1.Pain in legs
Almost all people at some point in time experience problems with their legs - pain in the legs, pain in the feet, toes, ankles and other unpleasant sensations.
Why is this happening? In fact, there can be many reasons. Most of the time, our body movements do not cause any problems. But due to daily or too intense stress, a variety of leg diseases can develop. In addition, injuries and the natural aging process can cause discomfort and pain in the legs.
Your toes, feet, and ankles may experience burning, pain, fatigue, numbness, tingling, warmth, or coldness
.
muscle spasms
occur in the legs, especially at night when you sleep, and swelling of the legs.
The feet and ankles may become discolored, pale, or blue
.
There may be an unpleasant odor from your feet
.
Some of these symptoms are normal for older people or pregnant women. In this case, treatment at home is usually sufficient. In other situations, you need to find the cause of the problem and treat it.
Bemer therapy is a modern way to combat all types of pain. You can read more about Swiss physiotherapy in this section
Sign up for a consultation
A must read! Help with treatment and hospitalization!
Osgood-Schlatter disease
Osgood-Schlatter disease (sometimes also called Schlatter disease or osteochondrosis of the tibial tuberosity) is an inflammation in the upper part of the tibia, where the patellar tendons attach to the tubercle called the tibial tuberosity. This disease is often the cause of knee pain in adolescence (from 10 to 15 years), is associated with the growth of the musculoskeletal system, and as growth completes, the symptoms may disappear.
Osgood-Schlatter disease can cause pain, swelling, and tenderness in the area of the front of the knee, below the kneecap. As a rule, one knee is affected (sometimes it happens on both sides). Symptoms worsen when the tendon attached to the tibial tuberosity is stressed (for example, when jumping). The diagnosis is made on the basis of radiography. The main goal of treatment is aimed at preventing symptoms (reducing certain types of stress, immobilization during exacerbation, physiotherapy). Surgical treatment methods are rarely used.
2.Causes of leg pain
There are several categories of problems that can cause leg pain, discomfort and the other symptoms listed above. Let's try to figure it out in more detail.
Firstly, it may be problems with the skin of the legs
. Symptoms and the diseases that cause them may be:
- If while walking you feel as if you are walking on stones or pebbles, it may be plantar warts on the lower part of your foot;
- Areas of dense and hard skin on the heels may appear due to calluses, blisters on the skin or engorgement of the skin due to uncomfortable shoes, walking barefoot;
- Redness, peeling of the skin, burning and itching between the toes or on the bottom of the leg are signs of foot fungus (mycosis). Another possible cause is dermatitis due to the shoes you wear;
- Red, swollen, and tender skin around the nail may be symptoms of an ingrown toenail or nail infection (paronychia);
- Redness, swelling of the feet, pain in the feet when walking or touching are signs of a possible bacterial infection. You can become infected in public showers, swimming pools and other similar institutions.
The toe joints are a very vulnerable area.
. And it is with the joints of the toes that there are more problems than with any other joints in the body.
- Big toe joint pain, redness, swelling and tenderness that suddenly appears in the big toe joint can be caused by gout. The same symptoms can appear due to infection;
- If you have a swelling or lump at the base of your big toe, it may be a bunion;
- A lump on the outside of the little finger may be due to bunion;
- Toe joint pain, stiffness, and swelling are common symptoms of bunions, arthritis, lupus, or gout.
Foot pain may appear in the front of the foot or in the heel.
- Sharp pain in the bottom of the heel can be caused by plantar fasciitis;
- Pain in the back of the heel or ankle are symptoms of Achilles tendinitis, or as it is also called, Achilles tendinitis;
- Pain that worsens before or after exercise but improves during exercise may be caused by a broken bone in the leg (usually a metatarsal);
- Small bone spurs under the heel bone that cause heel pain may be a heel spur;
- Pain in the midfoot occurs due to flat feet;
- Pain in the back of the heel or a lump in this area is a symptom of a type of bunion.
Many diseases can affect the nerves of the foot
, causing foot pain, numbness, tingling and burning.
- Foot pain, burning, tingling, or numbness between the toes, especially between the third and fourth toes, and the same sensation in the forefoot may occur due to swelling or thickening of the nerve in the forefoot;
- Pain, numbness, or tingling that starts in the back or buttocks and moves down the leg may be caused by sciatica due to a pinched nerve;
- Weakness and pain in the ankle, which is often accompanied by numbness, can begin due to a pinched nerve in the ankle (tarsal tunnel syndrome) or sciatica;
- Burning in the legs, numbness and loss of sensation appear due to poor blood circulation. This problem is more common among people with diabetes or peripheral artery disease.
As you can see, the causes of leg pain, pain in the feet, ankles, toes, and other causes of discomfort in the legs can be very different. Therefore, if you experience symptoms such as pain in the legs, swelling of the legs, cramps in the legs, burning sensation, numbness, tingling in the legs and toes, paleness or blueness of the legs, you need to consult a good doctor. A specialist will help determine the cause of discomfort in the legs and tell you how to deal with them.
Visit our Therapy page
Physiological edema
Swelling of the legs can be caused by physiological reasons, that is, be a consequence of special circumstances affecting a healthy body, and not a manifestation of a disease. These reasons include:
- salty food. Salt binds water. And if you eat a lot of salty foods, especially at night, you may notice swelling in the morning;
- alcohol. Alcohol also retains water. Therefore, after drinking alcohol, a person looks puffy. The problems are not limited to the face; the legs can also swell;
- hot weather. In the heat, blood vessels dilate as the body tries to normalize heat exchange. More blood flow means the risk of congestion and swelling in the legs increases;
- prolonged sitting or standing. If the legs are in one position for a long time, the blood stagnates in them, which leads to swelling. The worst thing is to sit with your legs crossed. Standing in one place for a long time is also not useful. Swelling of the legs is typical for people in standing professions - hairdressers, salesmen, cooks;
- uncomfortable shoes. If shoes disrupt normal blood circulation in the foot (high heels, narrow arches, tight straps), wearing them will lead to swelling.
3. Treatment of pain in the legs (ankles, feet, toes)
Treating leg pain at home often helps to cope not only with pain, but also with other symptoms - swelling of the legs, cramps, and discomfort. Treatment, as a rule, begins with eliminating the factors that caused pain in the legs.
and other unpleasant sensations.
For example, you should stop exercising at least temporarily if you experience pain in your legs (feet, ankles, or toes) during exercise. Physical activity “through pain” is contraindicated. It is important to wear high-quality and comfortable shoes. Arch supports and other orthopedic devices
will help make walking more comfortable.
Cold application, rest, foot massage, gentle and gentle exercises
(for example, for stretching tendons) will help cope with leg pain, leg swelling or cramps. To relieve leg pain, you can take over-the-counter pain medications.
For swelling of the legs, swelling of the feet and ankles
You can raise your swollen legs just above the level of your heart and sit like that for a while. If you have a sedentary job, get up and walk around for a few minutes every hour. Reduce your salt intake.
If your home treatments for leg pain (feet, ankles, toes), leg swelling, and other problems do not have the desired effect, consult your doctor. Consultation with a specialist is required
and when the pain and swelling intensify, signs of infection appear, the skin turns pale, tingling and numbness appear.
About our clinic Chistye Prudy metro station Medintercom page!
What to do before visiting a doctor.
Do leg exercises regularly, lead a healthy lifestyle, follow a diet and exercise, and visit the pool. It is necessary to wear comfortable shoes with orthopedic insoles, while trying to wear high-heeled shoes or, conversely, ballet flats or sneakers with flat soles as little as possible. In the evening, do a separate contrast shower for your feet - alternating warm and cool water, and place a pillow under your feet at night.
It is certainly necessary to follow these traditional recommendations if your legs ache. However, given the range of possible diseases that can cause this condition, you should not delay visiting a doctor and receiving specialized help.
Ivan Ilyich Kalachev, Ph.D. phlebologist, head of the surgical department of the Clinic of Expert Medical Technologies
4.Bemer therapy
In our medical practice, Bemer therapy has proven to be the most successful way to combat any type of pain. BEMER therapy is electromagnetic physiotherapy from Switzerland, the main goal of which is to improve blood circulation.
The Bemer device consists of three elements: an induction mattress aimed at general health improvement, a reinforced applicator - a device that allows you to influence a specific place, and a laser magnet, which has the strongest effect on the pain point
read more about Bemer therapy by following the link. If you want to get a consultation or make an appointment, you can do this using the feedback form or by phone: +7-495-212-08-85
Sign up for a consultation
Medicines
Some medications can cause leg problems due to side effects. Combination with smoking or drinking alcohol increases the risk of drug side effects. The main groups of drugs that can cause leg problems:
- Drugs that cause blood clots (for example, contraceptives)
- Neuroleptics (aminazine, haloperidol)
- Beta-2 receptor agonists (terbutaline or albuterol)
- Antihypertensive drugs (nifedipine, amlodipine or nicardipine)
- Statins are drugs that lower blood cholesterol levels (simvastatin or atorvastatin).
- Estrogens
- Lithium preparations
- Diuretics (Lasix and others)
- Opiates
- Steroids
If you are taking medications (especially long-term), you should inform your doctor about the occurrence of pain or cramps in the legs.
Neurogenic myalgia
Neuromuscular diseases, when muscle function is disrupted, i.e. damage to the muscles themselves or due to dysfunction of the neuromuscular junction, diseases of the spinal cord, damage to peripheral nerves or damage to the motor nuclei of the brain stem.
With osteochondrosis of the thoracic and lumbar spine, there may be plexopathies, radiculopathy, plexoradiculopathy. You are concerned about pain, limited movement, impaired sensitivity, muscle atrophy, paresis and paralysis may develop.
Progressive muscular dystrophies are genetic hereditary diseases and most often occur in childhood.
Inflammatory myopathies or myositis can occur due to inflammation or due to autoimmune diseases.
Mitochondrial myopathies are hereditary diseases, the cause of which is disruption of the functioning of mitochondria - the “power stations” of cells in which most of the ATP necessary for the cell is synthesized. This is a huge spectrum of diseases.
There are several different mitochondrial diseases with primary involvement of striated muscle or combined involvement of muscle tissue and the brain:
- — Kearns-Sayre syndrome is characterized by ophthalmoplegia, ataxia, muscle weakness, cardiac conduction disturbances, etc.;
- - MELAS syndrome - encephalomyopathy, lactic acidosis, stroke-like episodes;
Leber's optic neuropathy - acute loss of central vision in young men and many others.
Conditions associated with disruption of cellular energy are very common and are not limited to hereditary syndromes. Among them: chronic fatigue syndrome, migraines, cardiomyopathies, glycogenosis, connective tissue diseases, diabetes, rickets, hypoparathyroidism and many others.
The diagnosis of mitochondrial myopathies is based on morphological diagnosis and identification of the RRF phenomenon (“regged” red fibers, “torn” or “rough” red fibers).
Venous thrombosis
The occurrence of pain during thrombosis (blockage of a vein with a blood clot) is promoted by inflammation of the vessel wall or surrounding tissue. In addition, impaired outflow can lead to swelling and discoloration of the skin (pallor, cyanosis, redness). Pallor can be detected in the early stages of thrombosis of the veins of the iliofemoral region. Cyanosis is caused by congestive hypoxia and, as a rule, occurs with obstruction of the proximal veins of the leg. Pain during thrombosis can be aching, sharp or dull, intense and moderate. Often the pain intensifies when walking or carrying heavy objects. Pain may be relieved by lying down with your legs elevated. With superficial vein thrombosis, diagnosis is not difficult. If there is a suspicion of deep vein thrombosis, then objective research methods are necessary.
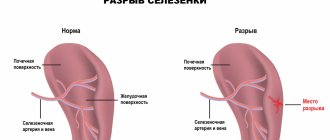
Rupture of popliteal cyst (Baker's cyst)
The fluid contained in a Baker's cyst, when ruptured (in the case of injury, arthritis or surgery in the knee joint), can flow down into the intermuscular space and cause an inflammatory reaction. This may manifest itself as pain, swelling in the lower leg, tenderness on palpation and resemble the picture of venous thrombosis. Rupture of a Baker's cyst can occur without provoking reasons. The diagnosis can be made based on radiography. But the possible combination of cyst rupture and venous thrombosis requires first of all the exclusion of thrombosis.
Diagnostics
First of all, to diagnose the cause of pain, the doctor needs to get answers to a number of questions:
- Localization of pain
- Presence of pain in one or two limbs
- Nature of pain (sharp, dull)
- Dependence of pain on time of day
- Dependence of pain intensity on physical activity
- Possibility of reducing pain when raising legs
- The presence of other symptoms (fever, weakness, lower back pain).
In addition, the doctor will conduct a physical examination (visual examination, palpation, various tests). Instrumental examination methods:
- Laboratory research
- Ultrasound of the vessels of the lower extremities (Dopplerography of veins and arteries)
- Arteriogram
- Scintigraphy
- MRI
- CT
- Radiography
Diagnostic measures
The presence of a specific pathology, as well as its exact cause, can only be determined during a face-to-face consultation with a specialist. During it, the doctor will ask several general questions regarding lifestyle and chronic diseases, study the medical history in detail, conduct some functional tests, and clarify the presence of similar pathologies in close relatives. As part of the examination, the doctor will ask you about the frequency and intensity of your symptoms, monitor your clinical picture, and identify the suspected etiology of the disease.
If suspicions are partially confirmed, you will be prescribed simple tests:
Rheovasography (RVG) is a non-invasive functional method for assessing pulse blood supply to the extremities, as well as the tone, elasticity and patency of peripheral vessels using a specific device;
Measurement of the brachial-ankle index - a one-time determination of the level of blood pressure in the area of the shoulders and ankles (normally it is the same);
Biochemical blood test (cholesterol content), and other tests to detect cardiac dysfunction.
For a more in-depth study of the course of the disease, the following measures are taken:
1. Duplex scanning of arteries and veins;
2. Angiography using a contrast agent;
3. Magnetic resonance angiography;
4. Multislice computed tomography of the lower extremities;
5. Functional tests.
At-risk groups
Patients with the following problems are most susceptible to vascular diseases of the lower extremities:
· Long history of smoking;
· Diabetes mellitus types 1 and 2;
· Alcohol abuse;
· Prolonged physical inactivity;
· High blood pressure;
· Hypercholesterolemia (increased concentration of cholesterol and triglycerides in the blood);
· High level of non-proteinogenic amino acid homocysteine in the blood;
· Obesity;
· Severe hormonal imbalance.
Pathologies of blood vessels and arteries of the legs mainly affect people who have crossed the threshold of fifty years of age, but in the last few years their active spread has also been observed among the young population. Men are more susceptible to such diseases than women.
It should be emphasized that most vascular dysfunctions are of a psychological nature, and people with a stressful type of character are most susceptible to them.
It is important to have a family history of disorders. This is especially true for atherosclerosis and varicose veins.
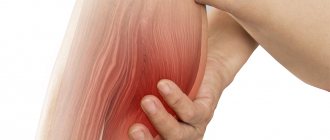
Muscle rupture
Most often, muscle ruptures occur in the lower leg (possibly in the thigh). A rupture occurs as a result of a sudden stretch or contraction of a muscle. Typically, a small section of muscle is torn where it connects to the tendon. But there are also large ruptures, up to separation of the muscle from the tendon or separation of the tendon. Muscle rupture occurs mainly when the limb is sharply flexed in the direction opposite to the acting force. The rupture is accompanied by acute pain immediately after excessive stress. The pain may subside for a while, but as the hematoma grows, the pain will gradually intensify. Swelling occurs in the area of the damaged muscle and range of motion is limited.
Bone damage
Damages to the bone tissue of the lower extremities (tumors, subperiosteal hematomas, fractures) may be accompanied by pain, tenderness to the touch, and swelling of the limb. Clinical manifestations may be similar to venous thrombosis. It can be especially difficult to diagnose a hip fracture in older people (the fracture is often accompanied by swelling of the lower limb). Considering the involutional changes in the central nervous system (cerebral vascular sclerosis), it is sometimes difficult to collect an anamnesis in this category of patients. In addition, elderly people often have a combination of a femoral neck fracture with venous thrombosis.