Multiple organ failure syndrome develops as a result of simultaneous or sequential dysfunction of several organs. In most cases, multiple organ failure is the terminal stage of serious diseases, including the last stages of cancer. The term was introduced relatively recently - in 1973 and for more than 45 years it continues to be one of the most common causes of death among patients in intensive care units.
- Features of multiple organ failure
- How does multiple organ failure syndrome manifest?
- Why does multiple organ failure develop?
- Methods for diagnosing the disease
- Treatment of multiple organ failure in Euroonco clinics
- Nutrition for multiple organ failure
- Why is multiple organ failure dangerous?
Features of multiple organ failure
Pathological changes in an organ or organ system do not develop simultaneously. This process occurs in three main stages:
- Compensation. Lasts from three to five days. In response to damage, the body tries to compensate for the lost function. At the initial stages, he manages to do this relatively simply, so a complete failure of the organ does not occur. If treatment is carried out at this stage, it will be possible to avoid serious consequences that are characteristic of other stages.
- Subcompensation. During this period, the body cannot fully replenish the lost function, so the patient needs drug treatment. In order to correct existing disorders, small doses of medications are sufficient.
- Decompensation. This stage is characterized by pronounced changes in organs and complete loss of performance. The patient's condition becomes extremely serious. He needs large dosages of medications and additional measures that are designed to maintain life support (ventilation, hemodialysis).
The severity of multiple organ failure is determined based on the volume of the lesion. Decompensation of two systems corresponds to a severe degree, and of three - to an extremely severe degree.
How does multiple organ failure syndrome manifest?
The exact set of symptoms depends on the damage to certain organs. As a rule, the most distinct signs are signs of dysfunction of the respiratory system. This may be evidenced by the following clinical manifestations:
- Dyspnea.
- Activation of accessory muscles during breathing.
- Cyanosis of the skin.
- Severe sweating.
- Impaired consciousness and lethargy in the later stages.
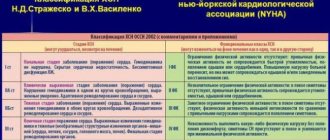
When the cardiovascular system is damaged, chest pain, various hemodynamic disorders, swelling of soft tissues and internal organs are noted. At the initial stage, there is pronounced tachycardia, up to 180 beats per minute. It develops to compensate for disturbances and is eventually replaced by bradycardia, in which the heart rate can drop to 40 beats per minute or even lower. In the later stages, the patient responds poorly to drugs that help normalize the activity of the cardiovascular system. This is one of the reasons why treatment of multiple organ dysfunction becomes difficult.
Disruption of the gastrointestinal tract in multiple organ failure is manifested by symptoms of mechanical compression of the intestine. These symptoms include:
- Violation of the process of defecation.
- Gas retention.
- Bloating and asymmetry of the abdomen.
- Vomit.
- Loss of appetite.
In some cases, gastrointestinal bleeding develops, which aggravates the course of the underlying disease and often causes the death of the patient.
Quite often the clinical picture contains signs that are characteristic of renal failure. First of all, this is a pronounced decrease in urine volume with the subsequent development of anuria, which is an indication for hemodialysis. In addition, patients exhibit a decrease in potassium levels in the blood, renal edema, water and electrolyte imbalance, etc.
Symptoms
The signs and their progress that appear in multiple organ failure are caused by a combination of disorders in the cardiovascular and respiratory systems, as well as dysfunction in the kidneys and liver. They are usually divided into several key conditions:
- functional disorders of the central nervous system;
- respiratory distress syndrome;
- acute liver and kidney failure;
- disseminated intravascular coagulation syndrome (DIC syndrome).
Also, medical specialists have identified four forms of the disease: obvious, hidden (latent), decompensated and terminal. In its obvious form, the toxic syndrome increases. It is accompanied by the progression of blood flow disorders in the liver, kidneys, and skin. The terminal form is characterized by the development of circulatory blockade and ischemia. Metabolites accumulate in human blood, which have a toxic effect on the body and disrupt the excretory function of the liver, kidneys and gastrointestinal tract.
A violation of the biochemical processes of detoxification in the liver is indicated by the presence of ammonia in the blood, and renal failure is indicated by the presence of medium-weight peptides. As for the respiratory system, respiratory distress syndrome develops. The lungs swell, breathing is impaired, and the body does not receive the required amount of oxygen. The patient experiences shortness of breath and an increased heart rate. Symptoms of cyanosis are detected: spots, pallor or blue discoloration of the skin. Extremities become cool.
As for the kidneys, with multiple organ failure syndrome, the risk of oliguria increases, a pathological condition when urine is retained in the body. Parents or caregivers may notice this in a child if he rarely urinates. Since this symptom does not appear only in MODS, it is impossible to make a diagnosis based on this alone. If kidney function is impaired, the content of epithelium, leukocytes and protein in the urine exceeds the norm. Red blood cells may also be detected. As oliguria progresses, anuria occurs, a disease in which urine does not enter the bladder and, as a result, is not excreted from it.
When the liver is damaged against the background of multiple organ failure, cholestatic jaundice develops. Manifestations include: skin itching, which gradually increases, yellowing of the sclera, increased cholesterol and bile acids in the blood, increased bilirubin concentration, decreased number of bilirubin metabolites in feces and urine.
Often, with multiple organ failure, disseminated intravascular coagulation syndrome appears - a disorder of hemostasis caused by deficiency and hyperstimulation of the reserves of the blood coagulation system. It provokes hemorrhagic, microcirculatory and thrombotic disorders. In DIC syndrome, organ dysfunction, bruising in the subcutaneous fat, subcutaneous hematomas, and petechial-hematomal rashes are observed. In acute cases, hypotension, shock, severe bleeding, etc. may develop.
One of the manifestations of MOF in adults and children is increasing acute heart failure. The heart muscle loses its elasticity and ability to contract. As a result, pumping blood becomes much more difficult, leading to stagnation. Progressive AHF may result in pulmonary edema or an asthma attack. Both conditions are extremely life-threatening.
In right ventricular heart failure, the liver becomes enlarged. All tissues and organs are poorly supplied with oxygen, and edema forms. It becomes more difficult for the patient to breathe. From the central nervous system, MOF manifests itself as acute psychosis, lethargy, and sometimes coma.
A common sign of multiple organ failure is duodenal and gastric ulcers. The patient is bothered by pain in the upper abdomen, which gradually intensifies. Heartburn inevitably accompanies a peptic ulcer.
Why does multiple organ failure develop?
Among the reasons that lead to the development of multiple organ failure syndrome are severe diseases and conditions that have a significant impact on the functions of the body. These include severe injuries, sepsis, infectious-toxic shock, etc.
In cancer patients, multiple organ failure syndrome develops after radical tumor removal. A distinctive feature of surgical interventions in oncology is the need to remove part of one or more organs that are affected by the tumor process. Moreover, such operations are often accompanied by massive blood loss, which increases the likelihood of developing the syndrome.
Multiple organ failure develops gradually. There are three main stages in its course:
- Production of various active molecules that lead to the development of a systemic inflammatory response. Such molecules can be interleukins, platelet activation factor, tumor necrosis factor, hormones, enzymes, free radicals, etc. As a result, vascular permeability and tone are disrupted, immune defense mechanisms and the most important biochemical processes are changed. All these changes correspond to the induction phase of multiple organ failure.
- During the cascade phase, the development of systemic damage is noted, which is manifested by characteristic symptoms - thrombocytopenia, leukocytosis, microcirculation disorders, hypoxia, etc.
- The phase of secondary autoaggression is characterized by severe organ dysfunction and disruption of homeostasis.
Multiple organ failure is characterized by several damaging mechanisms, among which the leading ones are ischemia, active thrombus formation and cerebrovascular accident.
Recommendations
- ^ a b c d f f gram h i j k
Irwin, Richard S.;
Rippe, James M. (2003). Irwin and Ripp Critical Care Medicine
.
Lippincott Williams and Wilkins. ISBN 978-0-7817-3548-3.[ page needed
] - Matsuda, Naoyuki; Hattori, Yuichi (2006). "Systemic inflammatory response syndrome (SIRS): molecular pathophysiology and gene therapy." Journal of Pharmacological Sciences
.
101
(3):189–198. Doi:10.1254/jphs.crj06010x. PMID 16823257. - Deitch, Edwin A. (June 1, 1989). "Simple intestinal obstruction causes bacterial translocation in humans." Archives of Surgery
.
124
(6):699–701. Doi:10.1001/archsurg.1989.01410060065013. PMID 2730322. - McIlroy, Daniel J.; Jarnicki, Andrew G.; Au, Gough G.; Lott, Natalie; Smith, Doug W.; Hansbro, Philip M.; Balog, Zsolt J. (December 2014). "Neutrophil extracellular traps of mitochondrial DNA are formed after injury and subsequent surgery." Journal of Intensive Care Medicine
.
29
(6): 1133.e1–1133.e5. doi:10.1016/j.jcrc.2014.07.013. PMID 25128442. - "MULTIPLE ORGAN FAILURE." ABC Australia
. August 7, 2014 - Watson, R. Scott; Crow, Sheri S.; Hartman, Mary E.; Lacroix, Jacques; Odetola, Folafoluwa O. (2017). "Epidemiology and outcomes of multiple organ dysfunction syndrome in children." Pediatric intensive care
.
18
(3 Suppl. 1): S4–S16. Doi:10.1097/PCC.0000000000001047. PMC 5334773. PMID 28248829. - van Wessem, Karlijn JP.; Linen, Luke P. (January 1, 2021). “Reducing mortality rates from post-traumatic multiple organ dysfunction syndrome: a paradigm shift? Prospective population-based cohort study." Shock: Trauma, Inflammation and Sepsis: Laboratory and Clinical Approaches
.
49
(1): 33–38. doi:10.1097/SHK.0000000000000938. PMID 28682941. S2CID 206062912. - Liu, Xiaoli; Hu, Pan; Mao, Zhi; Kuo, Po-Zhi; Li, Peiyao; Liu, Chao; Hu, Jie; Lee, Day; Cao, Desen; Mark, Roger J.; Cely, Leo Anthony; Zhang, Zhengbo; Zhou, Feihu (28 January 2021). "An interpretable machine learning model for early mortality prediction in elderly patients with multiple organ dysfunction syndrome (MODS): a multicenter retrospective study and cross-validation." arXiv:2001.10977. Magazine citation required | log = (help)
- van Brueghel, Johanna M. M.; Niemeyer, Menco J. S.; Houwert, Roderick M.; Groenwold, Rolf HH.; Leenen, Luke P. H.; van Wessem, Carlin JP (December 2021). “Global changes in mortality rates among polytrauma patients admitted to the intensive care unit—a systematic review.” World Journal of Emergency Surgery
.
15
(1):55. doi:10.1186/s13017-020-00330-3. PMC 7526208. PMID 32998744. - Sapan, Heber Bombang; Paturusi, Idrus; Yusuf, Irawan; Patellongi, Ilhamjaya; Massi, Mukh Nasram; Pusponegoro, Ariono Juned; Arif, Syafrie Kamsul; Labeda, Ibrahim; Islam, Andi Asadul; Randy, Leo; Hatta, Mohammad (1 June 2021). "The structure of cytokines (IL-6 and IL-10) as a mediator of inflammation and anti-inflammatory action in multiple organ dysfunction syndrome (MODS) in polytrauma." International Journal of Burns and Trauma
.
6
(2): 37–43. PMC 4913232. PMID 27335696. - Zeng, Lin; Du, Juan; Gu, Wei; Zhang, Anqiang; Wang, Hai-yan; Wen, Da-ling; Qiu, Lin; Yang, Xue-dao; Sun, Chien-hui; Zhang, Mao; Hao, Jiang; Jiang, Jian-xin (2015). "Rs1800625 in the receptor for advanced glycation end products gene predisposes to sepsis and multiple organ dysfunction syndrome in patients with major trauma." Critical care
.
19
(1): 6. doi:10.1186/s13054-014-0727-2. PMC 4310192. PMID 25572180.
Methods for diagnosing the disease
Symptoms of multiple organ failure may be similar to other diseases, so to confirm the diagnosis, the doctor prescribes a comprehensive examination, which includes the following diagnostic methods:
- Examination of the patient, analysis of complaints, collection of anamnesis. Already at this stage, a specialist can notice characteristic signs that indicate damage to one or more organs. These may be disturbances in respiratory and cardiac activity, metabolic changes, and deviations in hemodynamics.
- Instrumental examination. Its volume depends on the manifestations of multiple organ failure. The doctor has all non-invasive methods at his disposal, for example, ultrasound, X-ray, CT, MRI, etc. In addition, it is important to regularly monitor the body’s vital signs - blood pressure, heart rate, respiratory rate, etc.
- Laboratory diagnostic methods. Usually, basic tests are prescribed that allow one to evaluate and further monitor the main indicators of hemodynamics, the level of electrolytes and enzymes in the blood, etc.
Taking into account the fact that patients in most cases are in an intensive care unit, multiple organ failure can be detected in the early stages, when complete failure of the organ or system has not occurred.
Forecast
Mortality, although reduced to some extent, at least in developed countries with timely access to primary and tertiary care, varies where the chance of survival decreases as the number of organs involved increases. Mortality in MODS from septic shock (which itself has a high mortality rate of 25-50%) and from multiple traumas, especially if not treated promptly, is particularly severe. If more than one organ system is affected, the mortality rate is still higher, and this is especially true when five or more systems or organs are affected. Old age itself is a risk factor, and patients with weakened immune systems, such as those with cancer, AIDS, or a transplant, are at risk. The prognosis must take into account any underlying medical conditions the patient may have, their past and current health status, any genetic or environmental vulnerabilities they have, the nature and type of illness or injury (for example, COVID-19 data is still being analyzed while other cases caused by long-standing diseases are much better studied), as well as any resistance to drugs used to treat microbial infections or any coinfection acquired in the hospital. Earlier and more aggressive treatment, use of experimental treatments or at least modern tools such as ventilators, ECMO, dialysis, bypass and transplantation, especially in trauma centers, may improve outcomes in certain cases, but this depends in part on speed and accessibility. access to quality health care, which is lacking in many areas. Measurements of lactate, cytokines, albumin and other proteins, urea, blood oxygen and carbon dioxide levels, insulin and blood sugar, adequate hydration, continuous monitoring of vital signs, good communication within and between facilities and staff, and adequate staffing , education, and schedules are important in MODS, as with any serious illness.[6][7][8][9][10]
In patients with sepsis, septic shock, or multiple organ dysfunction syndrome caused by serious trauma, the rs1800625 polymorphism is a functional single nucleotide polymorphism, part of the receptor for advanced glycation end products (RAY) transmembrane receptor gene (of the immunoglobulin superfamily) and confers host susceptibility to sepsis and SPOD in these patients.[11]
Treatment of multiple organ failure in Euroonco clinics
Treatment of multiple organ failure should be comprehensive and carried out in an intensive care unit.
The main goal of patient treatment is to restore lost functions, eliminate the negative consequences of multiple organ failure and prevent complications. For this purpose, medications from the group of antibiotics, NSAIDs, hormones, anticoagulants, etc. are prescribed. If necessary, transfusions of blood or its components are performed, and prevention of disseminated intravascular coagulation syndrome, internal bleeding, and collapse is carried out. Throughout the treatment, the patient must maintain strict bed rest.
Multiple organ failure syndrome often requires replacement of the functions of vital organs that cannot cope with their work. For this purpose, artificial ventilation, renal replacement therapy, and various methods of maintaining cardiac function are used.
The leading cause of multiple organ failure is sepsis, an overreaction of the immune system to infectious agents, resulting in pockets of inflammation throughout the body. This condition often occurs in cancer patients. In this case, an important part of the treatment is antibacterial and infusion therapy. Euroonko clinics successfully use a modern technique - selective sorption on cartridges for extracorporeal hemoperfusion Toramyxin PMX-20R. With its help, the patient's blood is cleared of endotoxin in cases of infections caused by gram-negative and mixed flora.
In severe cases, surgical methods are used. These include extracorporeal detoxification, elimination of intestinal obstruction, and removal of non-viable organs that have begun to become necrotic.
The intensive care unit at the Euroonco clinic has all the necessary equipment for constant monitoring and maintenance of vital functions. We use equipment from leading brands; the rooms are equipped with a centralized oxygen supply system. All the necessary medications of the latest generations are always available. Our capabilities allow us to admit a patient on an emergency basis and immediately begin providing all necessary types of medical care.
Causes
Multiple organ failure can result from tissue hypoperfusion or hypermetabolism, various injuries and infections. As for cellular changes, the influence of mediators plays a major role in them. Their quantity during release depends on the severity of the factor provoking the damaging effect.
In some cases, the cause of multiple organ failure is a transfusion of canned blood that has been stored for a long time (especially in large quantities). Sometimes this condition is preceded by unskilled artificial ventilation. In the field of surgery, infectious complications are a key cause of the body's stress response. They cause disruption of the patient's homeostasis and metabolism system. In 7–22% of cases, multiple organ failure occurs in the postoperative period. In 50% of cases, the diagnosis is made due to purulent complications of acute inflammatory pathologies.
Multiple organ failure can result from impaired immunity and septic processes. In most situations, sepsis begins due to exposure to gram-negative bacteria that enter the organs and bloodstream through the gastrointestinal tract.
Nutrition for multiple organ failure
With multiple organ failure syndrome, the patient's body needs an increased amount of energy. Energy consumption increases 2–3 times compared to the norm. At the same time, the state of the digestive system does not allow the full absorption of nutrients. Therefore, feeding is carried out with special mixtures through a tube or intravenously. Gradually, as you recover, you are allowed to switch to normal food, initially in small portions.
Nutrition should be complete and balanced. The patient's body needs a sufficient amount of protein, vitamins, microelements, and antioxidants. In this case, mixtures with a low glycemic index are used to prevent the development of insulin resistance and diabetes mellitus.
Why is multiple organ failure dangerous?
The main danger of multiple organ failure is the high risk of death. Depending on the extent of the lesion, mortality can range from 30% to 100%. Even if the main manifestations of the syndrome can be eliminated in a timely manner, the likelihood of developing delayed diseases remains very high. Among the most common complications are:
- Chronic renal failure.
- Cardiac ischemia.
- Various lung diseases.
- Blockade of the cardiac pathways.
- Neurological disorders.
- Encephalopathy, etc.
Despite the development of methods of surgical treatment and systems for monitoring key indicators of the body during surgery, as well as approaches to postoperative patient management, the incidence of multiple organ failure continues to remain high. Due to the relevance of this problem, experts are looking for new ways to solve it, ranging from timely diagnosis to effective treatment.
| More information about treatment at Euroonco: | |
| Palliative care in Moscow | from 44300 per day |
| Emergency oncology care | from 12100 rub. |
Book a consultation 24 hours a day
+7+7+78
Prevention and prognosis
Preventing the body's stress response is a very real task. This requires timely diagnosis to avoid any existing disease from becoming critical. To implement such a preventive scheme, monitoring and functional assessment, normalization of blood circulation, elimination of infections, normalization of breathing and metabolism, provision of energy expenditure (nutrition), as well as early treatment of injuries, inflammation and necrosis are necessary.
The prognosis for the development of multiple organ failure depends on the severity and nature of the accompanying complications. When three or more organs and systems are affected, the patient’s death occurs in 70% of cases. When the function of two organs is impaired for more than a day, death occurs in 55% of patients. When one organ is affected - in 35% of cases.