the eyes.
Glaucoma
Diabetes
Vomit
1627 20 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Glaucoma: causes, symptoms, diagnosis and treatment methods.
Definition
Glaucoma is not one disease, but a whole group of serious diseases of the visual organ with similar symptoms:
- increased intraocular pressure (can be constant or episodic);
- damage and subsequent atrophy of the optic nerve;
- decreased visual acuity, impaired visual functions.
Causes of glaucoma
The space of the eye, filled with a clear liquid and limited on one side by the cornea and on the other by the iris, is called the anterior chamber. It contains an area called the anterior chamber angle, in the outer wall of which there is the drainage system of the eye, which provides controlled outflow of intraocular fluid.
Fluid circulation maintains intraocular pressure at a constant level, and disruption of its function entails its increase.
Intraocular pressure is considered a major factor in assessing the health of patients who are at risk of developing glaucoma. Normally, the pressure in the eye is 18-24 mmHg. Art. With glaucoma, the balance between the formation of intraocular fluid and its outflow is disrupted, intraocular pressure increases, which leads to atrophy of the optic nerve.
There are two main forms of glaucoma, each with its own characteristics:
Open angle – occurs in 90% of cases and is characterized by an open (wide) iridocorneal angle, but with a disorder in its functioning.
Closed-angle - is rare, mainly in people suffering from farsightedness after 35 years.
Congenital glaucoma is diagnosed in newborns and one-year-old children, and its development is associated with congenital eye pathology that impedes the outflow of fluid. Often this type of glaucoma is a consequence of intrauterine infections (rubella, mumps, toxoplasmosis). In addition, the development of the disease can be influenced by external factors, for example, radioactive radiation, poisoning of a pregnant woman with chemicals, etc.
All types of glaucoma develop when the circulation of fluid in the eye is impaired. But with open-angle glaucoma, the angle along which the intraocular fluid flows out does not overlap. The main problem arises in the drainage system of the eye, which, becoming less passable, gradually ceases to allow intraocular fluid to pass through. The closed-angle form, as a rule, occurs acutely - the increase in intraocular pressure occurs sharply and suddenly.
Risk factors for developing acquired glaucoma include:
- age over fifty years;
- periodically increasing intraocular pressure;
- high degree of myopia after 40-50 years;
- high degree of farsightedness (especially women after 50 years);
- low blood pressure;
- eye injuries, inflammatory eye diseases (uveitis, iridocyclitis, etc.), eye surgeries;
- chronic eye diseases;
- diabetes mellitus, obesity;
- dysfunction of the hormonal and nervous systems;
- diseases of the cardiovascular system;
- chronic stress;
- hereditary predisposition;
- long-term use of certain medications (hormonal drugs, antihistamines, antidepressants, etc.).
According to WHO, glaucoma is the leading pathology of the visual system, leading to vision loss.
In Russia, the number of cases is estimated at about a million people. Glaucoma is the second most common cause of blindness, second only to cataracts.
Classification of the disease
By origin:
- primary glaucoma, in which changes in the circulation of intraocular fluid occur primarily, and symptoms develop secondarily;
- Secondary glaucoma develops against the background of other eye pathologies or somatic diseases. There are always organic reasons that disrupt intraocular pressure.
According to the level of intraocular pressure:
- hypertensive glaucoma – with an increased level of intraocular pressure;
- Normal pressure glaucoma is a poorly understood type of eye pathology in which damage to the optic nerve occurs when intraocular pressure is normal.
According to the course of the disease:
- stabilized glaucoma - with long-term observation of the patient (at least 6 months), no deterioration in the state of the visual field and optic nerve head is detected;
- unstabilized glaucoma - deterioration in the visual field and optic nerve head is recorded during repeated examinations. When assessing the dynamics of the glaucomatous process, the level of intraocular pressure and its compliance with the “target” value are also taken into account.
According to the degree of damage to the optic nerve:
Stage I (initial) - no visible changes. The patient, as a rule, has no complaints. The disease is usually detected at this stage during a preventative visit to an ophthalmologist.
Stage II (developed) - it is at this stage that glaucoma is most often detected, when more than 60% of the optic nerve fibers are already affected. The level of intraocular pressure is higher. There is a significant (more than 10%) narrowing of the field of view on the nasal side.
Stage III (advanced) - characterized by pronounced changes in the optic nerve, narrowing of the visual fields, which is less than 15% of the point of fixation, excavation (depressions of various shapes and sizes) of the optic nerve head.
Stage IV (terminal) - complete loss of visual acuity and field of vision or preservation of light perception with incorrect projection. Sometimes a small island of the visual field is preserved in the temporal sector. Total excavation. The doctor states complete atrophy of the optic nerve. Very high intraocular pressure figures are noted.
By patient age:
- congenital glaucoma (up to 3 years);
- infantile glaucoma (from 3 to 10 years);
- juvenile glaucoma (from 11 to 35 years);
- glaucoma in adults (over 35 years old).
Symptoms of glaucoma
Main symptoms of the disease:
- the appearance of so-called rainbow circles around light sources;
- blurring and concentric (from the periphery to the center) narrowing of lateral vision;
- sporadic headaches;
- eye pain;
- a sharp decrease in visual acuity in a very short period of time;
- a periodic feeling of pain, pain and heaviness in the area of the affected eye;
- decreased field of view;
- decreased vision at dusk and at night;
- eye moisture;
- hyperemia of the eyeball.
In the open-angle form, the symptoms do not appear or are blurred, so the decrease in the radius of the visual field occurs unnoticed and can develop over 2-3 years.
Sometimes patients complain of a foggy veil before the eyes or colored spots that appear when looking at a bright light source. A person may accidentally discover that one eye has only partial vision. Sometimes signs of fatigue appear during intense visual work. With the angle-closure form, there is a sharp increase in intraocular pressure, which leads to the development of characteristic symptoms: acute pain in the affected eye, migraine, hyperemia of the eyeball, swelling of the eyes, decreased vision up to its complete loss, the pupil dilates and does not respond to light. Sometimes an optical phenomenon occurs - when looking at a light source, the patient sees a halo (luminous ring) around it.
Signs of an attack of glaucoma are:
- unprovoked acute pain in the eye;
- rainbow circles and a catastrophic decrease in visual acuity in the affected eye;
- headache in the frontal and temporal regions from the affected eye;
- sudden nausea and vomiting;
- bradycardia.
Diagnosis of glaucoma
For early detection of pathological processes, intraocular pressure is measured, the fundus and optic nerve head are examined, and a visual field study is performed to identify defects in central and peripheral vision. Tonometry is carried out repeatedly during the initial diagnosis, and during further observation - at each follow-up examination by an ophthalmologist.
To diagnose glaucoma, a comprehensive examination may be prescribed:
- study of the visual field (using a computer perimeter);
- measurement of refraction (the ability of the optical system of the eye to refract light rays);
- measurement of intraocular pressure;
- ultrasound examinations;
- determining the depth of the anterior chamber of the eye and the thickness of the lens (since high pressure is often caused by displacement or enlargement of the lens);
- determination of corneal thickness;
- biomicroscopic studies
- Using gonioscopy, the structure of the anterior chamber angle, through which fluid outflows from the eye, is assessed.
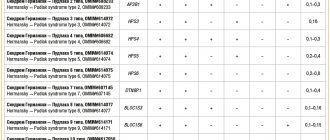
Determination of genetic predisposition to the development of the disease:
- juvenile open-angle glaucoma (Rieger syndrome);
Treatment of dilated pupils
There is no specific recipe for getting rid of this symptom: it all depends on the reasons that caused this condition. We recommend that you first contact an ophthalmologist, and then, if necessary, the doctor will recommend that you visit a related specialist.
Remember to get regular eye exams. Consistent visits to an ophthalmologist reduce the risk of developing serious eye pathologies. The earlier a problem is detected, the easier it is to solve it. Come to the Eye Clinic of Dr. Belikova, we are always happy to help you 
Diagnostics
To make a diagnosis, the specialist must obtain as complete an anamnesis as possible. He will find out what events happened before this, ask about the patient’s lifestyle, past illnesses, and how long mydriasis has been observed.
Sometimes an examination by several doctors is required: a neurologist, an ophthalmologist, a neurosurgeon. In addition, a blood test and magnetic resonance imaging are required, which will determine whether there are tumors inside the head. Only a thorough medical history will help a specialist establish the true cause of pathological mydriasis.
Concealing puncture marks
If there are many traces of intravenous injections on a person’s body, then for others this is the most obvious sign of drug addiction, which simply catches the eye. These traces can be seen by any loved one, friend or relative of a drug addict.
And if he compares it with other signs, for example, strange behavior, he will make a clear conclusion about the person’s drug addiction. Of course, when a drug addict begins to be asked questions about the nature of these traces, he has to come up with various, sometimes very ridiculous, options for their origin.
Versions may vary. From a squeezed pimple to scratches from a cat's claws. However, even a person who is far from medicine or drugs will be able to distinguish traces of injections from other skin lesions.
If you look closely at the marks on the skin, you will see the entrance hole of the needle in the form of a small red dot at the injection sites. Very often a small bruise will form around the injection site. For experienced drug addicts, injection points form entire “roads” because they follow each other.
When a drug addict injects many times in a row into the same vein, a “well” can form at that spot. Each new injection expands and deepens it, making it more distinct and noticeable.
If you take a closer look at the “roads” of a drug addict, you can see a certain pattern. This is a clear sign that the person is injecting drugs into a vein. After all, “roads” follow only along the lines of veins.
But stubborn in their desire to hide their drug addiction, people pass off even the most obvious “roads” as ordinary scratches, and explain the appearance of “wells” as burns. Everything depends only on the degree of development of the drug addict’s imagination.
Masking of injection marks occurs by regularly applying various ointments to the injection sites, which serve against the appearance of blood clots. CU such ointments include: troxevasin, hepatrombin and the like. Using these ointments, drug addicts get rid of bruises in a matter of days.
Another way to hide marks from injections is a method in which injections are made only in those areas of the body that are not visible to others. For example: groin area, legs, neck below and under the hair, back of the forearm or armpit.
With injections in the groin, the drug addict can afford to wear T-shirts and shorts in the hot summer, no different from other people. True, any drug addict is immediately betrayed by huge circles under the eyes and painful thinness.
Those drug addicts who do not inject drugs in any way, intramuscularly or intravenously, but only smoke narcotic mixtures or snort drugs, are not much different from other people. And recognizing them as drug addicts is quite difficult. It must be said that those drug addicts who are afraid for their loved ones or do not want anger on their part come to such drug use.
Medicines
As Devin McKay, director of the department of neuro-ophthalmology at Indiana University School of Medicine, notes in an interview with Insider, some drugs affect the signals generated by the brain. Thus, the pupils sometimes dilate or contract on their own.
Antihistamines like Claritin or Benadryl affect this; motion sickness medications containing scopolamine; stimulant medications, such as Adderall; tricyclic antidepressants; anti-seizure medications; Botox.
Before taking these medications, the doctor usually checks with the person to see if he or she has eye problems: for example, scopolamine should not be used by people with glaucoma - the drug can increase the risk of blindness.
Predisposition
Some people live with benign episodic unilateral mydriasis, a condition in which the pupil of one eye dilates on its own. According to Devin McKay, it can stay this way for a couple of minutes, hours, even days, before returning to its normal size.
The causes of DEOM are not known for certain; however, it is clear that the condition often affects young women prone to migraines. Benign mydriasis itself is harmless, but sometimes it can cause problems when choosing glasses or contact lenses.
Attraction
Liking a particular person stimulates the nervous system, after which the body releases dopamine, norepinephrine and serotonin.
The release of hormones affects the size of the pupils. Employees of the Healthline service, by the way, note that such a mechanism was justified by the biological need for reproduction. There is an assumption that a woman’s dilated pupils signal her desire to conceive a child from a certain partner. Men primarily reacted to women with “very black” eyes, understanding that such companions were interested in them - in this case, they could pass on their genes.