Spascuprel is an antispasmodic drug that helps with pain of various etiologies. It quickly relieves spasms and pain, alleviating the condition. It is presented as odorless tablets that are placed under the tongue when taken.
The homeopathic medicine Spascuprell is designed to effectively treat convulsive spasms and relieve acute pain. Source: flickr (Eugene Evehealth).
Compound
| Homeopathic sublingual tablets | 1 table |
| active substances: | |
| Citrullus colocynthis (citrullus colocyntis) D4 | 30 mg |
| Ammonium bromatum (ammonium bromatum) D4 | 30 mg |
| Atropinum sulfuricum (atropinum sulfuricum) D6 | 30 mg |
| Veratrum album D6 | 30 mg |
| Magnesium phosphoricum (magnesium phosphoricum) D6 | 30 mg |
| Gelsemium sempervirens (Gelsemium sempervirens) D6 | 30 mg |
| Passiflora incarnata (Passiflora incarnata) D2 | 15 mg |
| Agaricus muscarius (Agaricus muscarius) D4 | 15 mg |
| Chamomilla recutita (Chamomilla recutita) D3 | 15 mg |
| Cuprum sulfuricum (cuprum sulfuricum) D6 | 15 mg |
| Aconitum napellus (aconitum napellus) D6 | 60 mg |
| excipients: magnesium stearate - 1.5 mg; lactose - to obtain a tablet weighing about 302 mg |
Dosage and interactions
Apply the product three times a day under the tongue. Take before or after meals according to the instructions.
If there is a sharp exacerbation of the pain syndrome, then the tablets are taken every quarter of an hour, but no longer than two hours in a row (that is, up to eight times). The course lasts 3 weeks, but the period can be extended as prescribed by a doctor.
The study of Spascuprel did not reveal any problems caused by overdose. At the same time, doctors do not recommend deviating from the prescribed intake standards.
The medicine is considered safe for use by different age groups.
When prescribing it, the use of other medications is not excluded.
The drug is sold in pharmacies over the counter in packs of fifty pieces.
Shelf life is approximately 5 years.
special instructions
When taking homeopathic medicines, existing symptoms may temporarily worsen (primary deterioration). In this case, you should stop taking the drug and consult your doctor. If side effects occur that are not described in the instructions for medical use, you should inform your doctor.
The drug contains lactose, and therefore it is not recommended for patients with congenital galactosemia, glucose or galactose malabsorption syndrome, or congenital lactose intolerance.
Instructions for patients suffering from diabetes: 1 table. contains 0.025 XE.
Indications for use of Spaskuprel
- Pain syndrome of a spastic nature, which includes spasms of the urinary system, gall bladder and gastrointestinal tract.
- Muscle tension or stiffness.
- Relieving spasms.
The majority of patients taking Spascuprel noted a noticeable relief of their condition, relief from spasms for a long period of time.
In practice, homeopathic Spascuprel tablets are successfully used even in the treatment of toothache in infants. Source: flickr (dadew23)
Spascuprell was also used for algodismenorrhea (that is, painful periods), migraines, chronic obstructive pulmonary disease, laryngeal spasms, and gastrointestinal ulcers.
Important: doctors recommend using the drug only according to the instructions, since the effect of certain components on the body if used incorrectly can give undesirable results.
Analogs
Level 4 ATC code matches: Cystamine
Neovasculgen
Lymphomyosot
Galium-Hel
Ammonia
Mucosa Compositum
Coenzyme Compositum
Ubiquinone Compositum
Dimephosphone
Oscillococcinum
Dantinorm Baby
Coryzalia
Longidaza
Homeovox
Generics similar in chemical composition have not been found.
Best before date
60 months
Vitamins with similar effects
- Golden mustache. V. Ogarkov's drops No. 5 (Drops for oral administration)
- Yogi-T Stomakh Easy (Herbal tea)
- Cardianev (Capsule)
- Marcalact (Oral powder)
- Norma-SHPA (Capsule)
- Spascuprel (Suppositories)
- Golden mustache. V. Ogarkov's drops No. 2 (Drops for oral administration)
- Viburkol (Rectal suppositories)
- Reishi (Capsule)
- Carminative collection (Medicinal collection)
The description of vitamin Spascuprel is intended for informational purposes only. Before starting to use any drug, it is recommended to consult a doctor and read the instructions for use. For more complete information, please refer to the manufacturer's instructions. Do not self-medicate; EUROLAB is not responsible for the consequences caused by the use of information posted on the portal. Any information on the project does not replace consultation with a specialist and cannot be a guarantee of the positive effect of the drug you use. The opinions of EUROLAB portal users may not coincide with the opinions of the site Administration.
Are you interested in Vitamin Spascuprel? Do you want to know more detailed information or do you need a doctor's examination? Or do you need an inspection? You can make an appointment with a doctor - the Euro lab is always at your service! The best doctors will examine you, advise you, provide the necessary assistance and make a diagnosis. You can also call a doctor at home . Euro lab clinic is open for you around the clock.
Attention! The information presented in the vitamins and dietary supplements section is intended for informational purposes and should not be a basis for self-medication. Some of the drugs have a number of contraindications. Patients need to consult a specialist!
If you are interested in any other vitamins, vitamin-mineral complexes or dietary supplements, their descriptions and instructions for use, their analogues, information about the composition and form of release, indications for use and side effects, methods of use, dosages and contraindications, notes about the prescription of the drug for children, newborns and pregnant women, price and consumer reviews, or you have any other questions and suggestions - write to us, we will definitely try to help you.
Chronic daily headache (CDH) is a heterogeneous group of diseases characterized by cephalgia that occurs at least 6 times a week, lasts at least 4 hours a day and is observed at least 15 days a month and at least 6 months a year [2, 4 ]. The most common forms of CHH include chronic tension-type headache (CTH) and chronic headaches due to arterial hypertension (CHTH).
In turn, CGTH includes a headache, in which painful tension in the muscles of the face, scalp, and back of the neck is detected by palpation, i.e. CHF with and without pericranial muscle dysfunction (CHD). The latter is classified as psychogenic headache (CHBP).
CHBAH meet the main criteria for diagnosing this type of cephalalgia, but differ when measuring blood pressure (BP) by a predominant increase in its diastolic level. At the same time, headaches occur not only with significant hypertension, but also during the period when blood pressure levels do not exceed normal background values, i.e. “workers”, numbers [5]. This is apparently explained by a decrease in the pain threshold of the receptor territories of the vessels and membranes of the posterior cranial fossa, in which pulse fluctuations are perceived as painful with subsequent projection of pain in the occipital region. The secondary disturbances of venous blood flow that arise in this case may indirectly contribute to the contraction of the pericranial muscles, which in their final manifestation is close to CGNDDM. Thus, it cannot be completely excluded that in both main forms of CEHD, the final substrate on which vascular and psychogenic causes converge is the pericranial muscles.
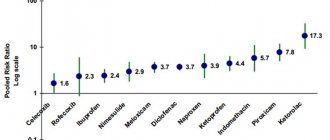
Patients with CEHD daily resort to various analgesics, tranquilizers, muscle relaxants, and antihypertensive drugs, which have many side effects. Thus, tranquilizers reduce concentration; muscle relaxants cause general muscle weakness and cannot be used by vehicle drivers; the use of antihypertensive drugs at “working” blood pressure levels is often not justified. Therefore, the search for drugs with minimal side effects (or without them) for the treatment of CEHD continues to be relevant.
Since common mechanisms of craniocephalgic syndrome are not excluded in patients with CGNDMA and CGBA, it was assumed that the use of a combination of antihomotoxic drugs Spascuprel and Spigelon could have a positive medicinal effect on such patients without leading to undesirable side effects. It seemed to us appropriate to conduct a clinical study of the combined use of these drugs for two reasons: firstly, the practically non-repetitive composition of these drugs (with the exception of the Gelsemium component) when taken simultaneously in practical terms, undoubtedly expands the therapeutic possibilities for relieving various cephalgic syndromes origin, and secondly, by adding Spascuprel to the drug Spigelon, which is basic for these purposes, we deliberately strengthened the antispasmodic component of the drug effect, which cannot be neglected in the complex treatment of CEHD.
Therefore, the purpose of this study was to identify the clinical-physiological and clinical-psychological effects of the drugs Spascuprel and Spigelon when used in combination by patients with CEHD.
At the same time, the following tasks were solved during the study: to assess the clinical and psychological state of patients suffering from CEHD and the dynamics of their cephalgic syndrome during the study period; to determine sensory and pain thresholds in the studied group of patients before and after 4-fold sequential administration of the drugs Spigelon and Spascuprel for 120 minutes; determine the aftereffect time of these drugs.
Material and methods
The study included 19 patients with CEHD (15 women and 4 men) aged from 32 to 73 years (average age - 47.8 years). The diagnosis of CHBDM and CHPAH was made based on the diagnostic criteria of the Classification of Chronic Pain recommended by the International Association for the Study of Pain [4]. The study results were analyzed in total for the entire population of patients (n=19).
At the same time, it should be noted that in the studied group of patients, 13 (68.4%) people were diagnosed with CHBAH. The most common clinical diagnosis was hypertension with predominant damage to the vessels of the heart and brain; cephalgic syndrome. In 6 (31.6%) patients, CHBD was diagnosed with the most common clinical diagnosis being “craniocephalgic syndrome, vestibulopathy due to osteochondrosis of the cervical spine.”
The control group consisted of 8 people (2 men and 6 women, average age - 53.3 years) without complaints of pain of any localization.
A characteristic feature of CHBAH was dull, medium-intensity headaches in the parieto-occipital region, which varied in intensity throughout the day, usually under the influence of emotional factors. At the same time, blood pressure did not exceed the usual “working” values acceptable for this category of patients.
In case of CHBNDM, the cranialgic syndrome usually involved the frontal, orbital, fronto-occipital areas of the head (or combinations thereof) and in all cases was accompanied by unpleasant sensations in the back of the neck. Such aching, aching, pressing pain of moderate intensity intensified or weakened under the influence of both emotional and physical stimuli [5].
Subjective characteristics of patients in the study group with pain in the head (according to Pain Dictionary-2) [3] are presented in Fig. 1.
The research methods included in-depth clinical, neurological and psychological examinations, which included assessment of pain sensations using a visual analog scale (VAS), a pain questionnaire [3], thermodolometry (TDM) [1], which involved dosed temperature effects on the skin in the interval between 2nd–3rd metacarpal bones on both sides, with registration of sensory (SP) and pain (BP) thresholds before (SP-1, BP-1) and after (SP-2, BP-2) the use of the studied drugs. The drugs Spigelon and Spascuprel were prescribed as an initiating therapy sublingually, sequentially, after 15 minutes, for 120 minutes (Fig. 2). The results of the study were subjected to statistical processing using paired Student's t-test and correlation analysis.
Research results
Before taking the drugs Spigelon and Spascuprel, the patients’ sensory threshold (SP-1) on the right and left was 47.2˚C, while after finishing taking a complex of two antihomotoxic drugs, the TDM indicators significantly increased and amounted to 48.2 on the right and 48.3 on the left ˚С (see table). Before using the drugs Spigelon and Spascuprel, the pain threshold (BP-1) on the right and left was the same and equal to 52.9˚C, while after 120 minutes, during which the initiating therapy was carried out, BP-2 increased on the right to 54.9˚C , and on the left up to 54.6˚С (in both cases p=0.0001). Moreover, the VAS scores before the study were 67.9 and after – 46.6 cm (p = 0.0001). Consequently, in comparison with the results of the background examination, 2 hours after the start of the use of complex drugs, an increase in the sensory threshold by 1.1˚С and a pain threshold by 1.7–2.0˚С was registered, which was accompanied by a decrease in pain on the VAS scale by 32.8%.
As a result of the correlation analysis, a significant negative correlation was established between the background level of pain threshold (BP-1) on the right and the magnitude of pain on the VAS scale before treatment (r=-0.46, p=0.046). After the therapy, this correlation disappeared. Of course, this fact, taking into account the general dynamics of the above-mentioned indicators after a course of treatment, is an objective confirmation of the analgesic effectiveness of the antihomotoxic drugs tested in the study and at the same time does not exclude differences in the final results of therapy, which largely depend on the level of the individual pain threshold in an individual patient . In Fig. Figure 3 graphically shows the dynamics of pain in patients after a course of combined use of the drugs Spigelon and Spascuprel. As can be seen from the presented graph, only in 3 (15.8%) cases out of 19, according to repeated VAS, ineffectiveness of the therapy was recorded.
Only in 1 of these clinical observations were the highest rates of BP on the right side established during background and repeat examinations without any dynamics (BP-1=BP-2=65˚С). And in 2 other patients, despite a favorable increase in BP-2, in one case the maximum level of pain was recorded on the VAS scale (VAS-1=VAS-2=100 cm), in the other a slight increase in this indicator was determined (by 4. 4%).
In most cases of successful relief of cephalgic syndrome, a regression of subjective pain on the VAS scale was determined by more than 30% (in 75% of patients with favorable dynamics of this indicator).
The level of the sensory threshold, on the contrary, was not “related” to the VAS examination data either before or after treatment. At the same time, a significant negative correlation was established between the SP on the right and the number of descriptor words according to the Pain Dictionary-1. Moreover, the reliability of this relationship was further enhanced after re-examination at the end of a 2-hour treatment with antihomotoxic drugs (r = -0.46; p = 0.053 and r = -0.53; p = 0.009, respectively). The number of selected descriptor words averaged 11.6±0.84 for the examined patients (with a range of indicators in the study sample from 7 to 21), which to a certain extent testifies in favor of the hypothesis of a significant psychogenic component of this type of cephalgia.
Taking into account the identified reliable patterns between the background examination according to the Dictionary of Pain-1 and the measurement data of the sensory threshold during a clinical experiment, it is necessary to emphasize the high significance of the “verbal portrait of pain” not only as a diagnostic test (for example, when there are no others in the arsenal, including .ch. and objective methods for studying the nature of the pain syndrome), but also as a prognostic test that allows us to predict the final result of a particular pain therapy. The last reasoning, of course, requires further scientific confirmation. Nevertheless, the fact that we established a correlation, close to a significant one, between the number of descriptor words according to the Pain Dictionary-1 and the level of BP-2 in patients with cephalgic syndrome (r = - 0.45; p = 0.064) allows us to make such an assumption.
The duration of the analgesic effect of the Spigelon–Spaskuprel complex in most cases reached 18 hours, and the peak therapeutic activity was 6 hours. In this aspect, it is important to note that during a re-examination carried out immediately after the end of the initiating therapy (i.e., after 2 hours of drug treatment), 42.1% of patients stated, when characterizing the dynamics of the pain syndrome, that “a moderate headache remained,” even 26.2% - that “the headache went away partially”, in 2 (10.5%) cases, patients o, and in 1 (5.3%) - “the headache remained the same, but became more localized.”
That is, in 84.1% of cases, patients indicated one or another positive dynamics during the course of the cephalgic syndrome. Only 4 (25% of the number of people who had a positive effect from the combined use of the proposed drugs) patients reported that the headache attack resumed 12–24 hours after stopping therapy.
An examination of patients in the control group showed that SP-1 on the right was 42.0±1.16˚С, on the left – 43.7±2.73˚С, while BP-1 was 46.3±1.2˚С on the right and 47 .0±1.0˚С on the left. After taking the complex of study drugs, these indicators of SP measurements on both sides remained the same and only a slight (unsignificant) change was noted in the levels of BP-2: on the right it was 47.0±1.0˚С, and on the left – 49.0±1 .54˚С.
conclusions
The use of the Spascuprel-Spigelon complex in the initiating therapy mode for 120 minutes significantly reduces the severity of cephalgic syndrome in the two main forms of CEHD - CHBNDM and in chronic headache with a compensated version of arterial hypertension. This is confirmed by both psychological methods (VAS) and TDM data.
No reliable indicators indicating changes in sensory and pain thresholds under the influence of taking antihomotoxic drugs were obtained from individuals without pain syndrome.