Open wound - symptoms and treatment
The pathogenesis of wounds has been studied in detail. The treatment of wounds is based on it. The invariability of pathogenetic links during injury allows us to speak of the wound process and its course as a general complex of typical manifestations characteristic of any wound, regardless of its morphology.
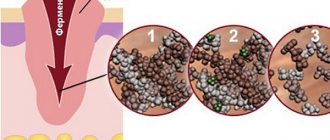
There are different classifications of terminologies and phase durations, but Ross's classification has earned worldwide recognition. According to it, there are three phases of the wound process:
- inflammatory phase;
- proliferative phase;
- reorganization phase.[11]
Inflammatory phase
In the first phase, an acute vascular reaction occurs, characterized by:
- vasospasm (narrowing of arteries and capillaries) for the purpose of local hemostasis (stopping bleeding);
- release of humoral coagulation factors, catalysts of local immune reactions.
The task of the inflammatory phase is to mobilize the body’s forces in order to localize the process and prepare for successful reparation (recovery) in the future.[12]
The second stage of this phase consists of the body eliminating (eliminating) damaged structures. The duration of these processes is from three to five days. After which the next stage of the wound process begins.
Proliferative phase
As the name implies, during this period the restoration of damaged and replacement of lost tissue begins.
In order to avoid “condomism” and a mechanistic understanding of the wound process, we note right away that the phases can intersect and run in parallel, being a single process, artificially separated for the purpose of convenience of study.[13]
As a rule, this phase lasts from several days to several weeks. There is a direct relationship with the amount of tissue lost during injury. The proliferative phase is based on the predominance of synthesis processes due to precursor cells.[14]
Reorganization phase
Considering the body’s limited capabilities for repair, regeneration occurs due to connective tissue, as the most universal and “suitable” substance for closing a defect with satisfactory plastic and functional effects. In this phase, fibroblasts and endothelial cells are active, which form tissue rich in collagen, permeated with newly formed capillaries. From the point of view of pathohistology, granulation tissue is formed. It becomes structured over time, having layer-by-layer differentiation and a tendency to form collagen bundles with the subsequent formation of fibrous tissue, more dense and suitable for integumentary function.[15]
Wound healing takes place in one of three ways: primary or secondary intention, or under the scab.[19]
Primary intention is the most favorable method of healing. However, it requires initial favorable conditions: a wound with minimal microbial contamination, tightly adjacent wound edges, and the absence of necrotic tissue.
Secondary intention is a wound healing option that is the opposite of the intention described above. This type of healing is common in infected wounds.[20]
Healing under a scab is healing characteristic of wounds with a large area but shallow depth. In this case, a process similar to healing by primary intention occurs, but oriented in the longitudinal plane. In addition, the wound surface is covered with a scab - a layer of dried blood, tissue fluid and detritus.[21] The scab serves as a biological dressing until the wound heals and epithelializes.
Complications of wounds
- home
- Diseases and treatment
- Complications of wounds
Wounds can be accompanied by a variety of complications, both immediately after the wounds are inflicted and in the long term. These include:
- Gray - accumulation of exudate in the residual cavity of the wound. Its infection leads to suppuration of the wound. Requires timely evacuation.
- Wound hematoma - formed due to incomplete stopping of bleeding. Serves as a potential source of infection. A tense hematoma compresses the surrounding tissues and leads to ischemia. The hematoma must be removed by puncture or revision of the wound.
- Necrosis of surrounding tissues - develops when the blood supply to the corresponding area is disrupted due to tissue trauma during surgery or improper suturing. Wet skin necrosis must be excised due to the risk of deep accumulations of pus. Superficial dry necroses of the skin are not removed, as they perform a protective function.
- their development is facilitated by a high level of contamination (contamination of the wound) and high virulence (aggressiveness) of the microflora that has entered the wound, the presence of foreign bodies in the wound, necrosis, accumulations of fluid or blood, chronic impairment of local blood supply, general factors influencing the course of the wound process, and also late surgical treatment. It is the patient’s refusal to seek specialized help in a timely manner that can lead to serious complications.
Suppuration with subsequent development of abscesses, phlegmon
Most often, the development of pyogenic (pyogenic) wound infection occurs on the 3-5th day after injury, less often - at a later date - on the 13-15th day. Anaerobic infection can develop very quickly; in fulminant forms, it appears within a few hours after injury. The first symptoms are thickening, redness and pain. Increasing pain in the wound area is an early, but, unfortunately, often ignored sign of the development of infection.
Adequate surgical treatment is necessary: the wound is opened, the pus is removed, thoroughly washed, after which, if indicated, it is drained with tubular drainage and tamponed with a material that has sorption properties. After cleansing the wound and the appearance of granulation tissue, secondary sutures are applied or the edges of the wound are tightened with an adhesive plaster.
- Dehiscence of the wound edges can occur in cases where the applied external forces exceed its strength. Most often, the divergence of the skin edges of the wound occurs during the first month after its suturing, precisely during that period of time when the sutures have already been removed and the formation of cross-links of collagen fibrils has not been completed. Even with normal metabolism, a postoperative scar in one month acquires only 35% of its original strength and never becomes stronger than the tissue it replaced. Dehiscence of the wound edges is eliminated surgically.
- Suppuration of postoperative wounds . Among all postoperative complications, surgical infection ranks first and accounts for 32-75%. After planned surgical interventions, infectious complications occur in 6.5% of cases, after emergency ones - in more than 12%
Manifestations of postoperative wound infection do not have specific symptoms relative to any other wound infection. Local symptoms include swelling and hyperemia (redness) or cyanosis (blueness) of the skin up to the development of necrosis, severe pain at rest and on palpation in the wound area, fluctuations in places of greatest accumulation of exudate, wound discharge, divergence of wound edges, slowdown of reparative processes in wound.
In patients weakened by severe surgery, concomitant pathology or trauma, these symptoms may be mild.
In case of total suppuration of the wound, the sutures are completely removed, the edges of the wound are separated, exudate or hematoma is evacuated, non-viable tissue is excised, pockets and leaks are opened. In most cases, in the early stages of the disease, these measures are enough to stop the purulent process. The wound is subsequently maintained openly. Dressings are carried out daily using iodophor solutions, water-soluble ointments or draining sorbents. After the signs of local inflammation have been relieved, secondary sutures are applied to the wound or the edges of the wound are closed with adhesive tape, which significantly reduces the treatment time.
- Malignization . Long-term chronic wounds can be complicated by malignancy (malignancy). The diagnosis is confirmed by a biopsy of wound tissue, which can be performed in our hospital. Further treatment tactics are determined individually, depending on the results of the histological examination.
Consultation on paid services Show phone numbers
Wound healing and factors influencing this process
The wound healing process can be disrupted by many factors.
Healing is the process of repairing damaged tissue and restoring its integrity. During the healing process, certain processes occur. We will not dwell on them in more detail, but will only indicate those factors that may disrupt the healing process:
- Age. As a rule, this applies more to older people. The child's body has great regenerative capabilities. This is due to the high level of anabolic (construction) processes in the body.
- Attachment of infection.
- Decreased immunity.
- Poor circulation in the wound area.
- Chronic diseases (diseases of the respiratory and cardiovascular systems, diabetes, tumors and others).
Healing complications
- Attachment of infection . Most often, a nonspecific purulent infection develops. The threat is tetanus, rabies, diphtheria. Therefore, injuries that have been bitten and contaminated with soil or old metal objects should be immediately examined by a surgeon with a number of preventive measures taken (administration of anti-tetanus serum, rabies vaccine).
- Bleeding.
- Divergence of defect edges.
- In some cases, healing may be complicated by a hypertrophic scar or keloid . They are an abnormal scar that can spread beyond the defect area and also contribute to the development of complications.
First aid for a child for superficial wounds
When such a situation arises, parents ask themselves: “How to treat the wound? How to properly treat a wound? What is the best remedy for treating a wound?
Before helping a child, parents need to wash their hands with soap and use an antiseptic. Next, in this sequence, you need to follow a number of instructions and actions:
- Assess the extent and nature of the damage. It is very important to understand whether the baby has a deep or superficial wound.
- Rinse and stop bleeding. Hydrogen peroxide is best suited for this purpose. You can also use a solution of furatsilin and chlorhexidine.
- Next, you can treat the skin with a drying antiseptic, for example, iodine solution or brilliant green.
- Apply an aseptic (clean) dressing.
- In the future, it is important to change the dressings regularly. It is also possible to use ointments and creams discussed earlier, which will speed up the healing process.
In case of deeper defects, heavy bleeding, wounds that have been bitten and contaminated with soil or old metal, you must urgently contact a surgeon.
Wounds are quite common, especially in young children. The task of parents is to provide timely assistance to the child in order to prevent infection. You must have a minimum first aid kit in your first aid kit. Do not self-medicate and, if threatening injuries occur, consult a doctor.
Products for treating wounds in children
Below we list the most popular and affordable means for treating superficial wounds in children:
- Iodine. Suitable for superficial abrasions, but not for deeper injuries.
- Diamond green.
- Hydrogen peroxide. It is the drug of choice for first aid in the treatment of superficial abrasions in children. Allows you to clean abrasions and scratches well. An equally important property is stopping bleeding.
- Furacilin. To prepare a solution for topical use, dissolve the tablet in water.
- Miramistin. It is also an antiseptic for topical use. Allows you to prevent suppuration. If a purulent process occurs, it allows you to fight it. A pleasant bonus will be the possibility of using this remedy for acute respiratory viral infections, sore throats and pharyngitis in children.
- Chlorhexidine.
An antiseptic helps prevent suppuration.
To speed up healing, ointments and creams can be used such as:
- Levomekol;
- Betadine;
- Vishnevsky ointment;
- cream Bepanten plus.
Main types of chronic wounds
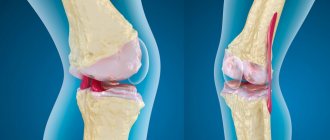
- Diabetic foot syndrome (DFS) is a set of anatomical and functional changes that develop against the background of diabetes mellitus, increasing the risk of injury and infection of the soft tissues of the foot. According to the World Health Organization, the risk of developing DDS in diabetics with 5-10 years of experience is about 15%. For diabetics with more than 15 years of experience, it increases to 90%.
- Prevention: protecting feet from injury, comprehensive foot and nail care, wearing shoes for diabetics.
- Trophic ulcers are complications of venous insufficiency caused by changes due to thrombophlebitis or deep vein varicose veins. Poor circulation and blood supply to the legs leads to venous congestion, and this leads to the formation of poorly healing ulcers on the ankles or legs.
- Symptoms are swelling, impaired skin pigmentation (redness or pallor), eczema, a feeling that the legs are bursting from pressure (more often in the evening).
- Prevention: timely treatment of the underlying disease, wearing elastic tights, treating the skin with antiseptic and healing agents.
Symptoms of non-healing wounds
•constant pain;
•converging edges of the wound;
•constant bleeding;
• “stuck” wound at one of the stages of healing for more than three weeks;
•often – unpleasant odor;
•conventional treatments do not help or help little.
These signs indicate that the regeneration processes in tissues are disrupted for one reason or another. For the treatment of chronic wounds, local treatment is not enough; comprehensive measures are required.
To achieve progress in healing, it is necessary to provide conditions for restoring the normal rate of regeneration. They largely depend on the cause of the chronic wound, but there are recommendations that are common to all situations.
The body needs to provide:
•balanced nutrition - in particular, the diet should be enriched with vitamins A and B, which stimulate tissue regeneration, and vitamin C, which promotes the production of collagen - a substance involved in the formation of connective tissue that closes the wound in the first stages;
•normal sleep mode – during sleep the regeneration process occurs more actively;
•protecting the wound and the area around it from external influences, such as rubbing, squeezing, etc.;
•wound ventilation – without air circulation, the wound will quickly fester.
More specific recommendations depend on the origin and nature of the wound.
Dressings for the treatment of non-healing wounds
When treating wounds of any nature, including chronic ones, the correct selection of dressing material plays an important role.
Dressing material for non-healing wounds should be:
•hygroscopic;
•"breathable";
•elastic and flexible – the bandage will have to be worn for a long time, so it should not interfere with movements.
Biotekfarm company offers a wide selection of dressings for the management of wounds of any complexity and at any stage. So, for wounds in which there are fragments of necrotic tissue or hemorrhage, a Parapran dressing with chymotrypsin is suitable - the drug included in the dressing helps to break down necrotic tissue, helping to cleanse the wound.
To moisturize “dry” chronic wounds (bedsores, trophic ulcers) and accelerate their healing, it is recommended to use the “GelePran” dressing with miramistin or colloidal silver. This soft transparent dressing, consisting of 70% water, moisturizes the surface of the wound, and the medicine it contains (miramistin or silver) disinfects and promotes regeneration.
For the treatment of infected wounds, bactericidal dressings Voskopran with Povidone-iodine ointment, antimicrobial dressings Voskopran with Dioxidin ointment, and anti-inflammatory dressings Voskopran with Levomekol ointment are suitable. Polipran dressings with Dioxidin are excellent for preventing infection of wounds at the granulation stage.
The Chitopran dressing based on chitosan nanofibers will help stimulate regeneration. It provides optimal conditions for healing - sufficient humidity, breathability and protection from damage, and promotes the rapid growth of its own cells. It is worth paying attention to the fact that this bandage does not need to be removed - it resorbs on its own as the wound heals.