September 14, 2020
Menopause occurs not only in women, but also in men. It’s just that women have a clear indicator of the cessation of reproductive function and the transition to a new stage of life - the cessation of menstruation, while in men there are no clear boundaries for the onset of andropause. But at the same time, many men experience a whole range of symptoms indicating that the body is undergoing age-related transformations.
At what age does male menopause occur?
After 30 years, every year a man's testosterone level decreases by about a percentage. The decline of sexual function and a decrease in the production of sex hormones occurs on average at the age of 50 years. But it is worth saying that this is a very conditional value, because much depends on the initial level of testosterone in youth and on lifestyle. The enemy of men's health is excess weight. Testosterone levels in obese men are significantly lower than those who maintain a normal body weight. Therefore, for some, a decrease in sexual function may occur long before the age of fifty, while for others it may occur much later. But a decrease in testosterone also provokes weight gain - a kind of vicious circle arises.
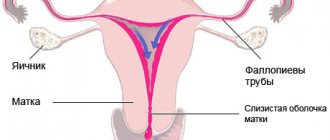
How does andropause affect the reproductive system?
A decrease in testosterone levels primarily affects the reproductive system:
- Decreased libido. Testosterone is the driving force of sexual desire. If the level of this hormone drops, then the desire for intimacy also fades away.
- Weakening of erection. Low testosterone levels lead to decreased blood supply to the male reproductive organ.
- Testicular atrophy. The testicles decrease in size, lose their ability to contract, and the process of sperm production is disrupted.
- Deterioration in sperm quality. A decrease in the concentration of the hormone leads to a decrease in sperm volume and quality, and the number and motility of sperm decreases.
The result of this is depression, loss of strength, and problems with fertility, that is, the ability to conceive a child.
Behavior of a man during menopause
Age-related androgen deficiency in a man can manifest itself as a complex of physical symptoms:
- decreased libido;
- erectile dysfunction;
- problems with the prostate - adenoma or prostatitis;
- changes in blood pressure;
- increased fatigue, loss of muscle mass.
Not all men notice physical changes. But for many, a decrease in the production of sex hormones affects behavior and emotional well-being:
- mood swings, depression, depression, bad mood, emotional fatigue and apathy, insomnia may be observed;
- vegetative-vascular disorders - changes in blood pressure, sweating, dizziness, hot flashes;
- some men become irritable and aggressive, behave demonstratively, and quarrel with loved ones.
Menopause is a natural, but not the easiest period in a man’s life. During adolescence, a hormonal storm affects the behavior of adolescents, the same thing happens when sexual functions begin to fade. Following internal changes come external ones. A man may worry about approaching old age and feel a decrease in sexual function. Psychological problems can be aggravated by erectile dysfunction. Because of this, a man can behave unusually and aggressively. Some become too active - they begin to dress brightly, engage in extreme sports, go to clubs and change sexual partners - this is how the fear of old age and the desire to prolong youth manifest themselves.
Treatment of menopause in men
Andropause in men is not a disease, but is used to describe the age-related symptoms listed above. It is often the case that symptoms are caused by physical, life or psychological problems.
- Stressful situations at work, financial problems - all this reduces libido and causes problems with sleep;
- Excessive drinking and lack of exercise can make you feel lethargic and reduce muscle mass;
- Lack of understanding and quarrels in the family provoke depression.
What methods of treating menopause in men do doctors use?
If you are experiencing several of the symptoms described above, make an appointment with your doctor so that he can find out what may be causing the problem.
Discuss the symptoms with your doctor, tell us when possible signs of menopause began, and in addition, the doctor will prescribe an examination in the form of hormone tests and a general blood test. Based on their findings, your doctor will be able to recommend a number of different treatments. Some treatment options include making lifestyle changes such as eating better, exercising, giving up alcohol and smoking, or prescribing cognitive behavioral therapy or taking medications.
Treatment will depend on what symptoms you have and what is causing them. In any case, treatment should be preceded by a thorough diagnosis, taking into account the results of appropriate blood tests, symptoms, medical history, lifestyle and physical examination, as well as screening for prostate cancer.
Ask a Question. Make an appointment by phone
8 (843) 207-18-00
How to relieve menopause symptoms
A healthy lifestyle, balanced nutrition, taking vitamins and physical activity will help smooth out the symptoms of menopause and improve your emotional background. Regular sex life will help maintain prostate health. But if the symptoms of menopause worsen a man's quality of life, he may be advised to take testosterone.
If you want to preserve your men's health for as long as possible, contact Dr. AkNer, here you will be given a high-quality examination and all existing problems will be identified.
Urologist, andrologist Akopyan Nerses Grigorievich.
Back to list of articles
What to do during male menopause
The first thing a man should do when experiencing symptoms of menopause is not to panic. A healthy lifestyle, multivitamin supplements, and hormonal therapy will help you stay active and courageous for a very long time. The main thing is to seek advice from an anti-age therapist, who will prescribe a comprehensive treatment - from cleansing the body to filling it with missing substances using special droppers. The ANACOSMA clinic prescribes individual rejuvenation programs for male menopause, which allow you to restore the body, restore vigor and virility.
Causes of physical inactivity
Testosterone is the main sex hormone associated with the functioning of all organs and systems. It affects not only sexual function, but also cognitive function, libido, metabolism of fats and carbohydrates, the immune system, hematopoiesis, and the density of fat, bone and muscle tissue. Hypodynamism refers to a drop in testosterone levels below normal, the signs of which become more noticeable with age. However, some men experience problems with potency by the age of 40, while others can boast of an active sex life even at 70. The fact is that everyone has their own timing of menopause. Men whose testosterone levels were initially higher develop androgen deficiency later than those who have this sex hormone within the average range. There are a number of factors that can accelerate the onset of andropause in men:
- constant stress;
- bad habits;
- long-term use of medications;
- the presence of certain diseases, such as diabetes, obesity, arterial hypertension, etc.
Folk remedies
Male menopausal syndrome can be corrected using herbal remedies. To relax and eliminate insomnia, andrologists recommend taking baths with extracts of valerian and pine needles before bed.
This is important : among the stronger sex, who are faced with menopause, there is an opinion about the magical properties of tincture of ginseng and leuzea. They say they improve potency, restore male strength and confidence, and comprehensively rejuvenate the body. These antioxidant biostimulants are good as adjuncts. But excessive consumption of ginseng tincture provokes hypertension.
To safely improve a man’s well-being during menopause, nutritionists recommend reviewing the diet. Include more walnuts, honey, and celery in your daily menu. Taking pollen, royal jelly and beebread has a positive effect on hormonal levels and general well-being. These substances contain many antioxidants, vitamins and phytohormones, which have properties similar to male sex hormones.
Male menopause is not a verdict. This is another natural period that should be experienced calmly and easily with the help of the right diet and an optimistic attitude.
Diagnosis of male menopause
It is easy to detect testosterone levels - just take a blood test for testosterone. If the deviations are not large, you don’t have to worry and continue monitoring your health. With a further decrease in hormone levels, the urologist will prescribe simple treatment.
As a rule of thumb, the biggest barrier to treating male menopause may be talking to your doctor about your symptoms. The doctor should ask too intimate questions regarding his personal life, which many men are embarrassed to answer.
Symptoms
Sexual dysfunction:
- decreased libido (sexual desire);
- orgasm disorders;
- deterioration of erection;
- decreased fertility (ability to fertilize);
- ejaculation disorders.
Somatic disorders:
- urinary disorders;
- loss of vitality, physical exhaustion;
- increase in adipose tissue;
- decreased muscle mass and strength;
- pain in the joints and lower back, decreased bone density.
Psycho-emotional disorders:
- sleep problems;
- decreased performance;
- irritability (despondency, negative reaction over trifles, aggressiveness);
- decreased attention and memory;
- increased fatigue and need for sleep;
- nervousness (restlessness, fussiness, internal tension), anxiety, depression.
Treatment of androgen deficiency
An individual treatment strategy is developed for each patient depending on the characteristics of his condition. As a rule, two main methods are used to correct the state of androgen deficiency:
Hormone replacement therapy. It is aimed at replenishing the lack of testosterone, increasing potency, and eliminating unpleasant symptoms. Stimulant therapy. Its goal is to push the body to produce its own testosterone.
The medical clinic employs experienced doctors who will help solve the problem of premature andropause, eliminate its symptoms and enable a man to feel full. A personal correction scheme will be developed for the patient, taking into account all the characteristics of his body and general condition.
Urologist in Lipetsk: +7 (4742) 90-40-50, and you can also make an appointment online
The difference between traditional and biomedicine approaches
When various symptoms occur (decreased sexual desire, fat deposition in the abdominal area, high blood pressure and the development of other cardiovascular diseases), men turn to different specialists, each of whom makes a separate diagnosis - from hypertension to prostatitis. From each doctor the patient receives his own recommendations and a specific set of pills. Unfortunately, this approach can lead to dire consequences.
Traditional medicine in the treatment of men, as they say, “hits the tails”: sleeping pills, blood pressure medications, genital blood circulation and potency stimulants are prescribed.
For example, beta blocker drugs designed to lower blood pressure lead to an even greater drop in testosterone levels, worsen the condition of the prostate gland, promote obesity, increase cholesterol and destroy blood vessels. For its part, reduced testosterone provokes the further development of hypertension - this closes the circle.
To compensate for all these side effects, the patient is additionally prescribed testosterone hormones. As a result, a man becomes dependent on drugs for the rest of his life, while the risks of developing atherosclerosis, fatty liver, strokes and heart attacks, obesity and oncology remain.
Bioreparative medicine, first of all, suggests eliminating the oxidation of lipids and proteins, starting cell regeneration and restoring adrenal function. That is, create conditions under which the body regulates itself and begins to produce more testosterone. And a normal level of testosterone will automatically lower cholesterol, cleanse the liver of fat, restore potency and libido, improve sleep and mood, and relieve chronic fatigue and irritability. And the most important thing is that at the end of the recovery program, the man will no longer be dependent on taking any pills. Now he will be able to withstand great physical and mental stress, be active, play sports, and feel like a leader again.
Reasons for the onset of andropause:
- taking certain medications (for example, prednisone or anabolic steroids);
- tissue injuries (including surgery) and previous diseases (infectious, fungal, parasitic);
- prolonged stress can completely stop testosterone production;
- Lack of necessary physical activity and irregular sex life can greatly slow down the production of hormones.
Andropause can be successfully treated, and most symptoms can be corrected to improve the patient’s quality of life. However, it is possible to cope with this condition only under the supervision of a professional andrologist. It is important to pay attention to the symptoms of the disease as early as possible and begin treatment for the disease immediately.
Diagnostics at Expert Clinics
At Expert Clinics in Moscow, we begin the program for restoring men's health with diagnostics, solving the problem with which the man came. For example, his libido decreases, his erection decreases, and he also complains of depressed mood and depression.
First of all, such a patient undergoes a full check-up of the body and undergoes tests. First, saliva and urine are collected to study hormone metabolites.
This way, the clinic’s doctors can understand which chain hormones are broken down and assess the state of hormonal function. Not only sex hormones - testosterone, progesterone and estrogen - but also adrenal and thyroid hormones. Metabolites of hormones, which are often more active than the hormones themselves, should also be assessed.
It is also very important to evaluate the first and second phases of detox in a man in order to understand whether any breakdowns have occurred in the detoxification processes, and what exactly is not removed from the body.
Adipose tissue is of enormous importance for men's health. And today there are also opportunities to evaluate markers of metabolic activity of adipose tissue.
Adipose tissue is a substrate for keeping blood vessels and nerves in good shape, and for inhibiting brain aging, because the brain is a fat-containing organ. And if some patients need to increase their fat layer, then others, due to individual indicators, are recommended to be as thin as possible and not accumulate fat.
Also, much attention is paid to the condition and volume of muscle mass. It is extremely important for representatives of the stronger sex to have a good muscular frame. When a man plays sports, muscles produce growth factor, which stimulates good tissue repair and regeneration.
If a reduction in muscle mass has begun, this is an alarming sign, especially when muscles are replaced by fatty tissue. Indeed, as a result, metabolism is distorted, which leads to rapid aging, deterioration of brain function, memory and vision, and apathy.
Also, much attention in diagnostics at Expert Clinics is paid to intestinal function; for this purpose, a genetic analysis of stool for microbiota is performed. The intestine, as one of the immunocompetent organs, affects immunity, detox and absorption of nutrients. Therefore, it is so important to restore the intestinal microflora.
Diagnosis of men's health may also include testing for the presence of heavy metals and other toxic components that inhibit tissue regeneration and repair. The condition of the membrane walls, on which the ability to obtain nutrients depends, is also assessed. To do this, a drop of blood is taken from each earlobe.
Hormone therapy for men
It is much easier to regulate the hormonal status of the male body than the female body, and this is good news for representatives of the stronger half of humanity. However, while women have long been accustomed to the idea that they need maintenance therapy during the premenopausal period, men are extremely wary of such an idea.
At Expert Clinics, we pay special attention to treating men and have developed the most comfortable methods for them. We prescribe strictly individually selected medications to patients, containing hormones in very small dosages.
Our advantage is that we adhere to the French school of endocrinology and work in accordance with biological circadian rhythms. That is, we take into account the hormone release curve: which of them are released in the evening and which in the morning. The drug intake program is developed individually for each man, and during the process of hormonal therapy, we make sure to study the dynamics of the metabolites that are produced when these hormones are broken down.
After leveling out the production of hormones, complete oncoprotection (protection against cancer) is launched, and the man’s prostate gland stops enlarging.
And soon after the start of therapy, the man notices that his erection, libido, and sexual function have been restored, which is also extremely important for self-esteem. Men regain confidence, sleep is restored - and a whole new world opens up for them.
Andropause: age-related decline in sex hormone levels in men
I.I. Buziashvili, G.A. Melnichenko
Department of Endocrinology, Moscow Medical Academy named after. THEM. Sechenov
Currently, the study of various issues related to aging occupies one of the leading places in modern medicine. First of all, this is due to significant demographic changes that have occurred in society over the last century - an increase in people's life expectancy, as well as an increase in the number of elderly people. It is noted that compared to 1900, the number of men in the world over the age of 65 has increased by 7 times, and those over the age of 85 by 31 times. In this regard, the exceptional relevance of issues related to health, as well as the quality of life of elderly and senile people, becomes clear.
Changes in the male reproductive system with aging
Traditionally, human aging is associated with a decrease in the reproductive function of the body. In middle-aged women, the onset of menopause characterizes the end of the reproductive period, and a decrease in the level of sex hormones leads to the appearance of various postmenopausal disorders: vegetative-vascular and mental reactions, urogenital disorders, as well as an increased risk of developing cardiovascular diseases and decreased bone density. Recently, great strides have been made in the treatment and prevention of postmenopausal disorders, which can significantly reduce the incidence of cardiovascular diseases and osteoporosis, as well as improve the quality of life of women of the same age.
Unlike women, men do not experience an abrupt end to their reproductive function. However, it is now generally accepted that in men there is a gradual decline in the level of sex hormones (primarily testosterone), which begins at the age of 30-40 years. By analogy with the cessation of menstruation in women - menopause - the term "andropause" was introduced to refer to the decrease in the level of sex hormones in men. Many authors reject this term due to the discrepancy between the phenomena that occur with age in the female and male body. In this regard, the term “partial androgen deficiency in older men” (PAMD) was proposed. In this article, we will use the term “andropause” to refer not only to the age-related decrease in the level of sex hormones, but also to the clinical manifestations of androgen deficiency in old age.
It is noted that after 30-40 years, testosterone levels decrease by about 1-2% per year. In men aged 80, testosterone levels average about 40% of the normal hormone levels for a 25-year-old man. In addition, the level of testosterone varies among different people of the same age and depends on many factors - lifestyle, the presence of concomitant diseases, bad habits, genetic and constitutional characteristics. Typically, in the presence of chronic concomitant diseases (diabetes mellitus, arterial hypertension, coronary heart disease), testosterone levels are 10-15% lower than in healthy people of the same age, while the rate of decline in testosterone levels in them does not differ from that in a healthy population.
The decline in testosterone levels with age is due to a number of factors. It has been shown that in elderly men the release of testosterone is reduced in response to the administration of human chorionic gonadotropin, which indicates the primacy of damage to the function of Leydig cells. This is due both to a decrease in the number of Leydig cells due to the blood supply to the testicular tissue, and to a decrease in receptors for luteinizing hormone (LH) on their surface. However, in contrast to primary hypogonadism in young individuals, LH secretion is often not increased and is within normal limits, which indicates a violation of negative feedback mechanisms in older individuals. Functional disorders in the secretion of gonadotropin-releasing hormone and gonadotropins also play a role in reducing testosterone levels.
The main amount (more than 98%) of testosterone circulates in plasma in a bound state: up to 58-60% in connection with albumin, about 40% in connection with sex hormone binding globulin (SHBG, testosterone-estradiol-binding globulin), and only about 1-2% of testosterone is in unbound, free form. It is believed that the biologically active, or "bioavailable" fraction of testosterone is the freely circulating fraction, and the portion of the hormone that is weakly bound to albumin, while the portion of testosterone bound to SHBG does not exhibit its biological activity. It has been proven that with aging there is an increase in the level of SHBG and, accordingly, the amount of testosterone associated with it. Thus, with age, the level of biologically active testosterone decreases to a greater extent than the level of total testosterone. It has been found that 50% of men aged 50-70 years have levels of bioavailable testosterone below the normal level of the hormone for men aged 20-40 years.
In a healthy person, testosterone secretion has a pronounced circadian rhythm with maximum levels of the hormone in the early morning hours, and minimum levels at 15:00-17:00. With age, in many men, the daily rhythm of testosterone secretion is erased or not expressed at all. However, most authors recommend measuring testosterone levels in the early morning hours in both young and elderly individuals.
For many men, estrogen levels increase with age, which leads to changes in the androgen/estrogens ratio in the body and the appearance of symptoms specific to this (for example, gynecomastia). Apparently, relative hyperestrogenism in old age is associated with increased aromatization of androgens in extragonadal tissue. In turn, suppression of the secretion of gonadotropins by extraglandularly formed estrogens through a negative feedback mechanism can lead to an additional decrease in testosterone synthesis in the testes.
Many authors have noted changes in the spermatogenic function of the testicles with age. In men over 60 years of age, the volume of ejaculate is often reduced, as well as the number of sperm with normal morphology and motility. A decrease in spermatogenesis in older individuals is also evidenced by a decreased number of Sertoli cells, as well as a decreased level of inhibin and an increased level of follicle-stimulating hormone (FSH).
Manifestations of age-related decrease in androgen levels
The intensity of the above-described changes in steroidogenesis and spermatogenesis during aging is subject to significant individual fluctuations. However, many men over the age of 50-60 years experience symptoms characteristic of the clinical picture of hypogonadism. These include:
A. Genitourinary disorders:
- decreased libido
- erectile disfunction
- orgasm disorders
- decreased ejaculate fertility
- pollakiuria (unrelated to benign prostatic hyperplasia)
B. Vegetovascular disorders:
- sudden hyperemia of the face, neck, upper body
- feeling of heat (“hot flashes”)
- fluctuations in blood pressure levels
- cardialgia
- dizziness
- feeling of lack of air
B. Psycho-emotional disorders:
- increased irritability
- fast fatiguability
- weakening of memory and attention
- insomnia
- depressive states
- decreased general well-being and performance
D. Somatic disorders:
- decrease in muscle mass and strength
- decreased bone density
- gynecomastia
- the appearance or increase in the severity of visceral obesity
- reduction in the amount of androgen-dependent hair
- thinning and atrophy of the skin
D. Laboratory changes:
- decreased levels of total and bioavailable testosterone
- increased levels of estradiol and sex hormone binding globulin
- anemia of varying severity
- increased levels of low-density lipoproteins (LDL) and very low-density lipoproteins (VLDL).
It should be noted that quite often the intensity of the described symptoms does not correlate with the level of plasma androgens. However, the important role of androgens in the development of these symptoms is confirmed by the elimination or significant reduction in the severity of many of these symptoms when androgen replacement therapy is started. Evidence of the complex relationship between the level of sex hormones and the symptoms of hypogonadism can also be the frequent detection of normal levels of estrogen and gonadotropins in women with severe postmenopausal disorders.
Diagnosis of andropause
According to most authors, when diagnosing andropause, a practitioner should focus primarily on the presence or absence of the symptoms listed above. To simplify screening, special screening tests are often used to ensure that men are more likely to be identified for further examination and treatment.
An important step in diagnosing andropause is determining the level of testosterone in the blood plasma. Most authors recommend determining the level of total testosterone at 8:00-9:00, i.e. during the maximum concentration of the hormone during the day. Depending on the method used to determine testosterone levels, normal levels of testosterone in the blood may vary. However, in most cases, a testosterone level of less than 12 nmol/l is regarded as a clear sign of hypogonadism and is an indication for all further diagnostic steps. According to foreign authors, testosterone levels from 7 to 12 nmol/l are considered borderline between normal and pathological. The tactics of the diagnostic process in this case are determined by the presence or absence of clinical manifestations of andropause.
If testosterone levels characteristic of male hypogonadism are detected, it is necessary to determine the levels of gonadotropins and prolactin. Due to the fact that the secretion of gonadotropins occurs in a pulsed mode, only double determination of LH and FSH levels with an interval of 15-20 minutes is considered reliable. The detection of increased levels of gonadotropins most likely indicates the primary changes in the testicles, i.e. for hypergonadotropic hypogonadism. As already mentioned, a common finding in elderly people is eugonadotropic hypogonadism, caused by impaired feedback functioning. Sometimes, when examining elderly people, a reduced level of gonadotropins in the blood is detected, which also indicates a violation of the negative feedback mechanism in the hypothalamic-pituitary-testicular system with age, and less often - the presence of secondary hypogonadism. In this regard, when diagnosing andropause, the clinical picture and the level of testosterone in the blood plasma are of paramount importance, and determination of the level of gonadotropins and prolactin is auxiliary, with the goal of excluding the pituitary origin of hypogonadism. It is preferable to determine the level of prolactin in plasma using modern laboratory methods to exclude cross-reaction of prolactin with macroprolactin, a biologically inactive form of prolactin.
Some authors recommend determining the level of bioavailable testosterone at a borderline (7-12 nmol/l) value of total testosterone and normal levels of gonadotropins and prolactin. It is advisable to re-determine the level of total or bioavailable testosterone if normal results are obtained in the first study and clinical symptoms of andropause are present.
Differential diagnosis of age-related decrease in testosterone levels in men should be carried out with the most common diseases leading to the development of hypogonadism in the postpubertal period. Both endo- and exocrine functions of the testicles can be affected by various systemic diseases (see Table 1), as well as taking medications (see Table 2).
Table 1. The most common somatic diseases accompanied by reproductive disorders in men
| Disease | Clinical and laboratory manifestations |
| Liver diseases | Gynecomastia, decreased secondary hair growth, decreased libido, ED and other symptoms of hypogonadism; decrease in T level, increase in LH, FSH, SHBG, E2 levels; spermatogenesis disorder |
| Hemochromatosis | Typical clinical picture of hypogonadism; decreased levels of T, LH, FSH, normal spermatogenesis |
| Chronic anemia | Reduced levels of T, LH, FSH |
| Chronic renal failure | The clinical picture of hypogonadism can be moderate; decreased T level, increased LH, FSH levels |
| Spinal cord diseases | Sometimes - gynecomastia; ejaculation disorder, ED; normal levels of T, LH, FSH, E2; oligo-, azoospermia, necrospermia |
| Thyrotoxicosis | Decreased libido, ED, gynecomastia; increased levels of total T, SHBG, E2, LH, FSH, decreased levels of free T |
| Hypothyroidism | Decreased libido, ED; decreased level of T, SHBG; often - increased levels of PRL |
| Cushing's syndrome | Gynecomastia, decreased libido, ED; decreased levels of T, E2, LH, FSH, SHBG; spermatogenesis disorder |
| Diabetes | ED, normal libido (in most cases); decreased levels of T, SHBG, LH, FSH |
| Obesity | Gynecomastia, decreased libido, ED; decreased level of T, SHBG, increased level of E2, normal or decreased level of LH, FSH |
| HIV infection | Gynecomastia, decreased libido; decreased levels of T, LH, FSH; spermatogenesis disorder |
| Malignant tumors | Reduced T level, increased SHBG, PRL; impaired spermatogenesis (oligospermia) |
| Extreme conditions, stress | Reduced levels of T, LH, FSH, impaired spermatogenesis |
Abbreviations: T - testosterone, E2 - estradiol, LH - luteinizing hormone, FSH - follicle stimulating hormone, PRL - prolactin, SHBG - sex hormone binding globulin, ED - erectile dysfunction.
Table 2. Some drugs that cause reproductive system disorders in men
| Androgens* | Antiepileptic drugs |
| Anabolic steroid | Sleeping pills |
| Estrogens | H2 receptor antagonists |
| GnRH agonists and antagonists | Neuroleptics |
| Glucocorticoids* | Antidepressants |
| Thyroid hormone preparations* | Dopamine antagonists |
| Antiandrogen drugs | Antitumor drugs |
| 5a reductase inhibitors | a - and b - adrenergic blockers |
| Steroidogenesis blockers | Anti-tuberculosis drugs |
| Lipid-lowering drugs | Narcotic drugs |
* - in doses significantly higher than physiological
If hyperprolactinemia is detected, as well as significantly reduced levels of gonadotropins, imaging of the sella turcica is recommended. Magnetic resonance imaging (MRI) is preferable due to its greater resolution and safety during the study. It must be borne in mind that, in comparison with the reduced level of androgens, the presence of a pituitary adenoma is a rather rare pathology in older men.
Treatment of andropause
For a long time, the possibility of androgen replacement therapy in older men was not discussed among doctors due to the widespread belief that the changes that occur with age in the male body are “physiological.” This was partly due to the negative consequences of the use of the first synthetic testosterone derivatives alkylated at the C17 position (methyltestosterone, fluoxymesterolone and others). These drugs had serious side effects in the form of toxic and carcinogenic effects on the liver, as well as a negative effect on the lipid spectrum of the blood (a sharp increase in the level of atherogenic and a decrease in the level of anti-atherogenic lipoproteins). Moreover, some of these drugs were not converted in the body into the active testosterone metabolites 5a-dihydrotestosterone (5a-DHT) and 17b-estradiol (E2), and thus did not provide the full range of therapeutic effects of natural testosterone. In this regard, the use of C17-alkylated testosterone derivatives in clinical practice was discontinued.
Currently, the main drugs used for androgen replacement therapy in men are drugs based on the unmodified testosterone molecule (see below).
1. Treatment goals. The effectiveness of the therapy.
According to most authors, the effectiveness of androgen replacement therapy should be assessed primarily by the dynamics of the clinical manifestations of andropause. In most cases, the effectiveness of therapy in clinical practice is assessed according to subjective criteria. Indicators of the effectiveness of testosterone therapy and at the same time the goals of the treatment are:
- increased libido and overall sexual satisfaction;
- reduction in severity or disappearance of vegetative-vascular and mental disorders;
- with long-term treatment (more than 1 year) - increased bone mass density, decreased severity of visceral obesity, increased muscle mass;
- laboratory parameters: increased hemoglobin level or red blood cell count, decreased VLDL and LDL levels with unchanged HDL levels.
Despite the frequent positive effects of androgen replacement therapy, improvement of erectile function should not be considered a goal of treatment due to its greater dependence on the state of the peripheral nervous system and blood vessels of the genital organs. Gynecomastia, which develops as a result of a change in the ratio of androgen to estrogen levels, is rarely eliminated using conservative treatment methods.
2. Drugs for androgen replacement therapy
As already mentioned, the main drugs for androgen replacement therapy in men are natural testosterone preparations. To date, drugs have been created for oral, injection and transdermal use.
Currently, C17-alkylated testosterone preparations (methyltestosterone), which have a pronounced toxic and carcinogenic effect on the liver when administered orally, have been practically withdrawn from use.
The drugs of choice are drugs based on unmodified (natural) testosterone molecules, most often testosterone esters. When taken orally, crystalline testosterone does not have therapeutic activity due to almost complete inactivation during the first passage through the liver. In contrast, its ester is testosterone undecanoate ( Andriol
, "Organon", the Netherlands) - does not undergo primary hepatic metabolism, as it is absorbed into the lymphatic system, bypassing the liver. After hydrolysis of testosterone undecanoate in the lymphatic system, testosterone enters the systemic circulation, which has a therapeutic effect both on its own and through its main metabolites - 5a-DHT and E2, which determine the full spectrum of androgenic activity of testosterone. Thus, ANDRIOL retains its activity when administered orally. At the same time, bypassing the portal vein system and passing through the liver, testosterone undecanoate does not have any hepatotoxic or hepatocarcinogenic effects. Thus, today ANDRIOL is the only drug based on an unmodified (natural) testosterone molecule that is effective when taken orally.
The half-life of the drug from plasma is 3-4 hours. In this regard, the dosage regimen for testosterone undecanoate is 2 times a day. The dose of the drug is selected individually, usually 80-120-160 mg per day (2-4 capsules of 40 mg each).
One of the first drugs for injection use were testosterone esters - testosterone enanthate and testosterone cypionate. When these drugs are administered intramuscularly, a depot is created from which the drug is released into the bloodstream. During the first 2-3 days after administration, testosterone levels rise to supraphysiological levels, and then slowly decrease over the next 2 weeks to subnormal values. The positive side of these drugs is the duration of the therapeutic effect. However, sudden changes in testosterone levels, often felt by the patient himself in the form of increases and decreases in libido, general well-being, and emotional status, are undesirable negative qualities of these drugs. Testosterone enanthate and testosterone cypionate are the most common testosterone preparations in the United States.
Sustanon 250 is most widespread.
(Organon, Netherlands). It is a combination of 4 testosterone esters (testosterone propionate, phenylpropionate, isocaproate and decanoate). Due to the fact that these testosterone esters have different pharmacokinetic properties (different absorption rates and duration of effect), the effect of SUSTANON 250 begins immediately after injection and persists for the next three weeks. Thus, an adequate dosage regimen is intramuscular administration of the drug in a dose of 1 ml once every 3 weeks.
Recently, therapeutic systems for transdermal application of testosterone have been developed. There are 2 types of such therapeutic patch systems: for application to the skin of the scrotum or to the skin of open parts of the torso. Due to the need to add substances that increase the absorption of testosterone through the extrascrotal skin, the use of the drug is often complicated by the appearance of side symptoms such as itching and redness at the site of application of the patch. Thus, the difficult route of administration, the frequent occurrence of these side effects, as well as the relatively high cost limit the widespread use of these drugs in clinical practice.
Previously, testosterone preparations were used in clinical practice for implantation into the subcutaneous fatty tissue. Due to the invasiveness of the method of application, these drugs are currently not used in clinical practice.
Currently, new testosterone drugs with new pharmacokinetic properties are being developed. Examples of such drugs are testosterone bucyclate, which has a long period of action (12-16 weeks), and testosterone associated with cyclodextrin for sublingual use.
According to many authors, the use of the drug 5a-dihydrotestosterone (in the form of a gel applied to the skin) is not recommended, since this drug, due to the inability to convert into estradiol, does not have the full range of therapeutic properties of testosterone (for example, the effect on bone tissue).
Finally, dehydroepiandrosterone sulfate (DHEA-S) preparations may be a promising drug for androgen replacement therapy. It is known that the level of this adrenal androgen decreases starting from 20-25 years. Thus, at the age of 80-90 years, the level of DHEA-S does not exceed 20% of the level of the hormone characteristic of 20 years of age. Currently, a large amount of work is being done on the possibility of using DHEA-S preparations in clinical practice.
3. Treatment tactics. Treatment regimens.
The specific tactics and regimen of androgen replacement therapy are selected individually for each patient and depend on the clinical manifestations of andropause, the level of total or bioactive testosterone, as well as the goals of therapy and possible side effects. Reduced testosterone levels are a direct indication for androgen replacement therapy, regardless of the presence of clinical symptoms of andropause, which is associated with the long-term clinical course of some manifestations of hypogonadism (for example, osteopenia, visceral obesity). On the other hand, in the presence of andropause symptoms and normal testosterone levels, it is advisable to prescribe a trial 3-month course of androgen replacement therapy, followed by an assessment of the effectiveness of treatment and a decision on further tactics. As already mentioned, to achieve the positive effects of testosterone on the somatic manifestations of andropause, long-term (more than 1 year) treatment is necessary.
According to many authors, in old age it is advisable to avoid the use of drugs that create a “jumping” level of testosterone in the blood due to the possible side effects of supraphysiological levels of the hormone (see below) and negative subjective symptoms of a sharp change in the level of testosterone in the blood. On the other hand, it is desirable to use a drug with a convenient method of application. As a result, the most common drug for androgen replacement therapy in men with manifestations of andropause is testosterone undecanoate (ANDRIOL, Organon, the Netherlands). The following are the two most commonly proposed regimens for androgen replacement therapy in the elderly.
- The prescription of a replacement dose of the drug is 120-160 mg ANDRIOLA per day for 2-3 weeks, followed by transition to maintenance therapy - 40-120 mg ANDRIOLA per day.
- Prescription of a replacement dose of the drug for 3 months, followed by withdrawal for up to 3 months.
When using any of the treatment regimens, a patient taking a testosterone drug should be examined every 3 months to assess the effectiveness of the therapy, possible adjustment of the drug dose, and to identify side effects of therapy.
Contraindications and side effects of androgen replacement therapy
As already mentioned, currently C17-alkylated testosterone preparations, which have a pronounced toxic and carcinogenic effect on the liver, have been withdrawn from use.
One of the most pressing issues of androgen replacement therapy is the effect of exogenously administered androgens on the prostate gland. It is known that the removal of androgens from the body using chemical (continuous use of gonadotropin-releasing hormone agonists) or surgical castration causes a noticeable slowdown in the development of prostate cancer. The use of 5a reductase inhibitors is highly effective in benign prostatic hyperplasia (BPH). In this regard, it has been suggested that exogenous androgens may have a negative effect on the prostate gland. At the same time, it was noted that most often these diseases occur in old age, i.e. against the background of a decrease in androgen levels. Numerous molecular studies have shown that the main pathogenetic factor in the development of BPH is an intracellular increase in 5a-reductase activity, leading to an increase in the level of 5a-DHT in prostate cells, and not increased plasma testosterone levels. When using replacement doses of testosterone, there was no deterioration in urofluometry, as well as in the American Urological Association questionnaire for assessing symptoms of BPH. Thus, BPH is not considered to be a contraindication to androgen replacement therapy.
Many studies have reported no correlation between plasma testosterone levels and the incidence of prostate cancer. Similar findings were found in another study where prostate specific antigen (PSA, a marker of prostate cancer) levels were not affected by androgen replacement therapy in healthy men. Moreover, according to many authors, there is no reason to believe that exogenous administration of testosterone will lead to the transition of subclinical forms of cancer to clinically significant prostate cancer. However, proven prostate cancer is an absolute contraindication to androgen replacement therapy, and detection of cancer during treatment is an indication to interrupt treatment. According to most authors, an adequate method of screening for the presence of prostate cancer is a digital examination of the prostate gland, determination of PSA levels, and transrectal ultrasound examination of the prostate gland. Due to the fact that all patients receiving androgen replacement therapy undergo mandatory screening for prostate cancer at least 2 times a year, they have a high probability of detecting cancer in the early and, thus, curable stages.
Another absolute contraindication to treatment is breast cancer, but this issue is not discussed in the article due to the low prevalence of the disease in men.
As is known, when taking androgens, suppression of the endocrine function of the testicles and spermatogenesis is possible through a negative feedback mechanism. This effect is especially noticeable when taking injection drugs with a long half-life. At the same time, taking 240 mg of testosterone undecanoate (ANDRIOL) for 6 months was not accompanied by a decrease in the initial normal level of spermatogenesis. Other studies have also shown no significant suppression of normal levels of gonadotropins or endogenous testosterone with this drug, which is likely due to the short half-life of testosterone undecanoate.
Testosterone therapy often results in an increase in hematocrit above physiological values due to the constant stimulation of erythropoiesis (associated with increased production of erythropoietin under the influence of androgens). Most authors recommend reducing the dose of the drug when hematocrit levels reach above 51% and discontinuation of the drug when levels are more than 54%. It has been noted that older people often have a reaction in the form of a sharp increase in hematocrit when relatively small doses of testosterone are prescribed. A particularly pronounced increase in hematocrit levels during androgen replacement therapy occurs in patients with chronic pulmonary diseases. When the drug is discontinued, the hematocrit level usually returns to normal values.
A controversial issue is the effect of exogenous androgens on blood lipid levels. It is traditionally believed that the increased risk of developing atherosclerosis and coronary heart disease in men compared to women of reproductive age is associated with the negative effect of androgens on the lipid profile. However, several studies have shown that testosterone administration leads to a decrease in the levels of atherogenic VLDL and LDL, with relatively unchanged levels of antiatherogenic HDL. Another population-based study found that the risk of coronary heart disease decreased as plasma testosterone levels increased. This may be due to the positive effect of testosterone on the severity of visceral obesity.
An increase in the incidence of sleep apnea syndrome has been noted in patients taking testosterone replacement therapy. It is possible that this side effect occurs mainly in individuals with obesity or chronic lung disease.
Rare complications during androgen replacement therapy are fluid retention in the body, a physiological increase in appetite, and a tendency to thrombosis. Due to the latter side effect, careful use of testosterone is recommended for men with recent surgeries or injuries.
Table 3 shows a sample examination plan for assessing the effectiveness and side effects of androgen replacement therapy.
Table 3. Examination plan for assessing the effectiveness and side effects of androgen replacement therapy.
Questioning
— subjective assessment by the patient:
- psycho-emotional status
: general well-being, mood, degree of irritability, performance, quality of sleep - sexual function
(can be assessed using special questionnaires): libido, erectile function, general sexual satisfaction - autonomic symptoms
: sweating, hot flashes, palpitations, dizziness, shortness of breath - somatic status
: muscle mass and strength, amount of fatty tissue - side effects of therapy:
frequency, duration, difficulty urinating, nocturia; sleep apnea (snoring, holding your breath); increased blood pressure, urine output
Physical examination:
- assessment of the amount of muscle mass, adipose tissue (calculation of body mass index, ratio of waist to hip volume), degree of gynecomastia
- measurement of heart rate, blood pressure
- digital examination of the prostate gland; presence of peripheral edema
Laboratory and instrumental examination:
- complete blood count (red blood cell count, hemoglobin level, hematocrit)
- blood lipid spectrum (level of total cholesterol, triglycerides, VLDL, LDL, HDL)
- prostate specific antigen (PSA) level
- densitometry of the bones of the forearm, spine
- urofluometry / ultrasound examination of the prostate gland, targeted biopsy (if pathology is suspected)
IMPOTENCE Impotence Erectile dysfunction Erection Causes of impotence Psychological impotence Organic impotence Diagnosis of impotence Treatment of impotence Penile prosthetics Penile prosthetics
Where is male menopause treated in St. Petersburg, prices
Such conditions require a special approach, so it is better to be treated in a private clinic. For example, such services in St. Petersburg are offered by the specialized clinic Diana. An experienced urologist works here, you can take tests for hormones and infections, take a spermogram, undergo a comprehensive ultrasound and other diagnostics.
The cost of treatment and examination is low: an appointment with a Urologist will cost 1000 rubles, a comprehensive ultrasound of the pelvis on a new machine with Doppler will cost 1000 rubles, a consultation based on the results of the examination costs only 500 rubles.
Treatment of andropause
These symptoms can be relieved. The urologist recommends lifestyle changes, mild antidepressants, and hormonal therapy to replenish the missing testosterone.
First of all, of course, you will need to switch to a healthy lifestyle: you will have to switch to a normal diet, increase the number of walks, get enough sleep and be minimally nervous. If you cannot cope with depression, your doctor will prescribe relaxation medications.
The most effective way to treat male menopause is hormone replacement therapy. This technique is used in all European countries. Based on the test results, the doctor calculates the missing amount of testosterone and prescribes a synthetic analogue.
Before hormone replacement therapy, you need to undergo a number of additional tests and studies, since the technique has contraindications. In particular, testosterone is contraindicated in prostate cancer, as it causes cell growth and rapid replacement.
You will need to go through:
- Ultrasound of male organs - ultrasound of the prostate, ultrasound of the testicles;
- Ultrasound of the pelvis;
- Smear for infections;
- Blood test for tumor markers.