Signs of the disease
The content of the article
The main signs of the disease and its symptoms:
- nausea and vomiting;
- heaviness in the stomach;
- belching;
- frequent heartburn;
- pain in the stomach;
- hunger;
- prolonged discomfort;
- diarrhea or constipation.
Most people become infected with this bacterium in the first years of their lives, it is transmitted through dirty hands, hygiene items, even by kissing, the bacteria Helicobacter pylori can be transferred. While this microorganism is inactive, it does not pose a particular threat to human health. But, as soon as some malfunctions appear in the body’s functioning, this bacterium begins to become active and causes a destructive effect, the stomach and duodenum are especially susceptible to its effects. Under its influence, gastritis and stomach ulcers develop. Erosion is formed, which causes pain and discomfort to a person.
2.1 how to treat
There is no clear answer to the treatment of Helicobacter pylori. Some are inclined to believe that it needs to be treated, others are against its complete elimination from the body. But, of course, self-prescribing medications is out of the question.
Treatment should be prescribed by a doctor, after a full medical examination, with all the necessary tests, and based on the complete picture, the doctor must make a decision on treatment. Basically, treatment involves the prescription of antibiotics, in combination with other drugs that will have a healing and restorative effect on the walls of the stomach. Diet is also a necessary condition for successful treatment; food should be light so as not to cause sudden changes in increase or decrease in acidity. At the end of treatment, a second full diagnosis is carried out to ensure the correctness of the treatment and its success.
Often, having discovered a bacterium, it is suggested that all family members be tested in order to exclude this bacterium from them. If a microorganism is nevertheless detected in family members, then they are all prescribed complex treatment, mainly with first-generation antibiotics. After 1-2 months, repeat tests are carried out, and based on their results, treatment is stopped or a second course is prescribed using stronger drugs.
2.2 Eradication therapy
The most effective treatment method is eradication therapy, which involves the use of several drugs simultaneously, with different effects. Of course, you can’t do without an antibiotic, but in addition to it, medications are prescribed that have an effect on the body’s digestive system, improve and speed it up, use enzymes to quickly break down food, thereby reducing the load on the digestive organs. There is less reflux of bile into the stomach to break down food, and due to this, the mucous membrane is less irritated. By prescribing drugs that have an enveloping effect, ulcers and erosions on the gastric mucosa are healed, pain and discomfort gradually go away. Naturally, it is necessary to properly restore and strengthen the body’s microflora through the use of probiotics and prebiotics. With their help, the patient's normal stool will be restored.
2.3 tests that must be taken to detect the bacteria:
- blood from a vein;
- breath test;
- stool analysis;
- saliva analysis;
- smear analysis for FGS;
In fact, it is not necessary to take the entire series of tests listed above. Basically, doctors prescribe blood from a vein, a breath test and a test for FGS.
A blood test will only show the presence of antibodies to bacteria of this type, and if its indicators are slightly deviated in one direction or another, then another analysis will have to be carried out to make sure.
The most reliable analysis is a smear, which is taken when examining the stomach from its walls, during fibrogastroscopy (FGS). Another similar method is to break off a piece of mucous membrane during endoscopy and examine it under a microscope for cytology. There can no longer be a mistake; the laboratory assistant sees a bacterium. There cannot be any deviations or errors, such as in a blood or stool test.
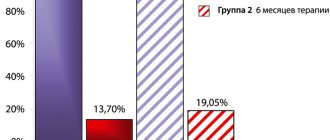
Peptic ulcer disease in the world of big numbers
According to various sources, from 10 to 15% of the world's population will experience this disease at some point in their lives. Both in Russia and throughout the world, peptic ulcer disease is considered the most common gastrointestinal pathology, and with age the likelihood of getting sick becomes higher. This is largely due to the fact that the risk of “catching” the culprit of all troubles - small, but very resistant in an acidic environment, Helicobacter pylori - only grows over the years. And if at the age of 20 the probability of infection is 20%, then with each subsequent decade it increases by exactly 10%. It turns out that by the beginning of their sixties, half of the planet’s inhabitants are already intimately familiar with H. pylori.
Every year more and more new cases of the disease are diagnosed. Doctors attribute this disappointing trend to the widespread use of non-steroidal anti-inflammatory drugs, which significantly increase the vulnerability of the stomach wall. However, the achievements of modern medicine make it possible to give a very favorable prognosis for peptic ulcer disease. But back at the end of the last century, everything was not so clear.
Table 1.
Eradication therapy regimens
| A drug | Dose | Frequency of application |
| 1st line eradication therapy (7–10 days) | ||
| IPP | standard dose | 2 times a day |
| clarithromycin | 500 mg | |
| amoxicillin | 1g | |
| 2nd line therapy (10–14 days) - if first line therapy is ineffective or intolerant | ||
| IPP | standard dose | 2 times a day |
| metronidazole or amoxicillin | 500 mg (amoxicillin - 1 g) | 3 times a day (amoxicillin 2 times a day) |
| tetracycline | 500 mg | 4 times a day |
| bismuth drug | 120 mg | |
Disadvantages of treatment for Helicobacter pylori:
- treatment is carried out by using antibiotics, often these are two types of antibiotics at once, which can have a negative effect on other organs;
- often, after taking a course of antibiotics and re-testing, the presence of the bacteria is confirmed, i.e. it has not died, and the doctor will again prescribe you eradication therapy, only now even more stringent;
- Even after complete treatment and a negative test result for this microorganism, there is no guarantee that in a week you will not catch this virus again, and so, start taking an antibiotic again.
4.1 in what cases is treatment prescribed:
- atrophic gastritis;
- the presence of ulcers and disease of the duodenum;
- stomach cancer.
Antibacterial drugs
Macmiror destroys the parasite's genetic material.
The choice of antibacterial drugs that can cope with Helicobacter is small. This is "Trichopol" or "Metronidazole", or "Makmiror".
Trichopolum and Metronidazole are complete analogues. The main active ingredient of the drug, metronidazole, penetrates the microorganism and breaks down, releasing toxic substances.
They destroy the parasite's genetic material. The main active ingredient of Macmiror is nifuratel. It simultaneously inhibits the growth of bacteria and prevents the proliferation of microorganisms.
The peculiarity of this drug is that nifuratel does not reduce the patient’s overall immunity, but, on the contrary, improves the body’s defenses. Macmiror is a second-line drug. It is prescribed if treatment with metronidazole does not give the expected result. This medicine is used in the treatment of peptic ulcers in children.
Which doctor treats heliobacteriosis?
If pain and other negative symptoms appear in the stomach, as well as when diagnosing bacteria, you should consult a gastroenterologist. If similar problems appear in children, you should consult a pediatric gastroenterologist. In the absence of these specialists, you need to contact a therapist, or when treating children, a pediatrician.
Author of the article:
Danilova Tatyana Vyacheslavovna |
Infectious disease specialist Education: in 2008, received a diploma in the specialty “General Medicine (Therapeutic and Preventive Care)” at the Russian Research Medical University named after N. I. Pirogov. I immediately completed an internship and received a diploma as a therapist. Our authors
Extragastroduodenal diseases and conditions with an established pathogenetic role of infection.
- Iron deficiency anemia of unspecified etiology;
- Idiopathic thromocytopenic purpura;
- Vitamin B12 deficiency.
According to the provisions of the fifth Maastricht consensus, these patients are indicated for diagnosis and treatment of H. Pylori infection. Other extragastroduodenal diseases and conditions in which the pathogenetic role of the infection is being investigated. H. pylori has positive and negative associations with a large number of other extragastroduodenal conditions/diseases.
The etiology of these relationships has not been proven.
H. pylori infection and the cytotoxin-associated gene product CagA(+) of H. Pylori strains are associated with the development of atherosclerosis. A relationship has been identified between H. pylori and some neurological diseases (stroke, Alzheimer's disease, Parkinson's disease). However, these data are insufficient to establish a clear cause-and-effect relationship or relationship with treatment. In a number of populations, an inverse relationship has been found between the frequency of H. pylori infection and the prevalence of certain diseases, such as bronchial asthma and obesity.
Also of considerable interest are the data that revealed that the correlation between H. Pylori seropositivity and preeclampsia was very significant with an odds ratio = 9.22. This association was even more pronounced during pregnancy with both preeclampsia and fetal growth restriction (OR=35.56). At the same time, the highest risk was determined by H. Pylori CagA(+) strains (Cardoropoli S. et al., 2011). Moreover, another study showed that antibodies against CagA can cross-react with the bate-actin of cytotrophoblast cells, hypothetically explaining the above-described clinical association (Franceschi F. Et al., 2012).
Diagnosis of H. Pylori infection
Methods for diagnosing infection can be divided into invasive and non-invasive.
Invasive techniques:
- histological method;
- helpil test (rapid urease analysis);
- bacteriological method;
- cytological method - examination of smears;
- molecular genetic method (PCR in material taken from a biopsy).
Non-invasive techniques:
- serological method - blood testing for antibodies to a microorganism;
- enzyme immunoassay of feces (for the presence of a specific antigen);
- polymerase chain reaction for analysis of nucleotide sequences of microbes in feces;
- urease breath test with 13.14C-urea;
- ammonia breath test (helic test).
A common disadvantage of all invasive techniques is the need for endoscopic examination, which is not indicated in all cases, and sometimes is even contraindicated. The histological and cytological methods have absolute specificity (no false positive result), but not the highest sensitivity (probability of a true negative result), since the microbe may not be present in the biological material being studied. The results of bacteriological research (culture on a nutrient medium) also have high specificity and make it possible to check the sensitivity of a microorganism to antibiotics, however, the sensitivity of this method is even lower, since the microorganism requires special conditions for collecting transportation, the presence of nutrient media and specially trained personnel, which makes this method very expensive.
The most widely used in our country is the rapid urease helpil test, carried out during an endoscopic examination. According to the provisions of the Maastricht Agreement V on the diagnosis of H. Pylori infection, it must be performed during endoscopy and there are no contraindications to biopsy. In the case of a positive test, to clarify the nature of the mucosal lesion, it is necessary to take a biopsy from the antrum and body of the stomach, which is extremely rarely performed in our practical medicine. At the same time, the helpy test performed during endoscopic examination is not recommended for monitoring after treatment, since in these cases it is not informative (has low specificity and sensitivity. The serological method is based on the detection of antibodies to the microorganism in the blood, and has a sufficiently high sensitivity for primary diagnosis However, it is not suitable for monitoring the effectiveness of treatment, since a high level of antibodies can remain for a long period after treatment. In addition, the information content of the method depends on the presence of a particular antigen in the structure of the microorganism, which may not be found in all strains.
In practice, we often encounter patients whose infection was diagnosed incorrectly due to specialists’ ignorance of the applicability of the methods, which gives rise to the false opinion that it is impossible to cure the infection not only among ordinary people, but also among practitioners.
Serological testing of stool for antigen to H. Pylori is highly informative, but depends on the type of microorganism circulating in the region; the polymerase chain reaction method for identifying the nucleotide sequences of the microorganism has demonstrated many false-positive results in a number of observations and is currently not recommended for use.
The rapid urease helix test, which is widespread in our country, is based on recording an increase in the concentration of ammonia in exhaled air in the presence of urease activity of Helicobacter; however, for a number of reasons, in a number of randomized clinical trials it has demonstrated insufficient sensitivity and specificity (probability of true positive and true negative result) and is not currently recommended for diagnosing infection.
According to the first provision of the international recommendations for the diagnosis of H. Pylori (Maastricht V), the 13,14C-urease breath test is the most studied and recommended non-invasive method in the “test and treat” strategy. And according to the 10th provision of the same agreement, this study is the best option for confirming the eradication (successful treatment) of H. Pylori. The technique is actively used in developed countries, but has not yet become widespread in Russia due to the lack of gas analyzers for assessing 13СО2.
The Clinic's doctors specialize in the diagnosis and treatment of H. Pylori - associated diseases, and the hospital's arsenal includes the most modern diagnostic techniques in accordance with international standards, including the 13C breath test. You can get advice on optimal diagnosis and treatment by making an appointment with a specialist. Taking a breath test is possible without first consulting a doctor and is indicated if relatives have H. Pylori-associated diseases or are suspected of having H. Pylori infection. If the test is positive, you will be able to receive treatment recommendations from your doctor.
It is based on the change in the concentration of 13CO2 in the patient’s exhaled air 30 minutes after taking 13C-Urea compared to the baseline concentration of 13CO2 (before taking the test solution). The non-radioactive and stable isotope 13C is used as a label. Carbamide (urea) labeled with this isotope decomposes in the human stomach exclusively under the action of urease, an enzyme that is a waste product of H. Pylori. 13CO2 enters the lungs through the bloodstream, from where it is evacuated with exhaled air. The concentration of 13CO2 directly depends on the number of Helicobacter pylori bacteria in the patient’s gastric epithelium.
Features of the 13C Urea test in the diagnosis of H. pylori infection.
- Lack of radioactivity, can be used by any person, including pregnant women and small children.
- It is a priority method for diagnosing HP in the most advanced and technologically developed countries.
- Highest accuracy, sensitivity and specificity, minimizing the possibility of obtaining false positive and false negative results.
- Non-invasiveness of the technique (no need for endoscopic examination).
- The test method is simple and fast, with a guaranteed test result within three minutes after the end of the testing procedure.
MALT lymphoma
MALT lymphoma is an extranodal marginal zone B-cell lymphoma associated with mucous membranes. It is a non-Hodgkin lymphoma, the substrate of which is sufficiently mature malignantly transformed lymphocytes originating from solitary lymphoid follicles of the mucous membranes.
Currently, H. Pylori is considered as the main causative agent of the disease, but the incidence in the world is low and amounts to 1 case per 30,000-80,000 infected individuals.
Diet for the treatment of Helicobacter pylori infection
Modern techniques allow you to be cured in a matter of weeks.
There is no specialized nutrition to combat Helicobacter. During treatment, you should adhere to the diet recommended for patients with gastritis, ulcers and other diseases of the stomach and intestines.
Food should be light, pureed and not irritate the mucous membranes. Heavy, spicy, fried and fatty foods are prohibited.
An ulcer is a dangerous disease. The cause of this pathology has now been identified. Helicobacter pylori should be treated under the guidance of a gastroenterologist. Modern techniques make it possible to get rid of this microorganism in a matter of weeks.
Main stages in the study of H. Pylori infection
- 1906, U. Krieiutz first described spiral-shaped bacteria in patients with gastric cancer;
- 1915, E. Rosenow, A. Sanford discovered similar bacteria in patients with ulcerative lesions of the stomach and duodenum;
- 1924, J. Luck, T. Seth demonstrated in their works the presence of urease activity in the human stomach and put forward a hypothesis about its connection with 12-gut ulcer;
- 1923, 1947, G. Konjetzny, based on morphological and clinical data, made an assumption about the inflammatory nature of peptic ulcer and stomach cancer;
- In the second half of the last century, many clinicians in a number of studies noted the positive effect of antibacterial therapy on the healing of peptic ulcers.
- 1984 The Lancet published the results of a study on isolated spiral-shaped bacteria, mainly from the antrum of the stomach and from the area of gastric metaplasia of the duodenal epithelium (Marshall BJ, Warren JR), and subsequently in 2001 they received the Nobel Prize for achievements in the field of medicine for this discovery and physiology.
- 1985 Marshall B, according to Koch's postulates, self-infected himself as part of an experiment to confirm the infectious nature of chronic gastritis.
- 1985-1994, major studies were carried out that established H. Pylori infection as the most important etiopathogenetic factor of chronic gastritis (type B), duodenitis (gastroduodenitis), gastric ulcer and 12-gut ulcer, MALT lymphoma (mucosal-accociated lymphoid tissue) and adenocacinomas of the stomach;
- 1994, experts from the WHO International Agency for Research on Cancer classified H. Pylori as a class 1 carcinogen;
- 1994, the US National Institutes of Health first adopted guidelines for the treatment of H. Pylori-associated peptic ulcer disease;
- 1996-2015, 1-5 Maastricht consensus on the diagnosis and treatment of H. Pylori-associated diseases;
- 2014 Kyoto Consensus, the main provision of which was not only the recognition of H. Pylori-associated gastritis as an infectious disease, but also recommendations for the treatment of all persons infected with this microorganism.
Author of the article: Tryapitsyn Alexander Valerievich (gastroenterologist, candidate of medical sciences)